Abstract
Purpose
We analysed a correlation between pre- to post-treatment primary tumour metabolic volume (PT-MV) reduction on 18F-FDG-PET/CT and survival in non-small cell lung cancer (NSCLC) patients treated with chemoradiotherapy (CRT).
Methods
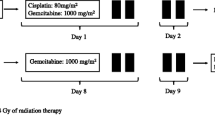
Sixty consecutive patients with NSCLC stage IIIA-B (UICC 7th edition), treated with chemoradiotherapy, who underwent 18F-FDG-PET/CT at the same institution before and 6 weeks after treatment, were analysed. Different metabolic response values were investigated on their correlation with survival parameters: complete response (100% PT-MV reduction); major response (80–99% PT-MV reduction); moderate response (50–79% PT-MV reduction); minor response (1–49% PT-MV reduction) and non-response (no change or increase in uptake).
Results
From 60 patients, 52 (87%) had repeat PET/CT scans 6 weeks after completion of CRT. Complete metabolic response (CR) was reached in ten (17%), whereas major and moderate metabolic responses occurred in 16 (27%) and 15 (25%) patients, respectively. Four patients (7%) had minor metabolic response. Non-response was documented in seven patients (12%). Median overall survival (MS) for the entire cohort was 17 months (95% CI: 11.9–22.1 months). MS according to the different metabolic response values was as follows: 34 months (95% CI: 0–84.1); 22 months (95% CI: 14.2–29.8); 12 months (95% CI: 0.4–23.6); 11 months (95% CI: 0.2–21.8) and 17 months in patients with complete, major, moderate, minor and non-response (95% CI: 6.7–27.3), respectively (p = 0.008).
On multivariate analysis, significant predictors of survival included ECOG performance status (p = 0.035, HR 0.49, 95% CI: 0.25–0.95) as well as complete and major metabolic response as a continuous variable with PT-MV reduction of at least 80% (p = 0.021, HR 0.36, 95% CI: 0.15–0.86). Moderate metabolic response did not correlate with improved outcome (p = 0.522).
Conclusions
In this homogeneous locally-advanced NSCLC single-centre patient cohort, a PT-MV reduction of at least 80% (complete and major metabolic response) following CRT was necessary to significantly improve patient outcome.

Similar content being viewed by others
References
Curran WJJ, Paulus R, Langer CJ, Komaki R, Lee JS, Hauser S, et al. Sequential vs. concurrent chemoradiation for stage III non-small cell lung cancer: randomized phase III trial RTOG 9410. J Natl Cancer Inst. 2011;103:1452–60. United States.
Zhu X, Liao C, Penney BC, Li F, Ferguson MK, Simon CA, et al. Prognostic value of quantitative PET/CT in patients with a nonsmall cell lung cancer and another primary cancer. Nucl Med Commun. 2017;38:185–92. England.
Cremonesi M, Gilardi L, Ferrari ME, Piperno G, Travaini LL, Timmerman R, et al. Role of interim 18F-FDG-PET/CT for the early prediction of clinical outcomes of non-small cell lung cancer (NSCLC) during radiotherapy or chemo-radiotherapy. A systematic review. Eur J Nucl Med Mol Imaging. 2017;44:1915–27. Germany.
Roengvoraphoj O, Wijaya C, Eze C, Li M, Dantes M, Taugner J, et al. Analysis of primary tumor metabolic volume during chemoradiotherapy in locally advanced non-small cell lung cancer. Strahlentherapie und Onkol. 2018;194:107–15.
Pottgen C, Gauler T, Bellendorf A, Guberina M, Bockisch A, Schwenzer N, et al. Standardized uptake decrease on [18F]-Fluorodeoxyglucose positron emission tomography after neoadjuvant chemotherapy is a prognostic classifier for long-term outcome after multimodality treatment: secondary analysis of a randomized trial for Resectable St. J Clin Oncol. 2016;34:2526–33. United States.
Ohri N, Bodner WR, Halmos B, Cheng H, Perez-Soler R, Keller SM, et al. 18F-Fluorodeoxyglucose/positron emission tomography predicts patterns of failure after definitive Chemoradiation therapy for locally advanced non-small cell lung cancer. Int J Radiat Oncol Biol Phys. 2017;97:372–80. United States.
Mattoli MV, Massaccesi M, Castelluccia A, Scolozzi V, Mantini G, Calcagni ML. The predictive value of 18F-FDG PET-CT for assessing the clinical outcomes in locally advanced NSCLC patients after a new induction treatment: low-dose fractionated radiotherapy with concurrent chemotherapy. Radiat Oncol. 2017;12:4. England.
Wald P, Mo X, Barney C, Gunderson D, Haglund AK, Bazan J, et al. Prognostic value of primary tumor volume changes on kV-CBCT during definitive chemoradiotherapy for stage III non-small cell lung cancer. J Thorac Oncol. 2017;12:1779–87. United States.
Roengvoraphoj O, Wijaya C, Eze C, Li M, Dantes M, Taugner J, et al. Analysis of primary tumor metabolic volume during chemoradiotherapy in locally advanced non-small cell lung cancer. Strahlentherapie und Onkol Organ der Dtsch Rontgengesellschaft [et al]. 2017;194:107–15. Germany.
Huber RM, Flentje M, Schmidt M, Pollinger B, Gosse H, Willner J, et al. Simultaneous chemoradiotherapy compared with radiotherapy alone after induction chemotherapy in inoperable stage IIIA or IIIB non-small-cell lung cancer: study CTRT99/97 by the bronchial carcinoma therapy group. J Clin Oncol. 2006;24:4397–404. United States.
Huber RM, Borgmeier A, Flentje M, Willner J, Schmidt M, Manegold C, et al. Concurrent chemoradiation therapy with docetaxel/cisplatin followed by docetaxel consolidation therapy in inoperable stage IIIA/B non-small-cell lung cancer: results of a phase I study. Clin Lung Cancer. 2010;11:45–50. United States.
Flentje M, Huber RM, Engel-Riedel W, Andreas S, Kollmeier J, Staar S, et al. GILT-A randomised phase III study of oral vinorelbine and cisplatin with concomitant radiotherapy followed by either consolidation therapy with oral vinorelbine and cisplatin or best supportive care alone in stage III non-small cell lung cancer. Strahlentherapie und Onkol Organ der Dtsch Rontgengesellschaft. [et al]. 2016;192:216–22.
Huang W, Zhou T, Ma L, Sun H, Gong H, Wang J, et al. Standard uptake value and metabolic tumor volume of (1)(8)F-FDG PET/CT predict short-term outcome early in the course of chemoradiotherapy in advanced non-small cell lung cancer. Eur J Nucl Med Mol Imaging. 2011;38:1628–35. Germany.
Wahl RL, Jacene H, Kasamon Y, Lodge MA. From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med. 2009;50(Suppl 1):122S–50S. United States.
Wang W-W, Wang S-J, Zhou Z-R. Did dose escalated radiotherapy in stage III non-small cell lung cancer improve overall survival. J Thorac Dis. 2016;8:3338–42.
Senan S, Brade A, Wang L-H, Vansteenkiste J, Dakhil S, Biesma B, et al. PROCLAIM: randomized phase III trial of pemetrexed-cisplatin or etoposide-cisplatin plus thoracic radiation therapy followed by consolidation chemotherapy in locally advanced nonsquamous non-small-cell lung cancer. J Clin Oncol. 2016;34:953–62. United States.
Liang J, Bi N, Wu S, Chen M, Lv C, Zhao L, et al. Etoposide and cisplatin versus paclitaxel and carboplatin with concurrent thoracic radiotherapy in unresectable stage III non-small cell lung cancer: a multicenter randomized phase III trial. Ann Oncol Off J Eur Soc Med Oncol. 2017;28:777–83. England.
Bradley JD, Paulus R, Komaki R, Masters G, Blumenschein G, Schild S, et al. Standard-dose versus high-dose conformal radiotherapy with concurrent and consolidation carboplatin plus paclitaxel with or without cetuximab for patients with stage IIIA or IIIB non-small-cell lung cancer (RTOG 0617): a randomised, two-by-two factorial p. Lancet Oncol. 2015;16:187–99. England.
Vokes EE, Herndon JE 2nd, Kelley MJ, Cicchetti MG, Ramnath N, Neill H, et al. Induction chemotherapy followed by chemoradiotherapy compared with chemoradiotherapy alone for regionally advanced unresectable stage III non-small-cell lung cancer: cancer and leukemia group B. J Clin Oncol. 2007;25:1698–704. United States.
Hanna N, Neubauer M, Yiannoutsos C, McGarry R, Arseneau J, Ansari R, et al. Phase III study of cisplatin, etoposide, and concurrent chest radiation with or without consolidation docetaxel in patients with inoperable stage III non-small-cell lung cancer: the Hoosier oncology group and U.S. oncology. J Clin Oncol. 2008;26:5755–60. United States.
Antonia SJ, Villegas A, Daniel D, Vicente D, Murakami S, Hui R, et al. Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. N Engl J Med. 2017;377:1919–29. United States.
Frood R, Prestwich R, Tsoumpas C, Murray P, Franks K, Scarsbrook A. Effectiveness of respiratory-gated positron emission tomography/computed tomography for radiotherapy planning in patients with lung carcinoma - a systematic review. Clin Oncol (R Coll Radiol). 2018;30:225–32. England.
Acknowledgments
Presented in part as a poster discussion at the European Lung Cancer Conference (ELCC) 2017, Geneva, Switzerland, 05–08 May 2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Disclosure
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Rudolf Maria Huber, Claus Belka and Farkhad Manapov are members of the German Centre for Lung Research (DZL CPC-M)
Rights and permissions
About this article
Cite this article
Roengvoraphoj, O., Eze, C., Wijaya, C. et al. How much primary tumor metabolic volume reduction is required to improve outcome in stage III NSCLC after chemoradiotherapy? A single-centre experience. Eur J Nucl Med Mol Imaging 45, 2103–2109 (2018). https://doi.org/10.1007/s00259-018-4063-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-4063-7