Abstract
Purpose
To assess the localizing value of 18F-FDG PET in patients operated on for drug-resistant epilepsy due to focal cortical dysplasia type 2 (FCD2).
Methods
We analysed 18F-FDG PET scans from 103 consecutive patients (52 males, 7–65 years old) with histologically proven FCD2. PET and MRI data were first reviewed by visual analysis blinded to clinical information and FCD2 location. The additional value of electroclinical data and PET/MRI coregistration was assessed by comparison with pathological results and surgical outcomes.
Results
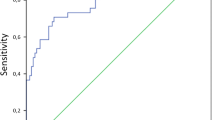
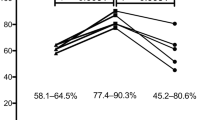
Visual analysis of PET scans showed focal or regional hypometabolism corresponding to the FCD2 in 45 patients (44%), but the findings were doubtful or misleading in 37 patients and negative in 21. When considering electroclinical data, positive localization was obtained in 73 patients, and this increased to 85 (83%) after coregistration of PET and MRI data. Under the same conditions, MRI was positive in 61 patients (59%), doubtful in 15 and negative in 27. The additional value of PET was predominant in patients negative or doubtful on MRI, localizing the FCD2 in 35 patients (83%). Interobserver agreement correlated with the grade of hypometabolism: it was good in patients with mild to severe hypometabolism (82–95%), but moderate in those with subtle/doubtful hypometabolism (45%). The main factors influencing positive PET localization were the grade of hypometabolism and the size of the FCD2 (P < 0.0001). Misleading location (nine patients) was associated with a small FCD2 in the mesial frontal and central regions. Following limited cortical resection mainly located in extratemporal areas (mean follow-up 5.6 years), a seizure-free outcome was achieved in 94% of patients, including Engel’s class IA in 72%.
Conclusion
In this series, 18F-FDG PET contributed to the localization of FCD2 in 83% of patients. This high localizing value was obtained by integration of electroclinical data and PET/MRI coregistration. This approach may help improve the surgical outcome in extratemporal epilepsy, even in patients negative on MRI.






Similar content being viewed by others
Change history
28 April 2018
The original version of this article has added numbers in the text which are unnecessary. Correct line should be: “We also performed PET/MRI based surgical resections in an increasing number of MRI negative/ doubtful cases with favourable outcome.”
References
Blumcke I, Spreafico R, Haaker G, Coras R, Kobow K, Bien CG, et al. Histopathological findings in brain tissue obtained during epilepsy surgery. N Engl J Med. 2017;377:1648–56.
Ryvlin P, Cross JH, Rheims S. Epilepsy surgery in children and adults. Lancet Neurol. 2014;13:1114–26.
Guerrini R, Duchowny M, Jayakar P, Krsek P, Kahane P, Tassi L, et al. Diagnostic methods and treatment options for focal cortical dysplasia. Epilepsia. 2015;56:1669–86.
Chassoux F, Rodrigo S, Semah F, Beuvon F, Landré E, Devaux B, et al. FDG-PET improves surgical outcome in negative-MRI Taylor type focal cortical dysplasias. Neurology. 2010;75:2168–75.
Rubí S, Setoain X, Donaire A, Bargalló N, Sanmartí F, Carreño M, et al. Validation of FDG-PET/MRI coregistration in nonlesional refractory childhood epilepsy. Epilepsia. 2011;52:2216–24.
Chassoux F, Landre E, Mellerio C, Turak B, Mann MW, Daumas-Duport C, et al. Type II focal cortical dysplasia: electro-clinical phenotypes and surgical outcome related to imaging. Epilepsia. 2012;53:349–58.
Blümcke I, Thom M, Aronica E, Armstrong DD, Vinters HV, Palmini A, et al. The clinicopathologic spectrum of focal cortical dysplasias: a consensus classification proposed by an ad hoc Task Force of the ILAE Diagnostic Methods Commission. Epilepsia. 2011;52:158–74.
Engel J Jr, Van Ness PC, Rasmussen TB, Ojemann LM. Outcome with respect to epileptic seizures. In: Engel J Jr, editor. Surgical treatment of the epilepsies. 2nd ed. New York: Raven; 1993. p. 609–21.
Mellerio C, Labeyrie MA, Chassoux F, Daumas-Duport C, Landre E, Turak B, et al. Optimizing MR imaging detection of type 2 focal cortical dysplasia: best criteria for clinical practice. AJNR Am J Neuroradiol. 2012;33:1932–8.
Rivière D, Geffroy D, Denghien I, Souedet N, Cointepas Y. BrainVISA: an extensible software environment for sharing multimodal neuroimaging data and processing tools. In: Proceedings of the 15th Annual Meeting of the Organization for Human Brain Mapping, 18–23 June 2009, San Francisco, California. http://brainvisa.info.
Chassoux F, Devaux B, Landre E, Turak B, Nataf F, Varlet P, et al. Stereo-electroencephalography in focal cortical dysplasia: a 3D approach to delineating the dysplastic cortex. Brain. 2000;123:1733–51.
Lee SK, Choe G, Hong KS, Nam HW, Kim JY, Chung CK, et al. Neuroimaging findings of cortical dyslamination with cytomegaly. Epilepsia. 2001;42:850–6.
Kim YK, Lee DS, Lee SK, Chung CK, Chung JK, Lee MC. (18)F-FDG PET in localization of frontal lobe epilepsy: comparison of visual and SPM analysis. J Nucl Med. 2002;43:1167–74.
Knowlton RC, Elgavish RA, Bartolucci A, Ojha B, Limdi N, Blount J, et al. Functional imaging: II. Prediction of epilepsy surgery outcome. Ann Neurol. 2008;64:35–41.
Salamon N, Kung J, Shaw SJ, Koo J, Koh S, Wu JY, et al. FDG-PET/MRI coregistration improves detection of cortical dysplasia in patients with epilepsy. Neurology. 2008;71:1594–601.
Paldino MJ, Yang E, Jones JY, Mahmood N, Sher A, Zhang W. Comparison of the diagnostic accuracy of PET/MRI to PET/CT-acquired FDG brain exams for seizure focus detection: a prospective study. Pediatr Radiol. 2017;47:1500–7.
Urbach H, Scheffler B, Heinrichsmeier T, von Oertzen J, Kral T, Wellmer J, et al. Focal cortical dysplasia of Taylor's balloon cell type: a clinicopathological entity with characteristic neuroimaging and histopathological features, and favorable postsurgical outcome. Epilepsia. 2002;43:33–40.
Besson P, Andermann F, Dubeau F, Bernasconi A. Small focal cortical dysplasia lesions are located at the bottom of a deep sulcus. Brain. 2008;13:3246–55.
Wagner J, Weber B, Urbach H, Elger CE, Huppertz HJ. Morphometric MRI analysis improves detection of focal cortical dysplasia type II. Brain. 2011;134:2844–54.
Mellerio C, Labeyrie MA, Chassoux F, Roca P, Alami O, Plat M, et al. 3T MRI improves the detection of transmantle sign in type 2 focal cortical dysplasia. Epilepsia. 2014;55:117–22.
Hong SJ, Kim H, Schrader D, Bernasconi N, Bernhardt BC, Bernasconi A. Automated detection of cortical dysplasia type II in MRI-negative epilepsy. Neurology. 2014;83:48–55.
Mellerio C, Roca P, Chassoux F, Danière F, Cachia A, Lion S, et al. The power button sign: a newly described central sulcal pattern on surface rendering MR images of type 2 focal cortical dysplasia. Radiology. 2015;274:500–7.
Roca P, Mellerio C, Chassoux F, Rivière D, Cachia A, Charron S, et al. Sulcus-based MR analysis of focal cortical dysplasia located in the central region. PLoS One. 2015;10:e0122252.
Colombo N, Tassi L, Deleo F, Citterio A, Bramerio M, Mai R, et al. Focal cortical dysplasia type IIa and IIb: MRI aspects in 118 cases proven by histopathology. Neuroradiology. 2012;54:1065–77.
Chassoux F, Navarro V, Catenoix H, Valton L, Vignal JP. Planning and management of SEEG. Neurophysiol Clin. 2018;48:25–37.
Rathore C, Dickson JC, Teotónio R, Ell P, Duncan JS. The utility of 18F-fluorodeoxyglucose PET (FDG PET) in epilepsy surgery. Epilepsy Res. 2014;108:1306–14.
Rubinger L, Chan C, D'Arco F, Moineddin R, Muthaffar O, Rutka JT, et al. Change in presurgical diagnostic imaging evaluation affects subsequent pediatric epilepsy surgery outcome. Epilepsia. 2016;57:32–40.
Lee SK, Lee SY, Kim KK, Hong KS, Lee DS, Chung CK. Surgical outcome and prognostic factors of cryptogenic neocortical epilepsy. Ann Neurol. 2005;58:525–32.
Chapman K, Wyllie E, Najm I, Ruggieri P, Bingaman W, Lüders J, et al. Seizure outcome after epilepsy surgery in patients with normal preoperative MRI. J Neurol Neurosurg Psychiatry. 2005;76:710–3.
Krsek P, Maton B, Jayakar P, Dean P, Korman B, Rey G, et al. Incomplete resection of focal cortical dysplasia is the main predictor of poor postsurgical outcome. Neurology. 2009;72:217–23.
Widdess-Walsh P, Jeha L, Nair D, Kotagal P, Bingaman W, Najm I. Subdural electrode analysis in focal cortical dysplasia: predictors of surgical outcome. Neurology. 2007;69:660–7.
Tassi L, Colombo N, Garbelli R, Francione S, Lo Russo G, Mai R, et al. Focal cortical dysplasia: neuropathological subtypes, EEG, neuroimaging and surgical outcome. Brain. 2002;125:1719–32.
Fauser S, Schulze-Bonhage A, Honegger J, Carmona H, Huppertz HJ, Pantazis G, et al. Focal cortical dysplasias: surgical outcome in 67 patients in relation to histological subtypes and dual pathology. Brain. 2004;127:2406–18.
Kim DW, Lee SK, Chu K, Park KI, Lee SY, Lee CH, et al. Predictors of surgical outcome and pathologic considerations in focal cortical dysplasia. Neurology. 2009;72:211–6.
Harvey AS, Mandelstam SA, Maixner WJ, Leventer RJ, Semmelroch M, MacGregor D, et al. The surgically remediable syndrome of epilepsy associated with bottom-of-sulcus dysplasia. Neurology. 2015;84:2021–8.
Archambaud F, Bouilleret V, Hertz-Pannier L, Chaumet-Riffaud P, Rodrigo S, Dulac O, et al. Optimizing statistical parametric mapping analysis of 18F-FDG PET in children. EJNMMI Res. 2013;3:2.
Mendes Coelho VC, Morita ME, Amorim BJ, Ramos CD, Yasuda CL, Tedeschi H, et al. Automated online quantification method for 18F-FDG positron emission tomography/CT improves detection of the epileptogenic zone in patients with pharmacoresistant epilepsy. Front Neurol. 2017;8:453.
Mayoral M, Marti-Fuster B, Carreño M, Carrasco JL, Bargalló N, Donaire A, et al. Seizure-onset zone localization by statistical parametric mapping in visually normal (18)F-FDG-PET studies. Epilepsia. 2016;57:1236–44.
Tan YL, Kim H, Lee S, Tihan T, Ver Hoef L, Mueller SG, et al. Quantitative surface analysis of combined MRI and PET enhances detection of focal cortical dysplasias. Neuroimage. 2018;166:10–8.
van't Klooster MA, Huiskamp G, Zijlmans M, Debets RM, Comans EF, Bouvard S, et al. Can we increase the yield of FDG-PET in the preoperative work-up for epilepsy surgery? Epilepsy Res. 2014;108:1095–105.
Acknowledgments
The authors thank the team of SHFJ, Patrick Bodilis, Christine Baron, Brigitte Jouve, Vincent Brulon, Philippe Gervais and Thierry Le Kieffre, for performing the PET scans.
Author information
Authors and Affiliations
Contributions
All authors were involved in drafting and revising the article.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the principles of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
The original version of this article was revised: There were added numbers in the text which are unnecessary. Correct line should be: “We also performed PET/MRI based surgical resections in an increasing number of MRI negative/ doubtful cases with favourable outcome.”
Rights and permissions
About this article
Cite this article
Desarnaud, S., Mellerio, C., Semah, F. et al. 18F-FDG PET in drug-resistant epilepsy due to focal cortical dysplasia type 2: additional value of electroclinical data and coregistration with MRI. Eur J Nucl Med Mol Imaging 45, 1449–1460 (2018). https://doi.org/10.1007/s00259-018-3994-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-3994-3