Abstract
Purpose
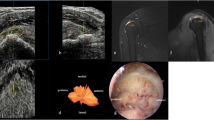
Magnetic resonance (MRI) is a valuable imaging method which can detect pre-operative rotator cuff tear characteristics accurately. However, tendon degeneration almost always necessitates a certain amount of debridement during arthroscopic repair, which alters tear size and shape. The aim of this study is to question the accuracy of the pre-operative tear size and classification in MRI and its relation to the tear size and type of the debrided tendon during arthroscopic repair.
Methods
A retrospective survey was performed to identify shoulders that underwent arthroscopic rotator cuff repair. Rotator cuff tears with an adequate history, a standard pre-operative MRI, and available surgical video records with appropriate measurements were included. Traumatic tears, calcifying tendonitis, isolated subscapularis tears, and revisions were excluded. In total, 60 shoulders’ (30 males, 27 females; age 55.2 [35–73]) preoperative MRIs and intra-operative measurements were analyzed by orthopaedic surgeons and radiologists. Tear width and type were recorded. Interdisciplinary and intradisciplinary consistency of measurements and classifications were analyzed. Tear width measured on pre-operative MRI and after debridement were compared.
Results
Average measured tear width was 9 ± 5.3 mm on MRI. Surgeons (9.98 ± 4.6 mm) measured tears significantly wider than radiologists (7.71 ± 6.6 mm). Radiologists (ICC, 0.930; CI, 0.883–0.959) showed superior consistency on MRI than surgeons (CI, 0.502; CI, 0.105–0.726). Average tear width measured after debridement (29.3 ± 9.6 mm) was significantly higher than tear width measured on pre-operative MRI (p < 0.0001). None of the researchers assessing tear type on pre-operative MRI showed agreement with surgeons assessing intra-operative data.
Conclusions
There were significant differences between the pre-operative tear characteristics on MRI and the debrided tendon characteristics during surgery, which were extensive enough to classify the tear in a different category.



Similar content being viewed by others
References
Cho NS, Rhee YG (2009) The factors affecting the clinical outcome and integrity of arthroscopically repaired rotator cuff tears of the shoulder. Clin Orthop Surg 1(2):96–104. https://doi.org/10.4055/cios.2009.1.2.96
Nho SJ, Brown BS, Lyman S, Adler RS, Altchek DW, MacGillivray JD (2009) Prospective analysis of arthroscopic rotator cuff repair: prognostic factors affecting clinical and ultrasound outcome. J Shoulder Elb Surg 18(1):13–20. https://doi.org/10.1016/j.jse.2008.05.045
Tashjian RZ, Hollins AM, Kim H-M, Teefey SA, Middleton WD, Steger-May K, Galatz LM, Yamaguchi K (2010) Factors affecting healing rates after arthroscopic double-row rotator cuff repair. Am J Sports Med 38(12):2435–2442. https://doi.org/10.1177/0363546510382835
Voigt C, Bosse C, Vosshenrich R, Schulz AP, Lill H (2010) Arthroscopic supraspinatus tendon repair with suture-bridging technique functional outcome and magnetic resonance imaging. Am J Sports Med 38(5):983–991. https://doi.org/10.1177/0363546509359063
Rol M, Favard L, Berhouet J (2018) Diagnosis of long head of biceps tendinopathy in rotator cuff tear patients: correlation of imaging and arthroscopy data. Int Orthop 42(6):1347–1355. https://doi.org/10.1007/s00264-017-3616-x
Mihata T, Watanabe C, Fukunishi K, Ohue M, Tsujimura T, Fujiwara K, Kinoshita M (2011) Functional and structural outcomes of single-row versus double-row versus combined double-row and suture-bridge repair for rotator cuff tears. Am J Sports Med 39(10):2091–2098. https://doi.org/10.1177/0363546511415660
Nove-Josserand L, Saffarini M, Hannink G, Carrillon Y (2016) Influence of pre-operative tear size and tendon retraction on repair outcomes for isolated subscapularis tears. Int Orthop 40(12):2559–2566. https://doi.org/10.1007/s00264-016-3299-8
Hsu JE, Gorbaty J, Lucas R, Russ SM, Matsen FA 3rd (2017) Treatment of irreparable cuff tears with smoothing of the humeroscapular motion interface without acromioplasty. Int Orthop 41(7):1423–1430. https://doi.org/10.1007/s00264-017-3486-2
Pander P, Sierevelt IN, Pecasse G, van Noort A (2018) Irreparable rotator cuff tears: long-term follow-up, five to ten years, of arthroscopic debridement and tenotomy of the long head of the biceps. Int Orthop. https://doi.org/10.1007/s00264-018-3991-y
Belangero PS, Ejnisman B, Arce G (2013) A review of rotator cuff classifications in current use. In: Arce G, Bak K, Shea PK et al (eds) Shoulder concepts 2013: consensus and concerns: proceedings of the ISAKOS upper extremity committees 2009–2013. Springer Berlin Heidelberg, Berlin, Heidelberg, pp 5–13. https://doi.org/10.1007/978-3-642-38097-6_2
Davidson JF, Burkhart SS, Richards DP, Campbell SE (2005) Use of preoperative magnetic resonance imaging to predict rotator cuff tear pattern and method of repair. Arthroscopy 21(12):1428. https://doi.org/10.1016/j.arthro.2005.09.015
Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K (2004) Detection and quantification of rotator cuff tears - comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am 86A(4):708–716
Neer CS (1990) Shoulder reconstruction. WB Saunders Company
Davidson J, Burkhart SS (2010) The geometric classification of rotator cuff tears: a system linking tear pattern to treatment and prognosis. Arthroscopy 26(3):417–424. https://doi.org/10.1016/j.arthro.2009.07.009
Bigliani L, Morrison D, April E (1986) The morphology of the acromion and its relationship to rotator cuff tears. Orthop Trans 10:228
Spencer EE, Dunn WR, Wright RW, Wolf BR, Spindler KP, McCarty E, Ma CB, Jones G, Safran M, Holloway B, Kuhn JE (2008) Interobserver agreement in the classification of rotator cuff tears using magnetic resonance imaging. Am J Sports Med 36(1):99–103. https://doi.org/10.1177/0363546507307504
Bryant L, Shnier R, Bryant C, Murrell GAC (2002) A comparison of clinical estimation, ultrasonography, magnetic resonance imaging, and arthroscopy in determining the size of rotator cuff tears. J Shoulder Elb Surg 11(3):219–224. https://doi.org/10.1067/mse.2002.121923
Dwyer T, Razmjou H, Henry P, Gosselin-Fournier S, Holtby R (2015) Association between pre-operative magnetic resonance imaging and reparability of large and massive rotator cuff tears. Knee Surg Sports Traumatol Arthrosc 23(2):415–422. https://doi.org/10.1007/s00167-013-2745-z
Kida Y, Morihara T, Matsuda K, Kajikawa Y, Tachiiri H, Iwata Y, Sawamura K, Yoshida A, Oshima Y, Ikeda T, Fujiwara H, Kawata M, Kubo T (2013) Bone marrow-derived cells from the footprint infiltrate into the repaired rotator cuff. J Shoulder Elb Surg 22(2):197–205. https://doi.org/10.1016/j.jse.2012.02.007
Bonnevialle N, Bayle X, Faruch M, Wargny M, Gomez-Brouchet A, Mansat P (2015) Does microvascularization of the footprint play a role in rotator cuff healing of the shoulder? J Shoulder Elb Surg 24(8):1257–1262. https://doi.org/10.1016/j.jse.2015.04.012
Parks AN, McFaline-Figueroa J, Coogan A, Poe-Yamagata E, Guldberg RE, Platt MO, Temenoff JS (2016) Supraspinatus tendon overuse results in degenerative changes to tendon insertion region and adjacent humeral cartilage in a rat model. J Orthop Res n/a-n/a. https://doi.org/10.1002/jor.23496
Jain NB, Collins J, Newman JS, Katz JN, Losina E, Higgins LD (2015) Reliability of magnetic resonance imaging assessment of rotator cuff: the ROW study. PM R 7(3):245–254.e243; quiz 254. https://doi.org/10.1016/j.pmrj.2014.08.949
Author information
Authors and Affiliations
Contributions
All authors declare that they were involved in designing the study, collecting the data, analyzing the data, writing the manuscript, and confirming the accuracy of the data and the analyses.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Institutional review board approval
The study protocol was approved by the Medical Ethics Committee of the Koç University, Istanbul, Turkey (2015.149.IRB2.054).
Additional information
The study was performed in Koc University, School of Medicine
Level 2 Diagnostic Study
Rights and permissions
About this article
Cite this article
Eren, I., Ozben, H., Gunerbuyuk, C. et al. Rotator cuff tear characteristics: how comparable are the pre-operative MRI findings with intra-operative measurements following debridement during arthroscopic repair?. International Orthopaedics (SICOT) 43, 1171–1177 (2019). https://doi.org/10.1007/s00264-018-4130-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4130-5