Abstract
Purpose
The purpose of the study was to determine if patients undergoing percutaneous biopsy for genetic profiling are undergoing more biopsies (procedures, passes per procedure), or experiencing more procedure-related complications.
Methods
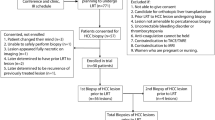
60 patients undergoing biopsy procedures for genetic profiling were retrospectively compared with 60 consecutive control patients undergoing routine biopsies. Procedural details and related complications were collected. Results were analyzed using t-tests and logistic regression.
Results
Biopsied organs included mainly lung (n = 31), liver (n = 50), and lymph nodes (n = 18). The average number of core biopsy passes was 3.45 in the study group and 2.18 in the control group (0.73, 1.81; p = 0.0001). The average study patient underwent 1.44 biopsy procedures by radiology from 2016 to 2017, whereas the average control patient underwent 1.08 (0.1657, 0.5010, p = 0.0002). Results were similar when looking at the subset of patients undergoing liver biopsies. In our cohort of 120 patients total, only 6 complications were noted. There were 4 complications in the control patients and 2 complications in the study patients, all of which were pneumothoraces in patients undergoing lung biopsy; only 2 of these required treatment. The odds ratio for a complication occurring from an increase in one core biopsy is 1.07 (0.601, 1.573; p = 0.775), suggesting no significant relationship among the number of biopsies taken and the probability of complication in this cohort.
Conclusions
Patients being biopsied for genetic profiling or clinical study enrollment are undergoing more biopsy procedures and more biopsy passes per procedure, but are not experiencing a detectable increased rate of complications in this small cohort, single-center study.

Similar content being viewed by others
References
Corr BR, Behbakht K, Spillman MA (2013) Gynecologic biopsy for molecular profiling: a review for the interventional radiologist. Semin Intervent Radiol 30:417–424
Cox VL, Bhosale P, Varadhachary GR, et al. (2017) Cancer genomics and important oncologic mutations: a contemporary guide for body imagers. Radiology 283:314–340
MacConaill LE (2013) Existing and emerging technologies for tumor genomic profiling. J Clin Oncol 31:1815–1824
Sabir SH, Krishnamurthy S, Gupta S, et al. (2017) Characteristics of percutaneous core biopsies adequate for next generation genomic sequencing. PLoS One 12:e0189651
Basik M, Aguilar-Mahecha A, Rousseau C, et al. (2013) Biopsies: next-generation biospecimens for tailoring therapy. Nat Rev Clin Oncol 10:437–450
Winter TC, Lee FT Jr, Hinshaw JL (2008) Ultrasound-guided biopsies in the abdomen and pelvis. Ultrasound Q 24:45–68
Kennedy SA, Milovanovic L, Midia M (2015) Major bleeding after percutaneous image-guided biopsies: frequency, predictors, and periprocedural management. Semin Intervent Radiol 32:26–33
van Beek D, Funaki B (2013) Hemorrhage as a complication of percutaneous liver biopsy. Semin Intervent Radiol 30:413–416
Atwell TD, Smith RL, Hesley GK, et al. (2010) Incidence of bleeding after 15,181 percutaneous biopsies and the role of aspirin. AJR Am J Roentgenol 194:784–789
Pieper M, Schmitz J, McBane R, et al. (2017) Bleeding complications following image-guided percutaneous biopsies in patients taking clopidogrel-a retrospective review. J Vasc Interv Radiol 28:88–93
Biankin AV, Waddell N, Kassahn KS, et al. (2012) Pancreatic cancer genomes reveal aberrations in axon guidance pathway genes. Nature 491:399–405
Lee MH, Lubner MG, Hinshaw JL, Pickhardt PJ (2018) Ultrasound guidance versus CT guidance for peripheral lung biopsy: performance according to lesion size and pleural contact. AJR Am J Roentgenol 210:W1–W8
Patel IJ, Davidson JC, Nikolic B, et al. (2012) Consensus guidelines for periprocedural management of coagulation status and hemostasis risk in percutaneous image-guided interventions. J Vasc Interv Radiol 23:727–736
Graffy P, Loomis SB, Pickhardt PJ, et al. (2017) Pulmonary intraparenchymal blood patching decreases the rate of pneumothorax-related complications following percutaneous CT-guided needle biopsy. J Vasc Interv Radiol 28(608–613):e601
Wagner JM, Hinshaw JL, Lubner MG, et al. (2011) CT-guided lung biopsies: pleural blood patching reduces the rate of chest tube placement for postbiopsy pneumothorax. AJR Am J Roentgenol 197:783–788
Prince J, Bultman E, Hinshaw L, et al. (2015) Patient and tumor characteristics can predict nondiagnostic renal mass biopsy findings. J Urol 193:1899–1904
Dindo D, Demartines N, Clavien P (2004) Classification of surgical complications. Ann Surg 240:205–213
Ettinger DS, Wood DE, Aisner DL, et al. (2017) Non-small cell lung cancer, version 5.2017 clinical practice guidelines in oncology. J Natl Compr Canc Netw 15:504–535
Benson AB, Venook AP, Cederquist L, et al. (2017) Colon cancer, version 1.2017 clinical practice guidelines in oncology. J Natl Compr Cancer Netw 15:370–398
Ajani JA, D’Amico TA, Almhanna K, et al. (2016) Gastric cancer, version 3.2016. J Natl Compr Cancer Netw 14:1286–1312
Coit DG, Thompson JA, Algazi A, et al. (2016) Melanoma, version 2.2016. J Natl Compr Cancer Netw 14:450
Zhou C, Wu YL, Chen G, et al. (2011) Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol 12:735–742
Solomon BJ, Mok T, Kim DW, et al. (2014) First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med 371:2167–2177
Sosman JA, Kim KB, Schuchter L, et al. (2012) Survival in BRAF V600-mutant advanced melanoma treated with vemurafenib. N Engl J Med 366:707–714
Bang YJ, Van Cutsem E, Feyereislova A, et al. (2010) Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet 376:687–697
Van Cutsem E, Lenz HJ, Kohne CH, et al. (2015) Fluorouracil, leucovorin, and irinotecan plus cetuximab treatment and RAS mutations in colorectal cancer. J Clin Oncol 33:692–700
Cohen MB, A-Kader HH, Lambers D, Heubi JE (1992) Complications of percutaneous liver biopsy in children. Gastroenterology 102:629–632
Seeff LB, Everson GT, Morgan TR, et al. (2010) Complication rate of percutaneous liver biopsies among persons with advanced chronic liver disease in the HALT-C trial. Clin Gastroenterol Hepatol 8:877–883
Heng C, Hansen BE, Tang WY, et al. (2017) Multiple biopsy passes and the risk of complications of percutaneous liver biopsy. Eur J Gastroenterol Hepatol 29:36–41
McGill DB, Rakela J, Zinsmeister AR, Ott BJ (1990) A 21-year experience with major hemorrhage after percutaneous liver biopsy. Gastroenterology 99:1396–1400
Abel EJ, Heckman JE, Hinshaw L, et al. (2015) Multi-quadrant biopsy technique improves diagnostic ability in large heterogeneous renal masses. J Urol 194:886–891
Winokur RS, Pua BB, Sullivan BW, Madoff DC (2013) Percutaneous lung biopsy: technique, efficacy, and complications. Semin Intervent Radiol 30:121–127
McSweeney SE, O’Regan KN, Mc Laughlin PD, Crush L, Maher MM (2012) Evaluation of the efficacy and safety of percutaneous biopsy of lung. Open Respir Med J 6:82–88
Wu CC, Maher MM, Shepard JA (2011) Complications of CT-guided percutaneous needle biopsy of the chest: prevention and management. AJR Am J Roentgenol 196:W678–682
Hiraki T, Mimura H, Gobara H, et al. (2010) Incidence of and risk factors for pneumothorax and chest tube placement after CT fluoroscopy-guided percutaneous lung biopsy: retrospective analysis of the procedures conducted over a 9-year period. AJR Am J Roentgenol 194:809–814
McInnes MDF, Kielar AZ, Macdonald DB (2011) Percutaneous image-guided biopsy of the spleen: systematic review and meta-analysis of the complication rate and diagnostic accuracy. Radiology 260:699–708
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Disclosures
Dr. Lubner has no relevant conflicts, but receives Grant funding from Philips, Ethicon. Dr. Pickhardt has no relevant conflicts but is co-founder of VirtuoCTC, consultant for Bracco and Check-Cap, and shareholder in SHINE, Elucent, and Cellectar Biosciences. Dr. Hinshaw has no relevant conflicts but is a consultant for Neuwave, Shareholder in Elucent, LiteRay, Accure, Histosonics, and Cellectar. All other authors have no disclosures.
Research approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Cherukuri, A.R., Lubner, M.G., Zea, R. et al. Tissue sampling in the era of precision medicine: comparison of percutaneous biopsies performed for clinical trials or tumor genomics versus routine clinical care. Abdom Radiol 44, 2074–2080 (2019). https://doi.org/10.1007/s00261-018-1702-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1702-1