Abstract
Purpose
To evaluate the ability of CT and PET radiomics features to classify lung lesions as primary or metastatic, and secondly to differentiate histological subtypes of primary lung cancers.
Methods
A cohort of 534 patients with lung lesions were retrospectively studied. Radiomics texture features were extracted using the LIFEx package from semiautomatically segmented PET and CT images. Histology data were recorded in all patients. The patient cohort was divided into a training and a validation group and linear discriminant analysis (LDA) was performed to classify the lesions using both direct and backward stepwise methods. The robustness of the procedure was tested by repeating the entire process 100 times with different assignments to the training and validation groups. Scoring metrics included analysis of the receiver operating characteristic curves in terms of area under the curve (AUC), sensitivity, specificity and accuracy.
Results
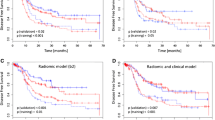
Radiomics features extracted from CT and PET datasets were able to differentiate primary tumours from metastases in both the training and the validation group (AUCs 0.79 ± 0.03 and 0.70 ± 0.04, respectively, from the CT dataset; AUCs 0.92 ± 0.01 and 0.91 ± 0.03, respectively, from the PET dataset). The AUC cut-off thresholds identified by LDA using direct and backward elimination strategies were −0.79 ± 0.06 and −0.81 ± 0.08, respectively (CT dataset) and −0.69 ± 0.05 and −0.68 ± 0.04, respectively (PET dataset). For differentiation between primary subgroups based on CT features, the AUCs in the training and validation groups were 0.81 ± 0.02 and 0.69 ± 0.04 for adenocarcinoma (Adc) vs. squamous cell carcinoma (Sqc) or “Other”, 0.85 ± 0.02 and 0.70 ± 0.05 for Sqc vs. Adc or Other, and 0.77 ± 0.03 and 0.57 ± 0.05 for Other vs. Adc or Sqc. The same analyses for the PET data revealed AUCs of 0.90 ± 0.10 and 0.80 ± 0.04, 0.80 ± 0.02 and 0.61 ± 0.06, and 0.97 ± 0.01 and 0.88 ± 0.04, respectively.
Conclusion
PET radiomics features were able to differentiate between primary and metastatic lung lesions and showed the potential to identify primary lung cancer subtypes.




Similar content being viewed by others
References
Sim YT, Poon FW. Imaging of solitary pulmonary nodule – a clinical review. Quant Imaging Med Surg. 2013;3:316–26.
van Gómez López O, García Vicente AM, Honguero Martínez AF, Jiménez Londoño GA, Vega Caicedo CH, León Atance P, et al. (18)F-FDG-PET/CT in the assessment of pulmonary solitary nodules: comparison of different analysis methods and risk variables in the prediction of malignancy. Transl Lung Cancer Res. 2015;4:228–35.
Ruilong Z, Daohai X, Li G, Xiaohong W, Chunjie W, Lei T. Diagnostic value of 18F-FDG-PET/CT for the evaluation of solitary pulmonary nodules: a systematic review and meta-analysis. Nucl Med Commun. 2017;38:67–75.
Dabrowska M, Krenke R, Korczynski P, Maskey-Warzechowska M, Zukowska M, Kunikowska J, et al. Diagnostic accuracy of contrast-enhanced computed tomography and positron emission tomography with 18-FDG in identifying malignant solitary pulmonary nodules. Medicine (Baltimore). 2015;94:e666.
Kikano GE, Fabien A, Schilz R. Evaluation of the solitary pulmonary nodule. Am Fam Phys. 2015;92:1084–91.
Leong PP, Rezai B, Koch WM, Reed A, Eisele D, Lee DJ, et al. Distinguishing second primary tumors from lung metastases in patients with head and neck squamous cell carcinoma. J Natl Cancer Inst. 1998;90:972–7.
Askin FB. Something old? Something new? Second primary or pulmonary metastasis in the patient with known extrathoracic carcinoma. Am J Clin Pathol. 1993;100:4–5.
Adkins PC, Wesselhoeft CW, Newman W, Blades B. Thoracotomy on the patient with previous malignancy: metastasis or new primary? J Thorac Cardiovasc Surg. 1968;56:351–61.
Shepherd MP. Thoracic metastases. Thorax. 1982;37:366–70.
Perandini S, Soardi GA, Motton M, Augelli R, Dallaserra C, Puntel G, et al. Enhanced characterization of solid solitary pulmonary nodules with Bayesian analysis-based computer-aided diagnosis. World J Radiol. 2016;8:729–34.
Choi EJ, Jin GY, Han YM, Lee YS, Kweon KS. Solitary pulmonary nodule on helical dynamic CT scans: analysis of the enhancement patterns using a computer-aided diagnosis (CAD) system. Korean J Radiol. 2008;9:401–8.
Rubin GD, Lyo JK, Paik DS, Sherbondy AJ, Chow LC, Leung AN, et al. Pulmonary nodules on multi-detector row CT scans: performance comparison of radiologists and computer-aided detection. Radiology. 2005;234:274–83.
Way TW, Hadjiiski LM, Sahiner B, Chan H-P, Cascade PN, Kazerooni EA, et al. Computer-aided diagnosis of pulmonary nodules on CT scans: segmentation and classification using 3D active contours. Med Phys. 2006;33:2323–37.
Swensen SJ, Silverstein MD, Edell ES, Trastek VF, Aughenbaugh GL, Ilstrup DM, et al. Solitary pulmonary nodules: clinical prediction model versus physicians. Mayo Clin Proc. 1999;74:319–29.
Chen B, Zhang R, Gan Y, Yang L, Li W. Development and clinical application of radiomics in lung cancer. Radiat Oncol. 2017;12:154.
Miwa K, Inubushi M, Wagatsuma K, Nagao M, Murata T, Koyama M, et al. FDG uptake heterogeneity evaluated by fractal analysis improves the differential diagnosis of pulmonary nodules. Eur J Radiol. 2014;83:715–9.
Dennie C, Thornhill R, Sethi-Virmani V, Souza CA, Bayanati H, Gupta A, et al. Role of quantitative computed tomography texture analysis in the differentiation of primary lung cancer and granulomatous nodules. Quant Imaging Med Surg. 2016;6:6–15.
Chen S, Harmon S, Perk T, Li X, Chen M, Li Y, et al. Diagnostic classification of solitary pulmonary nodules using dual time 18 F-FDG PET/CT image texture features in granuloma-endemic regions. Sci Rep. 2017;7:9370.
Nguyen P, Bashirzadeh F, Hundloe J, Salvado O, Dowson N, Ware R, et al. Grey scale texture analysis of endobronchial ultrasound mini probe images for prediction of benign or malignant aetiology. Respirology. 2015;20:960–6.
Zwanenburg A, Leger S, Vallières M, Löck S; Image Biomarker Standardisation Initiative. Image biomarker standardisation initiative (arXiv:1612.07003). Cornell University Library: arXiv. http://arxiv.org/abs/1612.07003
Boellaard R, Delgado-Bolton R, Oyen WJ, Giammarile F, Tatsch K, Eschner W, et al. FDG PET/CT: EANM procedure guidelines for tumour imaging: version 2.0. Eur J Nucl Med Mol Imaging. 2014;42:328–54.
Nicole C, Orlhac F, Boughdad S, Reuze S, Soussan M, Robert C, et al. A freeware for tumor heterogeneity characterization in PET, SPECT, CT, MRI and US to accelerate advances in radiomics [abstract]. J Nucl Med. 2017;58:1316.
MacMahon H, Naidich DP, Goo JM, Lee KS, Leung ANC, Mayo JR, et al. Guidelines for management of incidental pulmonary nodules detected on CT images: from the Fleischner Society 2017. Radiology. 2017;284:228–43.
Petrella F, Diotti C, Rimessi A, Spaggiari L. Pulmonary metastasectomy: an overview. J Thorac Dis. 2017;9:1291–8.
Sollini M, Cozzi L, Antunovic L, Chiti A, Kirienko M. PET Radiomics in NSCLC: state of the art and a proposal for harmonization of methodology. Sci Rep. 2017;7:358.
Ha S, Choi H, Cheon GJ, Kang KW, Chung JK, Kim EE, et al. Autoclustering of non-small cell lung carcinoma subtypes on 18F-FDG PET using texture analysis: a preliminary result. Nucl Med Mol Imaging. 2014;48:278–86.
Kim D-H, Jung J, Son SH, Kim C-Y, Hong CM, Oh J-R, et al. Prognostic significance of Intratumoral metabolic heterogeneity on 18F-FDG PET/CT in pathological N0 non-small cell lung cancer. Clin Nucl Med. 2015;40:708–14.
Kirienko M, Gallivanone F, Sollini M, Veronesi G, Voulaz E, Antunovic L, et al. FDG PET/CT as theranostic imaging in diagnosis of non-small cell lung cancer. Front Biosci (Landmark Ed). 2017;22:1713–23.
Aerts HJ, Velazquez ER, Leijenaar RT, Parmar C, Grossmann P, Carvalho S, et al. Decoding tumour phenotype by noninvasive imaging using a quantitative radiomics approach. Nat Commun. 2014;5:4006.
Budiawan H, Cheon GJ, Im HJ, Lee SJ, Paeng JC, Kang KW, et al. Heterogeneity analysis of 18F-FDG uptake in differentiating between metastatic and inflammatory lymph nodes in adenocarcinoma of the lung: comparison with other parameters and its application in a clinical setting. Nucl Med Mol Imaging. 2013;47:232–41.
Flechsig P, Frank P, Kratochwil C, Antoch G, Rath D, Moltz J, et al. Radiomic analysis using density threshold for FDG-PET/CT-based N-staging in lung cancer patients. Mol Imaging Biol. 2017;19:315–22.
Giesel FL, Schneider F, Kratochwil C, Rath D, Moltz J, Holland-Letz T, et al. Correlation between SUVmax and CT radiomic analysis using lymph node density in PET/CT-based lymph node staging. J Nucl Med. 2017;58:282–7.
Wang H, Zhou Z, Li Y, Chen Z, Lu P, Wang W, et al. Comparison of machine learning methods for classifying mediastinal lymph node metastasis of non-small cell lung cancer from 18F-FDG PET/CT images. EJNMMI Res. 2017;7:11.
Craigie M, Squires J, Miles K. Can CT measures of tumour heterogeneity stratify risk for nodal metastasis in patients with non-small cell lung cancer? Clin Radiol. 2017;72:899.e1–7.
Gao X, Chu C, Li Y, Lu P, Wang W, Liu W, et al. The method and efficacy of support vector machine classifiers based on texture features and multi-resolution histogram from 18F-FDG PET-CT images for the evaluation of mediastinal lymph nodes in patients with lung cancer. Eur J Radiol. 2015;84:312–7.
Kirienko M, Gallivanone F, Sollini M, Veronesi G, Voulaz E, Antunovic L, et al. Texture analysis of FDG-PET/CT images to characterize lung cancer lesions and to predict outcome in patients undergoing primary surgery: preliminary results. Eur J Nucl Med Mol Imaging. 2016;43:306.
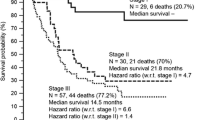
Kirienko M, Cozzi L, Antunovic L, Lozza L, Fogliata A, Voulaz E, et al. Prediction of disease-free survival by the PET/CT radiomic signature in non-small cell lung cancer patients undergoing surgery. Eur J Nucl Med Mol Imaging. 2018;45:207–17.
Zhu A, Lee D, Shim H. Metabolic PET imaging in cancer detection and therapy response. Semin Oncol. 2011;38:55–69.
Lambin P, Leijenaar RTH, Deist TM, Peerlings J, de Jong EEC, van Timmeren J, et al. Radiomics: the bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol. 2017;14:749–62.
Acknowledgments
We thank Elena Vanni for support in patient selection; Paola Bossi and Dahoud Rahal for collaboration in pathological analyses; Marco Alloisio, Giulia Veronesi and the Thoracic Surgery Unit for close collaboration in patient selection and follow-up; Lorenzo Leonardi for image processing; and Riccardo Muglia, Nicolò Gennaro and Orazio Giuseppe Santonocito for their help in patient selection. Tommaso Cozzi is acknowledged for support in the processing of radiomics features. M.K. is supported by an AIRC (Italian Association for Cancer Research) scholarship funded by a grant won by A.C. (IG-2016-18585).
Author information
Authors and Affiliations
Contributions
M.S., M.K. and A.C. conceived the idea of the study; L.C. and A.F. performed the statistical analysis; E.V. collected the data and selected the patients; M.S., M.K. and L.A. reviewed and segmented the images; L.C. performed the radiomics image analysis; M.S., M.K. and L.C. wrote the manuscript; A.R. edited and reviewed the manuscript.
All the authors discussed the results and commented on the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
A. Chiti received speaker honoraria from General Electric and Sirtex Medical System, acted as scientific advisor to Blue Earth Diagnostics and Advanced Accelerator Applications, and benefited from an unconditional grant from Sanofi to Humanitas University. All honoraria and grants are outside the scope of the submitted work.
L. Cozzi acts as Scientific Advisor to Varian Medical Systems. All honoraria are outside the scope of the submitted work.
M. Kirienko is supported by an AIRC (Italian Association for Cancer Research) scholarship funded by a grant won by A.C. (IG-2016-18,585).
All other authors have no conflicts of interest.
Ethical approval
The study was approved by the institutional Ethics Committee. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the principles of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
For this type of study (i.e. retrospective), formal consent was not required.
Rights and permissions
About this article
Cite this article
Kirienko, M., Cozzi, L., Rossi, A. et al. Ability of FDG PET and CT radiomics features to differentiate between primary and metastatic lung lesions. Eur J Nucl Med Mol Imaging 45, 1649–1660 (2018). https://doi.org/10.1007/s00259-018-3987-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-3987-2