Abstract
Purpose and hypothesis
The aim of this study was to evaluate and to compare the radiological parameters after arthroscopic and open Latarjet technique via evaluation of computed tomography (CT) scans. Our hypothesis was that the radiological results after arthroscopic stabilisation remained in the proximity of those results achieved after open stabilisation.
Material and methods
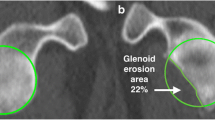
CT scan evaluation results of patients after primary Latarjet procedure were analysed. Patients operated on between 2006 and 2011 using an open technique composed the OPEN group and patients operated on arthroscopically between 2011 and 2013 composed the ARTHRO group. Forty-three out of 55 shoulders (78.2%) in OPEN and 62 out of 64 shoulders (95.3%) in ARTHRO were available for CT scan evaluation. The average age at surgery was 28 years in OPEN and 26 years in ARTHRO. The mean follow-up was 54.2 months in OPEN and 23.4 months in ARTHRO. CT scan evaluation was used to assess graft fusion and osteolysis. Bone block position and screw orientation were assessed in the axial and the sagittal views. The subscapularis muscle fatty infiltration was evaluated according to Goutallier classification.
Results
The non-union rate was significantly higher in OPEN than in ARTHRO: 5 (11.9%) versus 1 (1.7%) (p < 0.05). The total graft osteolysis was significantly higher in the OPEN group: five cases (11.9%) versus zero in ARTHRO (p < 0.05). Graft fracture incidence was comparable in both groups: in two patients in ARTHRO (3.3%) and one case (2.4%) in the OPEN group (p > 0.05). These results should be evaluated very carefully due to significant difference in the follow-up of both groups. A significantly higher rate of partial graft osteolysis at the level of the superior screw was reported in ARTHRO with 32 patients (53.3%) versus 10 (23.8%) in OPEN (p < 0.05). In the axial view, 78.4% of patients in ARTHRO and 80.5% in OPEN had the coracoid bone block in an acceptable position (between 4 mm medially and 2 mm laterally). In the sagittal plane, the bone block was in an acceptable position between 2 and 5 o’clock in 86.7% of patients in ARTHRO and 90.2% in OPEN (p > 0.05). However, in the position between 3 and 5 o’clock there were 56.7% of the grafts in ARTHRO versus 87.8% in OPEN (p < 0.05). The screws were more parallel to the glenoid surface in ARTHRO—the angles were 12.3° for the inferior screw and 12.6° for the superior one. These angles in the OPEN group were respectively 15° and 17° (p < 0.05 and for the superior screw). There was no significant difference in the presence of fatty infiltration of the subscapularis muscle.
Conclusions
Arthroscopic Latarjet stabilisation showed satisfactory radiographic results, comparable to the open procedure, however the short-term follow-up can bias this evaluation. Graft healing rate was very high in the arthroscopic technique, but yet osteolysis of the superior part of the graft and more superior graft position in the sagittal view were significantly different when compared to the open technique. The screw position was slightly more parallel to the glenoid via the arthroscopic technique. We recommend both further investigation and development of the arthroscopic technique.
Level of evidence: III.



Similar content being viewed by others
References
Latarjet M (1954) Treatment of recurrent dislocation of the shoulder. Lyon Chir 49:994–997
Bhatia S, Frank RM, Ghodara NS et al (2014) The outcomes and surgical techniques of the Latarjet procedure. Arthroscopy 30:227–235. https://doi.org/10.1016/j.arthro.2013.10.013
Paladini P, Singla R, Merolla G, Porcellini G (2016) Latarjet procedure: is the coracoid enough to restore the glenoid surface? Int Orthop 40:1675–1681. https://doi.org/10.1007/s00264-015-3093-z
Edwards BT, Walch G (2012) The Latarjet procedure for recurrent anterior shoulder instability: rationale and technique. Oper Tech Sports Med 20:57–64. https://doi.org/10.1053/j.otsm.2012.03.007
Allain J, Goutallier D, Glorion C, Surgery J (1998) Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am 80:841–852
Ladermann A, Lubbeke A, Stern R et al (2013) Risk factors for dislocation arthropathy after Latarjet procedure: a long-term study. Int Orthop 37:1093–1098. https://doi.org/10.1007/s00264-013-1848-y
Lafosse L, Lejeune E, Bouchard A et al (2007) The arthroscopic Latarjet procedure for the treatment of anterior shoulder instability. Arthroscopy 23:1242e1–1242e5. https://doi.org/10.1016/j.arthro.2007.06.008
Lafosse L, Boyle S (2010) Arthroscopic Latarjet procedure. J Shoulder Elb Surg 19:2–12. https://doi.org/10.1016/j.jse.2009.12.010
Dumont GD, Fogerty S, Rosso C, Lafosse L (2014) The arthroscopic latarjet procedure for anterior shoulder instability: 5-year minimum follow-up. Am J Sports Med 42:2560–2566. https://doi.org/10.1177/0363546514544682
Boileau P, Gendre P, Baba M et al (2016) A guided surgical approach and novel fixation method for arthroscopic Latarjet. J Shoulder Elb Surg 25:78–89. https://doi.org/10.1016/j.jse.2015.06.001
Wellmann M, Petersen W, Zantop T et al (2009) Open shoulder repair of osseous glenoid defects: biomechanical effectiveness of the Latarjet procedure versus a contoured structural bone graft. Am J Sports Med 37:87–94. https://doi.org/10.1177/0363546508326714
Hovelius L, Sandström B, Sundgren K, Saebö M (2004) One hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: study I - clinical results. J Shoulder Elb Surg 13:509–516. https://doi.org/10.1016/j.jse.2004.02.013
Mizuno N, Denard PJ, Raiss P et al (2014) Long-term results of the Latarjet procedure for anterior instability of the shoulder. J Shoulder Elb Surg 23:1691–1699. https://doi.org/10.1016/j.jse.2014.02.015
Meyer DC, Moor BK, Gerber C et al (2013) Accurate coracoid graft placement through use of a drill guide for the Latarjet procedure. J Shoulder Elb Surg 22:701–708. https://doi.org/10.1016/j.jse.2012.06.012
Casabianca L, Gerometta A, Massein A et al (2016) Graft position and fusion rate following arthroscopic Latarjet. Knee Surg Sports Traumatol Arthrosc 24:507–512. https://doi.org/10.1007/s00167-015-3551-6
Kany J, Flamand O, Grimberg J et al (2016) Arthroscopic Latarjet procedure: is optimal positioning of the bone block and screws possible? A prospective computed tomography scan analysis. J Shoulder Elb Surg 25:69–77. https://doi.org/10.1016/j.jse.2015.06.010
Itoi E, Lee S-B, Amrami KK et al (2003) Quantitative assessment of classic anteroinferior bony Bankart lesions by radiography and computed tomography. Am J Sports Med 31:112–118
Doursounian L, Debet-Mejean A, Chetboun A, Nourissat G (2009) Bristow-Latarjet procedure with specific instrumentation: study of 34 cases. Int Orthop 33:1031–1036. https://doi.org/10.1007/s00264-008-0606-z
Clavert P, Koch G, Neyton L et al (2016) Is anterior glenoid bone block position reliably assessed by standard radiography? A cadaver study. Orthop Traumatol Surg Res 102:S281–S285. https://doi.org/10.1016/j.otsr.2016.08.005
Kordasiewicz B, Malachowski K, Kicinski M et al (2017) Comparative study of open and arthroscopic coracoid transfer for shoulder anterior instability (Latarjet)-clinical results at short term follow-up. Int Orthop 41(5):1023–1033. https://doi.org/10.1007/s00264-016-3372-3
Kraus TM, Martetschläger F, Graveleau N et al (2013) CT-based quantitative assessment of the surface size and en-face position of the coracoid block post-Latarjet procedure. Arch Orthop Trauma Surg 133:1543–1548. https://doi.org/10.1007/s00402-013-1825-3
Ladermann A, Denard PJ, Burkhart SS (2012) Injury of the suprascapular nerve during latarjet procedure: an anatomic study. Arthroscopy 28:316–321. https://doi.org/10.1016/j.arthro.2011.08.307
Goutallier D, Postel JM, Bernageau J et al (1995) Fatty infiltration of disrupted rotator cuff muscles. Rev Rhum Engl Ed 62:415–422
Lunn JV, Castellano-Rosa J, Walch G (2008) Recurrent anterior dislocation after the Latarjet procedure: outcome after revision using a modified Eden-Hybinette operation. J Shoulder Elb Surg 17:744–750. https://doi.org/10.1016/j.jse.2008.03.002
Hovelius L, Sandstrom B, Saebo M (2006) One hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: study II—the evolution of dislocation arthropathy. J Shoulder Elb Surg 15:279–289. https://doi.org/10.1016/j.jse.2005.09.014
Hovelius L, Sandström B, Olofsson A et al (2012) The effect of capsular repair, bone block healing, and position on the results of the Bristow-Latarjet procedure (study III): long-term follow-up in 319 shoulders. J Shoulder Elb Surg 21:647–660. https://doi.org/10.1016/j.jse.2011.03.020
Schmid SL, Farshad M, Catanzaro S, Gerber C (2012) The Latarjet procedure for the treatment of recurrence of anterior instability of the shoulder after operative repair: a retrospective case series of forty-nine consecutive patients. J Bone Joint Surg Am 94:e75. https://doi.org/10.2106/JBJS.K.00380
Hovelius L, Eriksson K, Fredin H et al (1983) Recurrences after initial dislocation of the shoulder. Results of a prospective study of treatment. J Bone Joint Surg Am 65:343–349
Walch G (1991) Recurrent anterior shoulder instability [in French]. Rev Chir Orthop Reparatrice Appar Mot 77(Suppl 1):177–191
Shah AA, Butler RB, Romanowski J et al (2012) Short-term complications of the Latarjet procedure. J Bone Joint Surg Am 94:495–501. https://doi.org/10.2106/JBJS.J.01830
Butt U, Charalambous CP (2012) Complications associated with open coracoid transfer procedures for shoulder instability. J Shoulder Elb Surg 21:1110–1119. https://doi.org/10.1016/j.jse.2012.02.008
Haeni DL, Opsomer G, Sood A et al (2016) Three-dimensional volume measurement of coracoid graft osteolysis after arthroscopic Latarjet procedure. J Shoulder Elb Surg. https://doi.org/10.1016/j.jse.2016.08.007
Di Giacomo G, Costantini A, De Gasperis N et al (2011) Coracoid graft osteolysis after the Latarjet procedure for anteroinferior shoulder instability: a computed tomography scan study of twenty-six patients. J Shoulder Elb Surg 20:989–995. https://doi.org/10.1016/j.jse.2010.11.016
Moroder P, Blocher M, Auffarth A et al (2014) Clinical and computed tomography-radiologic outcome after bony glenoid augmentation in recurrent anterior shoulder instability without significant glenoid bone loss. J Shoulder Elb Surg 23:420–426. https://doi.org/10.1016/j.jse.2013.07.048
Boileau P, Mercier N, Roussanne Y et al (2010) Arthroscopic Bankart-Bristow-Latarjet procedure: the development and early results of a safe and reproducible technique. Arthroscopy 26:1434–1450. https://doi.org/10.1016/j.arthro.2010.07.011
Cunningham G, Benchouk S, Kherad O, Lädermann A (2016) Comparison of arthroscopic and open Latarjet with a learning curve analysis. Knee Surg Sports Traumatol Arthrosc 24:540–545. https://doi.org/10.1007/s00167-015-3910-3
Zumstein V, Kraljevic M, Conzen A et al (2014) Thickness distribution of the glenohumeral joint cartilage: a quantitative study using computed tomography. Surg Radiol Anat 36:327–331. https://doi.org/10.1007/s00276-013-1221-2
Metais P, Clavert P, Barth J et al (2016) Preliminary clinical outcomes of Latarjet-Patte coracoid transfer by arthroscopy vs. open surgery: prospective multicentre study of 390 cases. Orthop Traumatol Surg Res 102:S271–S276. https://doi.org/10.1016/j.otsr.2016.08.003
Maynou C, Cassagnaud X, Mestdagh H (2005) Function of subscapularis after surgical treatment for recurrent instability of the shoulder using a bone-block procedure. J Bone Joint Surg Br 87:1096–1101. https://doi.org/10.1302/0301-620X.87B8.14605
Hardy A, Gerometta A, Granger B et al (2016) Preoperative CT planning of screw length in arthroscopic Latarjet. Knee Surg Sports Traumatol Arthrosc 1–7. https://doi.org/10.1007/s00167-016-4286-8
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kordasiewicz, B., Kicinski, M., Małachowski, K. et al. Comparative study of open and arthroscopic coracoid transfer for shoulder anterior instability (Latarjet)—computed tomography evaluation at a short term follow-up. Part II. International Orthopaedics (SICOT) 42, 1119–1128 (2018). https://doi.org/10.1007/s00264-017-3739-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3739-0