Abstract
Purpose
Dynamic 18F-fluorodeoxyglucose (FDG) PET can be used to quantitatively assess the rate of myocardial glucose uptake (MRGlu). The aim of this study was to evaluate the clinical significance and prognostic value of right ventricular (RV) MRGlu in patients with coronary artery disease and heart failure with reduced ejection fraction.
Methods
Patients with left ventricular ejection fraction (LVEF) ≤ 40% were consecutively enrolled for FDG PET between November 2012 and May 2017. Global LV and RV MRGlu (μmol/min/100 g) were analyzed. Outcome events were independently assessed using electronic medical records to determine hospitalization for revascularization, new-onset ischemic events, heart failure, cardiovascular, and all-cause death. Differences between LV and RV MRGlu and associations with clinical characteristics and echocardiographic data were evaluated. Associations among FDG PET findings and outcomes were analyzed using Kaplan-Meier survival analysis.
Results
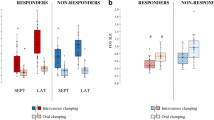
Seventy-five patients (mean age 62.2 ± 12.7 years, male 85.3%, LVEF 19.3 ± 8.6%) were included for analysis. The mean glucose utilization ratio of RV-to-LV (RV/LV MRGlu) was 89.5 ± 264.9% (r = 0.77, p < 0.001). Positive correlations between RV MRGlu and maximal tricuspid regurgitation peak gradient (r = 0.28, p = 0.033) and peak tricuspid regurgitation jet velocity (r = 0.29, p = 0.021) were noted. LVEF was positively correlated with LV MRGlu (r = 0.27, p = 0.018), but negatively correlated with end-diastolic volume (r = − 0.37, p = 0.001), end-systolic volume (r = − 0.54, p < 0.001), and RV/LV MRGlu (r = − 0.40, p < 0.001). However, RV MRGlu was not well correlated with LVEF. Forty-three patients received revascularization procedures after FDG PET, and 13 patients died in a mean follow-up period of 496 ± 453 days (1–1788 days), including nine cardiovascular deaths. Higher RV and LV MRGlu values, LVEF ≤ 16% and LV end-diastolic volume ≥ 209 ml of gated-PET were associated with poor overall survival and cardiac outcomes.
Conclusions
In patients with coronary artery disease and ischemic cardiomyopathy, RV glucose utilization was positively correlated with RV pressure overload, but not LVEF. Global LV and RV MRGlu, LVEF, and LV end-diastolic volume showed significant prognostic value.



Similar content being viewed by others
References
Guo Y, Lip GY, Banerjee A. Heart failure in East Asia. Curr Cardiol Rev. 2013;9:112–22.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2013;62:e147–239.
Savarese G, Lund LH. Global public health burden of heart failure. Card Fail Rev. 2017;3:7–11.
Abebe TB, Gebreyohannes EA, Tefera YG, Abegaz TM. Patients with HFpEF and HFrEF have different clinical characteristics but similar prognosis: a retrospective cohort study. BMC Cardiovasc Disord. 2016;16:232.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the heart failure association (HFA) of the ESC. Eur Heart J. 2016;37:2129–200.
Kerkhof PL. Characterizing heart failure in the ventricular volume domain. Clin Med Insights Cardiol. 2015;9:11–31.
Reyes EB, Ha JW, Firdaus I, Ghazi AM, Phrommintikul A, Sim D, et al. Heart failure across Asia: same healthcare burden but differences in organization of care. Int J Cardiol. 2016;223:163–7.
Wang CC, Chang HY, Yin WH, Wu YW, Chu PH, Wu CC, et al. TSOC-HFrEF registry: a registry of hospitalized patients with decompensated systolic heart failure: description of population and management. Acta Cardiol Sin. 2016;32:400–11.
Wu CK, Juang JJ, Chiang JY, Li YH, Tsai CT, Chiang FT. The Taiwan heart registries: its influence on cardiovascular patient care. J Am Coll Cardiol. 2018;71:1273–83.
Lammertsma AA. Forward to the past: the case for quantitative PET imaging. J Nucl Med. 2017;58:1019–24.
Kluge R, Barthel H, Pankau H, Seese A, Schauer J, Wirtz H, et al. Different mechanisms for changes in glucose uptake of the right and left ventricular myocardium in pulmonary hypertension. J Nucl Med. 2005;46:25–31.
Wang L, Li W, Yang Y, Wu W, Cai Q, Ma X, et al. Quantitative assessment of right ventricular glucose metabolism in idiopathic pulmonary arterial hypertension patients: a longitudinal study. Eur Heart J Cardiovasc Imaging. 2016;17:1161–8.
Raina A, Meeran T. Right ventricular dysfunction and its contribution to morbidity and mortality in left ventricular heart failure. Curr Heart Fail Rep. 2018;15:94–105.
Bleasdale RA, Frenneaux MP. Prognostic importance of right ventricular dysfunction. Heart. 2002;88:323–4.
Galie N, McLaughlin VV, Rubin LJ, Simonneau G. An overview of the 6th world symposium on pulmonary hypertension. Eur Respir J. 2019;53:1802148.
Bossone E, D'Andrea A, D'Alto M, Citro R, Argiento P, Ferrara F, et al. Echocardiography in pulmonary arterial hypertension: from diagnosis to prognosis. J Am Soc Echocardiogr. 2013;26:1–14.
Chemla D, Castelain V, Humbert M, Hebert JL, Simonneau G, Lecarpentier Y, et al. New formula for predicting mean pulmonary artery pressure using systolic pulmonary artery pressure. Chest. 2004;126:1313–7.
Parasuraman S, Walker S, Loudon BL, Gollop ND, Wilson AM, Lowery C, et al. Assessment of pulmonary artery pressure by echocardiography-a comprehensive review. Int J Cardiol Heart Vasc. 2016;12:45–51.
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685–713.
Austin C, Alassas K, Burger C, Safford R, Pagan R, Duello K, et al. Echocardiographic assessment of estimated right atrial pressure and size predicts mortality in pulmonary arterial hypertension. Chest. 2015;147:198–208.
Ko KY, Wang SY, Yen RF, Shiau YC, Hsu JC, Tsai HY, et al. Clinical significance of quantitative assessment of glucose utilization in patients with ischemic cardiomyopathy. J Nucl Cardiol. 2018. https://doi.org/10.1007/s12350-018-1395-4.
Mäki M, Luotolahti M, Nuutila P, Iida H, Voipio-Pulkki L-M, Ruotsalainen U, et al. Glucose uptake in the chronically dysfunctional but viable myocardium. Circulation. 1996;93:1658–66.
Mannting F, Zabrodina YV, Dass C. Significance of increased right ventricular uptake on 99mTc-sestamibi SPECT in patients with coronary artery disease. J Nucl Med. 1999;40:889–94.
Abraham A, Kass M, Ruddy TD, deKemp RA, Lee AK, Ling MC, et al. Right and left ventricular uptake with Rb-82 PET myocardial perfusion imaging: markers of left main or 3 vessel disease. J Nucl Cardiol. 2010;17:52–60.
Mazraeshahi RM, Striet J, Oeltgen RC, Gerson MC. Myocardial SPECT images for diagnosis of pulmonary hypertension and right ventricular hypertrophy. J Nucl Med Technol. 2010;38:175–80.
Melenovsky V, Andersen MJ, Andress K, Reddy YN, Borlaug BA. Lung congestion in chronic heart failure: haemodynamic, clinical, and prognostic implications. Eur J Heart Fail. 2015;17:1161–71.
Passino C, Sironi AM, Favilli B, Poletti R, Prontera C, Ripoli A, et al. Right heart overload contributes to cardiac natriuretic hormone elevation in patients with heart failure. Int J Cardiol. 2005;104:39–45.
Ritt P, Vija H, Hornegger J, Kuwert T. Absolute quantification in SPECT. Eur J Nucl Med Mol Imaging. 2011;38:S69–77.
Feher A, Sinusas AJ. Quantitative assessment of coronary microvascular function: dynamic single-photon emission computed tomography, positron emission tomography, ultrasound, computed tomography, and magnetic resonance imaging. Circ Cardiovasc Imaging. 2017;10:e006427.
Voelkel NF, Quaife RA, Leinwand LA, Barst RJ, McGoon MD, Meldrum DR, et al. Right ventricular function and failure: report of a National Heart, Lung, and Blood Institute working group on cellular and molecular mechanisms of right heart failure. Circulation. 2006;114:1883–91.
de Keizer B, Scholtens AM, van Kimmenade RRJ, de Jong PA. High FDG uptake in the right ventricular myocardium of a pulmonary hypertension patient. J Am Coll Cardiol. 2013;62:1724.
Drozd K, Ahmadi A, Deng Y, Jiang B, Petryk J, Thorn S, et al. Effects of an endothelin receptor antagonist, Macitentan, on right ventricular substrate utilization and function in a Sugen 5416/hypoxia rat model of severe pulmonary arterial hypertension. J Nucl Cardiol. 2017;24:1979–89.
Vachiery JL, Adir Y, Barbera JA, Champion H, Coghlan JG, Cottin V, et al. Pulmonary hypertension due to left heart diseases. J Am Coll Cardiol. 2013;62:D100–8.
Bokhari S, Raina A, Rosenweig EB, Schulze PC, Bokhari J, Einstein AJ, et al. PET imaging may provide a novel biomarker and understanding of right ventricular dysfunction in patients with idiopathic pulmonary arterial hypertension. Circ Cardiovasc Imaging. 2011;4:641–7.
Ohira H, deKemp R, Pena E, Davies RA, Stewart DJ, Chandy G, et al. Shifts in myocardial fatty acid and glucose metabolism in pulmonary arterial hypertension: a potential mechanism for a maladaptive right ventricular response. Eur Heart J Cardiovasc Imaging. 2016;17:1424–31.
Wu YW, Tadamura E, Yamamuro M, Kanao S, Marui A, Tanabara K, et al. Comparison of contrast-enhanced MRI with (18)F-FDG PET/201Tl SPECT in dysfunctional myocardium: relation to early functional outcome after surgical revascularization in chronic ischemic heart disease. J Nucl Med. 2007;48:1096–103.
Fang W, Zhao L, Xiong CM, Ni XH, He ZX, He JG, et al. Comparison of 18F-FDG uptake by right ventricular myocardium in idiopathic pulmonary arterial hypertension and pulmonary arterial hypertension associated with congenital heart disease. Pulm Circ. 2012;2:365–72.
Gibb AA, Hill BG. Metabolic coordination of physiological and pathological cardiac remodeling. Circ Res. 2018;123:107–28.
Zhang X, Schindler TH, Prior JO, Sayre J, Dahlbom M, Huang SC, et al. Blood flow, flow reserve, and glucose utilization in viable and nonviable myocardium in patients with ischemic cardiomyopathy. Eur J Nucl Med Mol Imaging. 2013;40:532–41.
Gall H, Felix JF, Schneck FK, Milger K, Sommer N, Voswinckel R, et al. The Giessen pulmonary hypertension registry: survival in pulmonary hypertension subgroups. J Heart Lung Transplant. 2017;36:957–67.
van der Bruggen CEE, Tedford RJ, Handoko ML, van der Velden J, de Man FS. RV pressure overload: from hypertrophy to failure. Cardiovasc Res. 2017;113:1423–32.
Puwanant S, Park M, Popovic ZB, Tang WH, Farha S, George D, et al. Ventricular geometry, strain, and rotational mechanics in pulmonary hypertension. Circulation. 2010;121:259–66.
Wu YW, Hsu PY, Lin YH, Cheng MF, Ko CL, Huang YH, et al. Diagnostic and prognostic implications of exercise treadmill and rest first-pass radionuclide angiography in patients with pulmonary hypertension. Clin Nucl Med. 2017;42:e392–9.
Hardegree EL, Sachdev A, Fenstad ER, Villarraga HR, Frantz RP, McGoon MD, et al. Impaired left ventricular mechanics in pulmonary arterial hypertension: identification of a cohort at high risk. Circ Heart Fail. 2013;6:748–55.
Hueb T, Rocha MS, Siqueira SF, Nishioka SADO, Peixoto GL, Saccab MM, et al. Impact of diabetes mellitus on ischemic cardiomyopathy. Five-year follow-up. REVISION-DM trial. Diabetol Metab Syndr. 2018;10:19.
Hu L, Qiu C, Wang X, Xu M, Shao X, Wang Y. The association between diabetes mellitus and reduction in myocardial glucose uptake: a population-based 18F-FDG PET/CT study. BMC Cardiovasc Disord. 2018;18:203.
Hansen MS, Andersen A, Tolbod LP, Hansson NH, Nielsen R, Vonk-Noordegraaf A, et al. Levosimendan improves cardiac function and myocardial efficiency in rats with right ventricular failure. Pulm Circ. 2018;8:2045893217743122.
Shah KS, Xu H, Matsouaka RA, Bhatt DL, Heidenreich PA, Hernandez AF, et al. Heart failure with preserved, borderline, and reduced ejection fraction: 5-year outcomes. J Am Coll Cardiol. 2017;70:2476–86.
Dilsizian V, Bacharach SL, Beanlands RS, Bergmann SR, Delbeke D, Dorbala S, et al. ASNC imaging guidelines/SNMMI procedure standard for positron emission tomography (PET) nuclear cardiology procedures. J Nucl Cardiol. 2016;23:1187–226.
Acknowledgments
The authors thank Ms. Ya-Huang Chen, Ms. Chia-Wen Lai, Mr. Chao-Chun Huang and Mr. Po-Wei Li for dynamic PET acquisition, and Dr. Kuan-Yin Ko, Ms. Yu-Shuan Hung, and Mr. Chien-Yu Chu for their assistance in PET analyses and clinical data collection.
Funding
This study was funded by Ministry of Science and Technology of Taiwan (MOST-101-2314-B-418-012-MY3, MOST-104-2314-B-418-008, MOST-105-2628-B-418-002-MY2, MOST-107-2314-B-418-006-MY3) and Far Eastern Memorial Hospital (FEMH-101-2314-B-418-012-MY3, FEMH-104-2314-B-418-008, FEMH-105-2628-B-418-002-MY2, FEMH-107-2314-B-418-006-MY3).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Research involving human participants and/or animals
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
Except for financially supported by the Ministry of Science and Technology of Taiwan (MOST-101-2314-B-418-012-MY3, MOST-104-2314-B-418-008, MOST-105-2628-B-418-002-MY2, MOST-107-2314-B-418-006-MY3) and Far Eastern Memorial Hospital (FEMH-101-2314-B-418-012-MY3, FEMH-104-2314-B-418-008, FEMH-105-2628-B-418-002-MY2, FEMH-107-2314-B-418-006-MY3), no other relevant potential conflicts of interest exist. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Corresponding author Yen-Wen Wu has received research grants from Ministry of Science and Technology of Taiwan and Far Eastern Memorial Hospital. The other authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardiology
Rights and permissions
About this article
Cite this article
Tsai, SY., Wu, YW., Wang, SY. et al. Clinical significance of quantitative assessment of right ventricular glucose metabolism in patients with heart failure with reduced ejection fraction. Eur J Nucl Med Mol Imaging 46, 2601–2609 (2019). https://doi.org/10.1007/s00259-019-04471-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-019-04471-9