Abstract
Purpose
The aim of this study was to evaluate the pre-operative performance of an automated multiplex PCR (mPCR) system in patients with suspected periprosthetic joint infection (PJI).
Methods
Under sterile conditions, synovial fluid samples from patients with a suspected PJI were collected pre-operatively. One hundred eighty microliter of the aspirate was used for analysis in the mPCR. The remaining joint fluid was sent for microbiological analysis. PJI was diagnosed by using the Musculoskeletal Infection Society (MSIS) criteria. Total percentage agreement and Cohen’s kappa coefficient were calculated to measure overall agreement.
Results
Overall, 90 patients with a suspected PJI were included. Using MSIS criteria, 38 (42%) patients were classified as septic. Total percent agreement between mPCR and synovial fluid culture was 86% with a Cohen’s kappa of 0.68. The mPCR and synovial fluid culture showed sensitivities of 71% and 84%, respectively. Combined evaluation provided an even higher sensitivity of 92%. While Cutibacterium spp. were detected five times by mPCR, it could only be cultured once. A higher detection rate of CoNS by mPCR (n = 7) compared to conventional culture (n = 5) was also demonstrated. In comparison to synovial fluid culture, the mPCR missed Staphylococcus aureus five times.
Conclusion
With a moderate agreement between synovial fluid mPCR and culture, the mPCR system could be a useful adjunct in diagnosing a PJI pre-operatively. Due to faster availability of results and a higher detection rate of low-virulent microorganisms, it can complement conventional culture.
Similar content being viewed by others
Introduction
The pre-operative detection of the causative microorganism(s) and antimicrobial susceptibility is essential for ideal surgical and antibiotic treatment of periprosthetic joint infection (PJI). An accurate and prompt evaluation is crucial for treatment success. Currently, pre-operative-collected synovial fluid cultures represent the method of choice for diagnosing an infection and planning the optimal revision surgery (one-stage vs. two-stage). Results from conventional microbiological culture-based analyses should become available within one to 14 days [1]. If a PJI with low-virulence microorganisms is suspected, the cultures should be observed for 14 days or longer [1]. Treatment is adjusted according to the antibiogram. This time period in which treatment is considered is needed to choose the ideal operation procedure and to optimize antimicrobial therapy.
Currently, attention has been paid to polymerase chain reactions (PCR) for genotypic evaluation of bacteria. These techniques are verified methods in diagnosing infectious diseases in hospitalized patients. In the literature, multiplex PCR analysis of periprosthetic tissue or periprosthetic sonicate fluid samples has already been evaluated for diagnosing orthopaedic infections [2,3,4,5]. The great advantages of multiplex PCR systems are the short turnaround time and rapid identification within five to six hours of the most common clinically relevant pathogens and genetic markers of resistances.
The purpose of the current study was to investigate the pre-operative performance of the automated multiplex PCR Unyvero i60 ITI cartridge application (Curetis GmbH, Holzgerlingen, Germany) in patients with suspected periprosthetic joint infection under clinical conditions. We aimed to evaluate the detected pathogens and resistance marker in synovial fluid samples so as to compare the results with those of synovial fluid cultures. Furthermore, the merit of combining both diagnostic methods was determined.
Material and methods
Study design
This prospective cohort study was conducted in a tertiary healthcare centre. Synovial joint fluid samples were investigated by a specific commercial mPCR system and conventional culture. The study was approved by the institutional ethical review board of Medical University of Vienna and was done in accordance with Declaration of Helsinki.
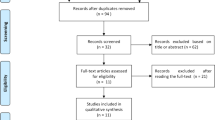
Study population
Between March 2016 and February 2018, 98 consecutive patients older than 18 years with a painful prosthesis and suspected periprosthetic joint infection were included. Exclusion criteria were invalid test results of the multiplex PCR system, obvious contamination of the joint fluid as well as contamination during transport to the laboratory, and an incomplete dataset. A periprosthetic joint infection was defined according to the Musculoskeletal Infection Society (MSIS) criteria [1].
Multiplex PCR evaluation
In the context of routine clinical pre-operative diagnosis of a painful periprosthetic joint, a needle aspiration of the affected joint was performed under sterile conditions in the outpatient facility before revision surgery. One hundred eighty microliter of the collected synovial fluid was used for microbial analysis using the multiplex PCR Unyvero i60 ITI application (Curetis GmbH, Holzgerlingen, Germany), which covers more than 100 pathogens and resistance markers. The remaining joint fluid was sent for conventional microbiological analysis.
The Unyvero i60 ITI application is a semiquantitative DNA test capable of parallelly performing eight multiplex PCR reactions to detect the nucleic acid of specific pathogens commonly found in PJI. It further can provide information about antibiotic resistance genes.
All specimens were processed with the Unyvero i60 ITI application according to the manufacturer’s protocol as previously described [6]. All performed tests were purchased by our department. A sample was seen to be positive if at least one of the analytes (pathogens) reached the threshold of 104 DNA fragments/pathogen/ml. The detection threshold for the antibiotic resistance analytes was determined with serial dilutions of living bacteria or dilutions of DNA fragments in the buffer by the manufacturer. The resistance markers aacA4, ctx-M, ermA, mecA, ndm, oxa-23, oxa-48, oxa-58, and vanA were detected at a concentration of 104 DNA fragments/pathogens/ml; aac(6′)/aph(2″), gyrA, imp, kpc, oxa-24, and vim were identified at a concentration of 105 DNA fragments/pathogens/ml; and ermC, mecC, rpoB, and vanB were detected at a concentration of 106 DNA fragments/pathogens/ml.
Routine cultivation of synovial fluid
Synovial fluid (SF) was inoculated onto the following media: Columbia agar III with 5% sheep blood and chocolate agar with IsoVitaleX and bacitracin (BD, Heidelberg, Germany). Both media were incubated in a carbon dioxide-enriched atmosphere for up to 14 days. McConkey agar No. 3 (Oxoid, Basingstoke, UK) was incubated for 48 hours at aerobic conditions. Brucella Blood agar with Hemin and vitamin K1 and Schaedler kanamycin-vancomycin with 5% sheep blood (BD, Heidelberg, Germany) were incubated under anaerobic conditions for up to 14 days. Additionally, an in-house-prepared brain heart infusion with 0.1% agar was also inoculated and incubated for up to 14 days. All media were incubated at 35–37 °C. Susceptibility testing was performed using the EUCAST disc diffusion method and interpreted according to the EUCAST clinical breakpoints for bacteria v 5.0.
Diagnostic tests
Serum CRP-levels were determined pre-operatively. In line with proceedings of the International Consensus Meeting [1], a cutoff of 10 mg/l was maintained. If the cutoff was exceeded, the minor criterion “serum CRP-level” was classified as positive. To evaluate the leukocyte count, a minimum of 1 ml synovial fluid was analyzed in an automatic manner. During surgery (if performed), at least three periprosthetic tissue samples were sent for microbiological analysis as mentioned above.
Statistical analysis
Positive and negative percent agreement between conventional culture and the multiplex PCR system was calculated as the number of concordant positive (negative) observations divided by the number of positive (negative) results of conventional culture. Total percentage agreement and Cohen’s kappa coefficient were calculated to measure overall agreement. Sensitivity, specificity, positive (LR+) and negative likelihood ratio (LR−), area under the ROC curve (AUC), positive (PPV) and negative predictive value (NPV) of mPCR, conventional culture, and the combination of both diagnostic methods were calculated, and individual receiver operating characteristic (ROC) curves were drawn for each test. All estimated parameters are reported with 95% confidence intervals. The software XLSTATPM (version 2017; XLSTAT; Addinsoft, New York, NY, USA) was used to perform the statistical analysis.
Results
Demographics and infection classification
Eight patients had to be excluded because of incomplete data. Ninety patients (47 female, 43 male) with a suspected periprosthetic joint infection were eligible for inclusion. The median age was 72 (range, 25–88) years. Fifty-one (57%) patients had a suspected infection after a total knee arthroplasty (TKA), 33 (37%) after a total hip arthroplasty (THA), four (4%) after a total shoulder prosthesis, one (1%) after a total upper ankle joint prosthesis, and one (1%) after a total elbow prosthesis. Twenty-six (29%) patients received antibiotics before aspiration.
Thirty-eight patients (42%) out of the 90 cases with suspected PJI were classified as septic according to the MSIS criteria. Of these 38 patients, at least one microorganism was detected in 27 synovial fluid samples by mPCR and in 32 synovial fluid specimens by SF culture (Fisher’s exact test; p = 0.271).
Performance of the multiplex PCR system
Overall, 34 microorganisms out of 29 synovial fluid samples could be detected in the mPCR system. In the conventional culture, 34 microorganisms out of 32 synovial fluid sample cases showed microbial growth. Overall percent agreement between mPCR and SF culture was 85.6% (95% CI, 78.3–92.8%). A Cohen’s kappa of 0.68 (0.52–0.84) indicated moderate agreement between mPCR and conventional culture of the SF. We calculated the positive and negative percent agreement in all cases. Furthermore, we separated the cohort in subgroups and calculated the overall percent agreement in patients after a THA and TKA, as shown in Table 1. A slightly higher overall agreement in patients after a TKA could be demonstrated, but it was not statistically significant (chi-squared test; p = 0.99).
Table 2 shows the distribution of all detected microorganisms according to the mPCR and conventional culture of the collected synovial fluid. The multiplex PCR system identified Staphylococcus aureus (n = 13) and coagulase-negative Staphylococci (n = 8) as the most common pathogens. Regarding conventional culture, the most frequently found bacterium was Staphylococcus aureus (n = 18) followed by coagulase-negative Staphylococci (n = 5). Particularly noteworthy are the differences of the identified microorganisms in the mPCR and the conventional culture. Cutibacterium spp. were detected in five specimens by the multiplex PCR system, whereas the conventional culture was only able to isolate Cutibacterium avidum/granulosum in one sample. A higher detection rate of coagulase-negative Staphylococci by mPCR (n = 7) compared to the conventional culture (n = 5) was also demonstrated. On the other hand, the conventional culture was able to isolate Staphylococcus aureus in 18 specimens; the mPCR system identified this pathogen in 13 synovial fluid samples. No statistically significant difference was shown between the performance of the mPCR in patients with and without antibiotics before aspiration (Fisher’s exact test; p = 0.457).
The sensitivity and specificity of the mPCR were 71.1% (95% CI, 55.1–83.0) and 96.2% (95% CI, 86.1–99.6), respectively. A sensitivity and specificity of synovial fluid cultures were calculated with 84.2% (95% CI, 69.1–92.8) and 100.0% (95% CI, 91.6–100), respectively. The combined evaluation of mPCR and synovial fluid cultures showed a sensitivity of 92.1% (95% CI, 78.3–97.9) and a specificity of 96.2% (95% CI, 86.1–99.6), respectively. Sensitivity, specificity, LR+, LR−, AUC, PNV, and NPV of the mPCR, conventional culture, and combined evaluation of both test methods are shown in Table 3, and their ROC curves are drawn in Fig. 1.
In five patients, the mPCR system was able to identify pathogens, while the synovial fluid culture was not able to do so (Cutibacterium acnes [n = 1], coagulase-negative Staphylococci [n = 1], Cutibacterium acnes + coagulase-negative Staphylococci [n = 1; both in one patient], coagulase-negative Staphylococci [n = 1]). Out of these, two were classified aseptic, although definitive histology indicated a low-grade infection (according to Krenn classification type III), and the serum CRP-level was elevated. It is particularly noteworthy that these patients were under antimicrobial treatment. In other three mPCR-positive patients, the MSIS criteria were positive, but no microorganism was isolated in the synovial fluid culture.
Although an infection was present (according to the MSIS criteria) in eight cases, no microorganism was identified by mPCR, while the synovial fluid culture was positive (Staphylococcus aureus [n = 4], coagulase-negative Staphylococci [n = 2], Enterobacter cloacae complex [n = 1], Actinomyces neuii [n = 1]).
Three synovial fluid samples showed negative results in mPCR and SF culture, although an infection was diagnosed (Staphylococcus aureus [n = 1; tissue culture]; coagulase-negative Staphylococci [n = 1; tissue culture, sonication]; negative culture [n = 1]). In one synovial fluid sample with suspected PJI, the detected pathogens did not match. The multiplex PCR system detected Klebsiella pneumoniae, and in the conventional culture of the synovial fluid, Staphylococcus aureus was isolated. Staphylococcus aureus was also cultured in the tissue and sonication fluid, and in the blood cultures, Klebsiella pneumoniae was isolated.
In two synovial fluid samples, Cutibacterium acnes was detected by the mPCR in addition to Staphylococcus aureus (in one patient) and Cutibacterium avidum (in the other patient). However, the conventional culture only isolated Staphylococcus aureus (in the first patient) and Cutibacterium avidum (in the second patient).
Performance of resistance detection
Table 4 shows the resistance marker detected by the mPCR system in comparison with the conventional culture of all corresponding microorganisms. Nine concordant microorganisms were sensitive and did not show a resistance either in the conventional culture or in the mPCR system. Overall, the mPCR system found 11 gene resistance markers, and the conventional culture of the synovial fluid samples found 23 antibiotic resistances. In one Cutibacterium avidum/granulosum, a resistance to clindamycin was detected by conventional resistance analysis. Due to a lack of resistance gene markers, the mPCR was not able to identify this resistance. Nevertheless, in this bacterium, only the resistance gene marker [erm X] is described in the literature [9]. Therefore, the mPCR system could not detect this resistance.
In one concordant Enterococcus faecalis, the drug resistance marker macrolides/lincosamides [ermC] was detected only by mPCR. However, macrolides or lincosamides are not clinically relevant.
In one Pseudomonas aeruginosa, a resistance to ciprofloxacin was detected by conventional resistance analysis. Due to a lack of resistance gene markers, the mPCR was not able to identify this resistance.
After a mean time period of 2.58 days (SD, 3.87), the microorganism was assessed by conventional culture in patients with concordant microorganisms. The antibiogram of the conventional culture was available for the physician after an average of 3.83 (SD, 4.09) days. While Staphylococcus aureus was identified after one day, Cutibacterium avidum needed 14 days to be isolated.
Discussion
The pre-operative diagnosis of PJI remains challenging. While serum CRP and ESR may not be accurate as diagnostic tools in the pre-operative diagnosis of PJI (and identification of infection persistence), particularly to identify low-grade PJI [10, 11], the synovial fluid white blood cell count/differential showed promising results, but cannot identify the causative microorganism [12]. The conventional culture of synovial fluid samples is the current gold standard [13] but has inferior sensitivity in comparison to tissue samples and sonication fluid, and a relatively long time period is needed before results are available [14]. In recent years, attention has been paid to new diagnostic techniques, such as the alpha defensin lateral flow test [12, 15,16,17] and multiplex PCR techniques [2, 5, 6, 8]. While both test methods are able to confirm PJI, the multiplex PCR system additionally provides information about the causative pathogen.
In the present study, an 86% agreement of all cases between the mPCR system and the conventional culture could be illustrated. This was in line with the results (82%) reported by Morgenstern et al. [7]. According to the MSIS criteria, the sensitivity of the mPCR was 71%. However, it is well known that some infections, especially low-grade infections, might be present without meeting these criteria [18, 19], but we utilized them in our study since they were used in other papers that analyzed diagnostic methods of PJI [19,20,21,22,23,24]. In contrast to the MSIS criteria, proposed EBJIS criteria are assumed for better detection of low-grade PJI but show the risk to misdiagnose aseptic cases as PJI [12]. Nevertheless, the sensitivity of the mPCR was 52% if we used the EBJIS criteria which is comparable to the reported 60% by Morgenstern et al. [7]. The multiplex PCR system showed superior detection of low-virulent organisms [7]. This phenomenon was also observed in our study. In contrast, this system showed a disadvantage in identifying Staphylococcus aureus when it came to diagnosing a PJI, possibly because of the prevailing high threshold value. However, Portillo et al. demonstrated better detectability of Staphylococcus aureus [5] by mPCR in sonication fluid samples. To investigate this detail more precisely, further studies with a higher sample size are needed.
A detailed list of results reported in literature is shown in Table 5. Due to different sample material, a proper comparison to the other studies is not possible. However, the ascertained literature data evaluated materials (sonication fluid, tissue samples) removed during surgery when the revision procedure was already planned [2,3,4,5]. Most likely, the results of the mPCR or the conventional culture were only available after the surgery was finished. A detailed planning of the operation (one-stage vs. two-stage) should be done pre-operatively. The faster availability of results (5–6 h) and better detection rate of low-virulent organisms of mPCR can provide an earlier decision by the surgeon and therefore an earlier treatment for the patient. Nevertheless, the combined use of synovial fluid culture and mPCR seems to be a better diagnostic tool (sensitivity 92%) than one method alone. Therefore, the SF culture cannot be replaced by the mPCR system and should remain the standard in the preoperative investigation for the diagnosis of PJI.
However, the currently available criteria [25] only include microorganisms isolated by culture and did not mention the detection of a pathogen by another source, such as PCR. This could represent an as-yet undetected problem with these criteria. An infection could be undiagnosed and insufficiently treated. Therefore, the lack of undetected low-virulent organisms could be minimized by additional inclusion of PCR systems.
In 14 concordant microorganisms, resistance or a resistance marker was determined either in the multiplex PCR system or in the SF culture. A positive and negative conformity was illustrated five and eight times, respectively. However, six of the resistance markers identified by conventional culture (oxacillin, clindamycin, erythromycin) were not detected in the mPCR system, even though the resistance marker genes ([mecA, mecC], [ermA, ermC]) are included in this device. A limitation of detectable resistance markers by the multiplex PCR system caused a lack in identification of four antibiotic resistances detected by conventional culture (ciprofloxacin [n = 2], fosfomycin [n = 1], doxycyclin [n = 1]). In two concordant microorganisms, only mPCR identified clinical relevant resistance gene markers (Escherichia coli fluoroquinolones [gyrA], Staphylococcus aureus [aminoglycosides aac(6′)/aph(2″)]), while the synovial fluid culture was not able to do so. However, due to the small number of detected resistance markers, a recommendation is not possible.
A limitation of the mPCR system is the lack of detectable microorganisms. However, in our study, only one of these undetectable pathogens in the mPCR was isolated in the conventional culture. Hence, it seems that the most common PJI-related microorganisms can be detected by this novel mPCR device.
Conclusion
The mPCR system provides an advantage in identification of low-virulent microorganisms and has short turnaround time. In comparison with conventional culture, mPCR was inferior for detection of Staphylococcus aureus. Nevertheless, with moderate agreement compared to the conventional culture and high sensitivity of combined evaluation, this device could be a useful adjunct in pre-operative diagnosis of PJI, especially in low-grade infections.
References
Parvizi J, Gehrke T, Chen AF (2013) Proceedings of the international consensus on periprosthetic joint infection. Bone Joint J 95-b(11):1450–1452. https://doi.org/10.1302/0301-620x.95b11.33135
Achermann Y, Vogt M, Leunig M, Wust J, Trampuz A (2010) Improved diagnosis of periprosthetic joint infection by multiplex PCR of sonication fluid from removed implants. J Clin Microbiol 48(4):1208–1214. https://doi.org/10.1128/jcm.00006-10
Borde JP, Hacker GA, Guschl S, Serr A, Danner T, Hubner J, Burrack-Lange S, Ludke G, Helwig P, Hauschild O, Kern WV (2015) Diagnosis of prosthetic joint infections using UMD-Universal Kit and the automated multiplex-PCR Unyvero i60 ITI cartridge system: a pilot study. Infection. https://doi.org/10.1007/s15010-015-0796-4
Hischebeth GT, Randau TM, Buhr JK, Wimmer MD, Hoerauf A, Molitor E, Bekeredjian-Ding I, Gravius S (2016) Unyvero i60 implant and tissue infection (ITI) multiplex PCR system in diagnosing periprosthetic joint infection. J Microbiol Methods 121:27–32. https://doi.org/10.1016/j.mimet.2015.12.010
Portillo ME, Salvado M, Sorli L, Alier A, Martinez S, Trampuz A, Gomez J, Puig L, Horcajada JP (2012) Multiplex PCR of sonication fluid accurately differentiates between prosthetic joint infection and aseptic failure. J Infect 65(6):541–548. https://doi.org/10.1016/j.jinf.2012.08.018
Renz N, Feihl S, Cabric S, Trampuz A (2017) Performance of automated multiplex PCR using sonication fluid for diagnosis of periprosthetic joint infection: a prospective cohort. Infection. https://doi.org/10.1007/s15010-017-1073-5
Morgenstern C, Cabric S, Perka C, Trampuz A, Renz N (2018) Synovial fluid multiplex PCR is superior to culture for detection of low-virulent pathogens causing periprosthetic joint infection. Diagn Microbiol Infect Dis 90(2):115–119. https://doi.org/10.1016/j.diagmicrobio.2017.10.016
Suda AJ, Tinelli M, Beisemann ND, Weil Y, Khoury A, Bischel OE (2017) Diagnosis of periprosthetic joint infection using alpha-defensin test or multiplex-PCR: ideal diagnostic test still not found. Int Orthop 41(7):1307–1313. https://doi.org/10.1007/s00264-017-3412-7
Ross JI, Eady EA, Carnegie E, Cove JH (2002) Detection of transposon Tn5432-mediated macrolide-lincosamide-streptogramin B (MLSB) resistance in cutaneous propionibacteria from six European cities. J Antimicrob Chemother 49(1):165–168
Perez-Prieto D, Portillo ME, Puig-Verdie L, Alier A, Martinez S, Sorli L, Horcajada JP, Monllau JC (2017) C-reactive protein may misdiagnose prosthetic joint infections, particularly chronic and low-grade infections. Int Orthop 41(7):1315–1319. https://doi.org/10.1007/s00264-017-3430-5
Muhlhofer HML, Knebel C, Pohlig F, Feihl S, Harrasser N, Schauwecker J, von Eisenhart-Rothe R (2018) Synovial aspiration and serological testing in two-stage revision arthroplasty for prosthetic joint infection: evaluation before reconstruction with a mean follow-up of twenty seven months. Int Orthop 42(2):265–271. https://doi.org/10.1007/s00264-017-3700-2
Renz N YK, Perka C, Trampuz A (2018) Alpha defensin lateral flow test for diagnosis of periprosthetic joint infection: a screening or confirmatory test? J Bone Joint Surg Am
Renner L, Perka C, Trampuz A, Renz N (2016) Treatment of periprosthetic infections. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen 87(10):831–838. https://doi.org/10.1007/s00104-016-0255-5
Renz N, Cabric S, Janz V, Trampuz A (2015) Sonication in the diagnosis of periprosthetic infections : significance and practical implementation. Orthopade 44(12):942–945. https://doi.org/10.1007/s00132-015-3192-y
Pupaibool J, Fulnecky EJ, Swords RL Jr, Sistrunk WW, Haddow AD (2016) Alpha-defensin-novel synovial fluid biomarker for the diagnosis of periprosthetic joint infection. Int Orthop 40(12):2447–2452. https://doi.org/10.1007/s00264-016-3306-0
Sigmund IK, Holinka J, Gamper J, Staats K, Bohler C, Kubista B, Windhager R (2017) Qualitative alpha-defensin test (Synovasure) for the diagnosis of periprosthetic infection in revision total joint arthroplasty. The bone & joint journal 99-b(1):66–72. https://doi.org/10.1302/0301-620x.99b1.bjj-2016-0295.r1
Sigmund IK, Yermak K, Perka C, Trampuz A, Renz N (2018) Is the enzyme-linked immunosorbent assay more accurate than the lateral flow alpha defensin test for diagnosing periprosthetic joint infection? Clin Orthop Relat Res 476(8):1645–1654. https://doi.org/10.1097/corr.0000000000000336
Kapadia BH, Berg RA, Daley JA, Fritz J, Bhave A, Mont MA (2016) Periprosthetic joint infection. Lancet (London, England) 387(10016):386–394. https://doi.org/10.1016/s0140-6736(14)61798-0
Frangiamore SJ, Siqueira MB, Saleh A, Daly T, Higuera CA, Barsoum WK (2016) Synovial cytokines and the MSIS criteria are not useful for determining infection resolution after periprosthetic joint infection explantation. Clin Orthop Relat Res 474(7):1630–1639. https://doi.org/10.1007/s11999-016-4710-x
Deirmengian C, Kardos K, Kilmartin P, Cameron A, Schiller K, Booth RE Jr, Parvizi J (2015) The alpha-defensin test for periprosthetic joint infection outperforms the leukocyte esterase test strip. Clin Orthop Relat Res 473(1):198–203. https://doi.org/10.1007/s11999-014-3722-7
Deirmengian C, Kardos K, Kilmartin P, Cameron A, Schiller K, Parvizi J (2014) Combined measurement of synovial fluid alpha-defensin and C-reactive protein levels: highly accurate for diagnosing periprosthetic joint infection. J Bone Joint Surg Am 96(17):1439–1445. https://doi.org/10.2106/jbjs.m.01316
Kwiecien G, George J, Klika AK, Zhang Y, Bauer TW, Rueda CA (2016) Intraoperative frozen section histology: matched for musculoskeletal infection society criteria. J Arthroplast. https://doi.org/10.1016/j.arth.2016.06.019
Grammatopoulos G, Munemoto M, Inagaki Y, Tanaka Y, Athanasou NA (2016) The diagnosis of infection in metal-on-metal hip arthroplasties. J Arthroplast. https://doi.org/10.1016/j.arth.2016.03.064
George J, Kwiecien G, Klika AK, Ramanathan D, Bauer TW, Barsoum WK, Higuera CA (2016) Are frozen sections and MSIS criteria reliable at the time of reimplantation of two-stage revision arthroplasty? Clin Orthop Relat Res 474(7):1619–1626. https://doi.org/10.1007/s11999-015-4673-3
Parvizi J, Gehrke T (2014) Definition of periprosthetic joint infection. J Arthroplast 29(7):1331. https://doi.org/10.1016/j.arth.2014.03.009
Acknowledgements
Part of the results was presented at the German Congress of Orthopedic Surgery and Traumatology (DKOU 2016) in Berlin, Germany, October 25–28, 2016 and at the SICOT Congress 2016 in Rome, Italy.
Funding
Open access funding provided by Medical University of Vienna.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the institutional ethical review board of Medical University of Vienna and was done in accordance with Declaration of Helsinki.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sigmund, I.K., Windhager, R., Sevelda, F. et al. Multiplex PCR Unyvero i60 ITI application improves detection of low-virulent microorganisms in periprosthetic joint infections. International Orthopaedics (SICOT) 43, 1891–1898 (2019). https://doi.org/10.1007/s00264-018-4136-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4136-z