Abstract
Purpose
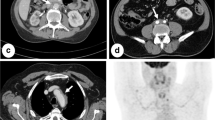
To assess the frequency with which previously reported characteristic findings of retroperitoneal fibrosis (RPF) (a circumferential or almost circumferential peri-aortic mass centered at L4, which does not displace the abdominal aorta or proximal common iliac arteries) are present in patients with RPF, in patients with other fibrosing diseases, and in cancer patients referred to a subspecialty clinic with a suspected diagnosis of RPF, in order to determine whether diagnostic percutaneous biopsy can be avoided in some patients.
Methods
This HIPAA-compliant Institutional Review Board-approved retrospective study assessed clinical and CT and MR imaging abnormalities on imaging studies in 92 patients referred to a subspecialty clinic with suspected RPF over a 14-year period. Two reviewers, in consensus, determined the frequency of different CT and MRI findings in three groups of patients (Group 1: those with an eventual diagnosis of RPF, Group 2: those with a fibrosing disease associated with vascular or urologic abnormalities, and Group 3: those with cancer). Assessed imaging features included the presence of retroperitoneal masses, whether masses were single or multiple, whether such masses were circumferential or nearly circumferential, whether they displaced the aorta away from the spine (with the degree of such displacement measured), and whether there were abnormalities outside of the peri-aortic region of the retroperitoneum. The frequency with which findings previously reported as characteristic of RPF were present was determined for each of the three groups. Imaging results were correlated with the final diagnoses.
Results
Of 68 subjects eventually diagnosed with retroperitoneal fibrosis (RPF) (Group 1), 47 had peri-aortic retroperitoneal masses, 18 of which displaced the aorta anteriorly away from the spine. Of 12 subjects with fibrosing abnormalities related to vascular or urologic disease (Group 2), six had retroperitoneal masses, none of which displaced the aorta away from the spine. Of 12 subjects with malignancies (Group 3), six had peri-aortic retroperitoneal masses only two of whom had aortic displacement. Only 34 of 68 Group 1 subjects had peri-aortic masses characteristic of RPF, compared with six Group 2 subjects and one Group 3 subject. Subjects with characteristic retroperitoneal masses were significantly more likely to have benign disease than cancer (p = 0.009).
Conclusion
Many patients with RPF do not have characteristic imaging findings. Contrary to prior publications, absence of aortic displacement is not seen in all patients with RPF and is seen in some cancer patients. Nonetheless, when infiltrative peri-aortic retroperitoneal soft tissue that does not displace the aorta is encountered on CT or MRI, RPF can be diagnosed with a high degree of confidence, obviating the need for biopsy.







Similar content being viewed by others
References
Swartz R (2009) Idiopathic fibrosis: a review of the pathogenesis and approaches to treatment. Am J Kid Dis 2009(54):546–553
Kermani TA, Crowson CS, Achenbach MS, Luthra HS (2011) Idiopathic retroperitoneal fibrosis: a retrospective review of clinical presentation, treatment, and outcomes. Mayo Clin Proc 86:297–303
Li KP, Zhu J, Zhang J (2011) Idiopathic retroperitoneal fibrosis (RPF): clinical features of 61 cases and literature review. Clin Rheumatol 30:601–605
Scheel PJ, Feeley N (2013) Retroperitoneal fibrosis. Rheum Dis Clin N Am 39:365–381
Liu H, Zhang G, Niu Y, Jiang N, Xiao W (2014) Retroperitoneal fibrosis: a clinical and outcome analysis of 58 cases and review of the literature. Rheumatol Int 34:1665–1670
Vaglio A, Salvarani C, Buzio C (2006) Retroperitoneal fibrosis. Lancet 367:241–251
Goldini M, Bonini S, Urban M, et al. (2014) Asbestos and smoking as risk factors for idiopathic retroperitoneal fibrosis. Ann Intern Med 161:181–188
Swartz RD (2015) Retroperitoneal fibrosis and asbestosis—a plausible association? Am J Kidney Dis 65:378–380
Amis ES (1991) Retroperitoneal fibrosis. AJR 57:321–329
Vaglio A, Salvarani C, Buzio C (2006) Retroperitoneal fibrosis. Lancet 367:241–251
Pelkman L, Aarndouse A, Hendriksz T, van Bommel E (2012) Value of acute-phase reactants in monitoring disease activity and response to treatment in idiopathic retroperitoneal fibrosis. Neph Dial Transpl 27:2815–2819
Gilkeson GS, Allen NB (1996) Retroperitoneal fibrosis: a true connective tissue disease. Rheum Dis Clin N Am 22:23–38
Degesys G, Dunnick NR, Silverman PM, et al. (1986) Retroperitoneal fibrosis: use of CT in distinguishing among possible causes. AJR 146:57–60
Amis ES Jr (1991) Retroperitoneal fibrosis. AJR 157:321–329
Oliveira Caiafa R, Sierra Vinuesa A, Salvador Izquierdo R, et al. (2013) Retroperitoneal fibrosis: role of imaging in diagnosis and follow up. Radiographics 33:535–552
Baker LR, Mallinson WJ, Gregory MC, et al. (1987) Idiopathic retroperitoneal fibrosis: a retrospective analysis of 60 cases. Br J Urol 60:497–503
Rosenkrantz AB, Spieler B, Seuss CR, Stifelman MD, Kim S (2012) Utility of MRI features for differentiation of retroperitoneal fibrosis and lymphoma. AJR 199:118–126
Bakir B, Yilmaz F, Turkay R, et al. (2014) Role of diffusion-weighted MR imaging in the differentiation of benign retroperitoneal fibrosis from malignant neoplasm: preliminary study. Radiology 272:438–445
Stone J (2012) IgG4-related disease: nomenclature, clinical features, and treatment. Semin Diagn Pathol 29:177–190
Mahajan V, Mattoo H, Deshpande V, Pillai S, Sonte J (2014) IgG4-related disease. Ann Rev Pathol Mech Dis 9:315–347
Khosroshahi A, Wallace ZS, Crowe JL, et al. (2015) International consensus guidance statement on the management and treatment of IgG4-related disease. Arthritis Rheumatol 67:1688–1699
Chiba K, Kamisawa T, Tabata T, et al. (2013) Clinical features of 10 patients with IgG4-related retroperitoneal fibrosis. Int Med 52:1545–1551
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received in support of this study.
Conflict of interest
All authors declare that they have conflicts of interest.
Ethical Approval
All procedures performed with the human participants in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The need for informed consent was waived due to the retrospective nature of this study.
Rights and permissions
About this article
Cite this article
Cohan, R.H., Shampain, K.L., Francis, I.R. et al. Imaging appearance of fibrosing diseases of the retroperitoneum: can a definitive diagnosis be made?. Abdom Radiol 43, 1204–1214 (2018). https://doi.org/10.1007/s00261-017-1282-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-017-1282-5