Abstract
Purpose
The purpose of the study is to propose a computed tomography (CT) classification of spontaneous isolated superior mesenteric artery dissection (SISMAD) correlated with clinical presentation
Methods
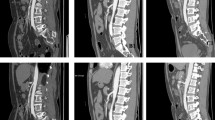
We retrospectively reviewed CT images of 40 patients with SISMAD at our institution from 2006 to 2015 and proposed a new classification: type I, patent false lumen with both entry and re-entry; type II, patent false lumen without re-entry; type III, completely or partially thrombosed false lumen; and type IV, thrombosed false lumen with ulcer-like projection. Additionally, we included a subtype (S) at each type when there was either a long segment of dissection and/or significant true lumen stenosis. CT features were statistically analyzed using Fisher’s exact and Mann–Whitney test.
Results
The CT findings classified patients as type I (15%), type II (12.5%), type III (35%), and type IV (37.5%). Of the 40 patients, 25 (62.5%) were symptomatic. There was a significantly different proportion of each type between symptomatic and asymptomatic patients (p = 0.005). There were 25 patients with subtype (S); no type I or II, 12 type III, and 13 type IV. The symptomatic patients showed longer dissection tendency and more severe true lumen stenosis (78% vs. 53%, p = 0.000) compared with asymptomatic patients.
Conclusion
The proposed multi-detector CT classification of SISMAD correlates with clinical presentation. This new classification could be helpful for treatment planning.




Similar content being viewed by others
References
Gouëffic Y, Costargent A, Dupas B, et al. (2002) Superior mesenteric artery dissection: case report. J Vasc Surg 35(5):1003–1005
Cho B, Lee M, Lee M, et al. (2011) Treatment guidelines for isolated dissection of the superior mesenteric artery based on follow-up CT findings. Eur J Vasc Endovasc Surg 41(6):780–785
Cho Y, Ko G, Kim H, Moon K, Kwon T (2009) Conservative management of symptomatic spontaneous isolated dissection of the superior mesenteric artery. Br J Surg 96(7):720–723
Min S-I, Yoon K-C, Min S-K, et al. (2011) Current strategy for the treatment of symptomatic spontaneous isolated dissection of superior mesenteric artery. J Vasc Surg 54(2):461–466
Park YJ, Park KB, Kim D-I, et al. (2011) Natural history of spontaneous isolated superior mesenteric artery dissection derived from follow-up after conservative treatment. J Vasc Surg 54(6):1727–1733
Subhas G, Gupta A, Nawalany M, Oppat WF (2009) Spontaneous isolated superior mesenteric artery dissection: a case report and literature review with management algorithm. Ann Vasc Surg 23(6):788–798
Yun W, Kim Y, Park K, et al. (2009) Clinical and angiographic follow-up of spontaneous isolated superior mesenteric artery dissection. Eur J Vasc Endovasc Surg 37(5):572–577
Ko SH, Hye R, Frankel DA (2015) Management of spontaneous isolated visceral artery dissection. Ann Vasc Surg 29(3):470–474
Lv PH, Zhang XC, Wang LF, Chen ZL, Shi HB (2014) Management of isolated superior mesenteric artery dissection. World J Gastroenterol 20(45):17179–17184
Morris JT, Guerriero J, Sage JG, Mansour MA (2008) Three isolated superior mesenteric artery dissections: update of previous case reports, diagnostics, and treatment options. J Vasc Surg 47(3):649–653
Nagai T, Torishima R, Uchida A, et al. (2004) Spontaneous dissection of the superior mesenteric artery in four cases treated with anticoagulation therapy. Intern Med 43(6):473–478
Takahashi B, Nakayama Y, Shiroma S, Ido K (2015) Three case report of spontaneous isolated dissection of the superior mesenteric artery-with an algorithm proposed for the management. Ann Vasc Dis 8(2):120–123
Sakamoto I, Ogawa Y, Sueyoshi E, et al. (2007) Imaging appearances and management of isolated spontaneous dissection of the superior mesenteric artery. Eur J Radiol 64(1):103–110
D-l Li, Y-Y He, Alkalei AM, et al. (2014) Management strategy for spontaneous isolated dissection of the superior mesenteric artery based on morphologic classification. J Vasc Surg 59(1):165–172
Luan J, Li X (2013) Computed tomography imaging features and classification of isolated dissection of the superior mesenteric artery. Eur J Vasc Endovasc Surg 46(2):232–235
Zerbib P, Perot C, Lambert M, et al. (2010) Management of isolated spontaneous dissection of superior mesenteric artery. Langenbeck’s Arch Surg 395(4):437–443
Foord A, Lewis R (1959) Primary dissecting aneurysms of peripheral and pulmonary arteries: dissecting hemorrhage of media. Arch Pathol 68:553
Park YJ, Park C-W, Park KB, et al. (2011) Inference from clinical and fluid dynamic studies about underlying cause of spontaneous isolated superior mesenteric artery dissection. J Vasc Surg 53(1):80–86
Ghuysen A, Meunier P, Van Damme H, Creemers E, D’orio V (2008) Isolated spontaneous dissection of the superior mesenteric artery: a case report. Annales de cardiologie et d’angeiologie 4:238–242
Suzuki S, Furui S, Kohtake H, et al. (2004) Isolated dissection of the superior mesenteric artery. Abdom Imaging 29(2):153–157
Kim H-K, Jung HK, Cho J, Lee J-M, Huh S (2014) Clinical and radiologic course of symptomatic spontaneous isolated dissection of the superior mesenteric artery treated with conservative management. J Vasc Surg 59(2):465–472
Roussel A, Pellenc Q, Corcos O, et al. (2015) Spontaneous and isolated dissection of the superior mesenteric artery: proposal of a management algorithm. Ann Vasc Surg 29(3):475–481
Sueyoshi E, Matsuoka Y, Imada T, et al. (2002) New Development of an ulcerlike projection in aortic intramural hematoma: CT evaluation 1. Radiology 224(2):536–541
Kitai T, Kaji S, Yamamuro A, et al. (2010) Impact of new development of ulcer-like projection on clinical outcomes in patients with type B aortic dissection with closed and thrombosed false lumen. Circulation 122(11 suppl 1):S74–S80
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Yoo, J., Lee, J.B., Park, H.J. et al. Classification of spontaneous isolated superior mesenteric artery dissection: correlation with multi-detector CT features and clinical presentation. Abdom Radiol 43, 3157–3165 (2018). https://doi.org/10.1007/s00261-018-1556-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1556-6