Abstract
Purpose
Since the introduction of 68Ga-PSMA-11 PET/CT for imaging prostate cancer (PC) we have frequently observed mediastinal lymph nodes (LN) showing tracer uptake despite being classified as benign. The aim of this evaluation was to further analyze such LN.
Methods
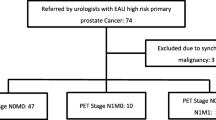
Two patient groups with biphasic 68Ga-PSMA-11 PET/CT at 1 h and 3 h p.i. were included in this retrospective evaluation. Group A (n = 38) included patients without LN metastases, and group B (n = 43) patients with LN metastases of PC. SUV of mediastinal/paraaortal LN of group A (n = 100) were compared to SUV of LN metastases of group B (n = 91). Additionally, 22 randomly selected mediastinal and paraaortal LN of patients without PC were immunohistochemically (IHC) analyzed for PSMA expression.
Results
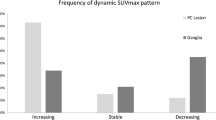
In group A, 7/38 patients (18.4%) presented with at least one PSMA-positive mediastinal LN at 1 h p.i. and 3/38 (7.9%) positive LN at 3 h p.i. with a SUVmax of 2.3 ± 0.7 at 1 h p.i. (2.0 ± 0.7 at 3 h p.i.). A total of 11 PSMA-positive mediastinal/paraaortal LN were detected in nine patients considering both imaging timing points. SUVmax of LN-metastases was 12.5 ± 13.2 at 1 h p.i. (15.8 ± 17.0 at 3 h p.i.). SUVmax increased clearly (> 10%) between 1 h and 3 h p.i. in 76.9% of the LN metastases, and decreased significantly in 72.7% of the mediastinal/paraaortal LN. By IHC, PSMA-expression was observed in intranodal vascular endothelia of all investigated LN groups and to differing degrees within germinal centers of 15/22 of them (68.1%). Expression was stronger in mediastinal nodes (p = 0.038) and when follicular hyperplasia was present (p = 0.050).
Conclusion
PSMA-positive mediastinal/paraaortal benign LN were visible in a notable proportion of patients. PSMA-positivity on the histopathological level was associated with the activation state of the LN. However, in contrast to LN metastases of PC, they presented with significantly lower uptake, which, in addition, usually decreased over time.










Similar content being viewed by others
References
Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics. CA Cancer J Clin. 2014;64:9–29.
Israeli RS, Powell CT, Corr JG, Fair WR, Heston WD. Expression of the prostate-specific membrane antigen. Cancer Res. 1994;54:1807–11.
Maresca KP, Hillier SM, Femia FJ, Keith D, Barone C, Joyal JL, et al. A series of halogenated heterodimeric inhibitors of prostate specific membrane antigen (PSMA) as radiolabeled probes for targeting prostate cancer. J Med Chem. 2009;52:347–57.
Hillier SM, Maresca KP, Femia FJ, Marquis JC, Foss CA, Nguyen N, et al. Preclinical evaluation of novel glutamate–urea–lysine analogues that target prostate-specific membrane antigen as molecular imaging pharmaceuticals for prostate cancer. Cancer Res. 2009;69:6932–40.
Afshar-Oromieh A, Malcher A, Eder M, Eisenhut M, Linhart HG, Hadaschik BA, et al. PET imaging with a [68Ga]gallium-labelled PSMA-ligand for the diagnosis of prostate cancer: biodistribution in humans and first evaluation of tumour lesions. Eur J Nucl Med Mol Imaging. 2013;40:486–95.
Afshar-Oromieh A, Zechmann CM, Malcher A, Eder M, Eisenhut M, Linhart HG, et al. Comparison of PET imaging with a (68)Ga-labelled PSMA-ligand and (18)F-choline-based PET/CT for the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2014;41:11–20.
Afshar-Oromieh A, Avtzi E, Giesel FL, Holland-Letz T, Linhart HG, Eder M, et al. The diagnostic value of PET/CT imaging with the (68)Ga-labelled PSMA-ligand HBED-CC in the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2015;42:197–209.
Eiber M, Maurer T, Souvatzoglou M, Beer AJ, Ruffani A, Haller B, et al. Evaluation of hybrid 68Ga-PSMA-ligand PET/CT in 248 patients with biochemical recurrence after radical prostatectomy. J Nucl Med. 2015;56:668–74.
Afshar-Oromieh A, Holland-Letz T, Giesel FL, Kratochwil C, Mier W, Haufe S, et al. Diagnostic performance of (68)Ga-PSMA-11 (HBED-CC) PET/CT in patients with recurrent prostate cancer: evaluation in 1007 patients. Eur J Nucl Med Mol Imaging. 2017:44(8):1258–68.
Zechmann CM, Afshar-Oromieh A, Armor T, Stubbs JB, Mier W, Hadaschik B, et al. Radiation dosimetry and first therapy results with a (124)I/ (131)I-labeled small molecule (MIP-1095) targeting PSMA for prostate cancer therapy. Eur J Nucl Med Mol Imaging. 2014;41:1280–92.
Afshar-Oromieh A, Haberkorn U, Zechmann C, Armor T, Mier W, Spohn F, et al. Repeated PSMA-targeting radioligand therapy of metastatic prostate cancer with (131)I-MIP-1095. Eur J Nucl Med Mol Imaging. 2017;44:950–9.
Chang SS. Overview of prostate-specific membrane antigen. Rev Urol. 2004;6(Suppl 10):S13–8.
Sheikhbahaei S, Afshar-Oromieh A, Eiber M, Solnes LB, Javadi MS, Ross AE, et al. Pearls and pitfalls in clinical interpretation of prostate-specific membrane antigen (PSMA)-targeted PET imaging. Eur J Nucl Med Mol Imaging. 2017;44(12):2117–36
Krohn T, Verburg FA, Pufe T, Neuhuber W, Vogg A, Heinzel A, et al. 68Ga-PSMA-HBED uptake mimicking lymph node metastasis in coeliac ganglia: an important pitfall in clinical practice. Eur J Nucl Med Mol Imaging. 2015;42:210–4.
Afshar-Oromieh A, Hetzheim H, Kübler W, Kratochwil C, Giesel FL, Hope TA, et al. Radiation dosimetry of (68)Ga-PSMA-11 (HBED-CC) and preliminary evaluation of optimal imaging timing. Eur J Nucl Med Mol Imaging. 2016;43:1611–20.
Eder M, Neels O, Müller M, Bauder-Wüst U, Remde Y, Schäfer M, et al. Novel preclinical and radiopharmaceutical aspects of [68Ga]Ga-PSMA-HBED-CC: a new PET tracer for imaging of prostate cancer. Pharm Basel Switz. 2014;7:779–96.
Herrmann K, Bluemel C, Weineisen M, Schottelius M, Wester H-J, Czernin J, et al. Biodistribution and radiation dosimetry for a probe targeting prostate-specific membrane antigen for imaging and therapy. J Nucl Med. 2015;56:855–61.
Afshar-Oromieh A, Hetzheim H, Kratochwil C, Benesova M, Eder M, Neels OC, et al. The theranostic PSMA-ligand PSMA-617 in the diagnosis of prostate cancer by PET/CT: biodistribution in humans, radiation dosimetry, and first evaluation of tumor lesions. J Nucl Med. 2015;56:1697–705.
Afshar-Oromieh A, Sattler LP, Mier W, Hadaschik B, Debus J, Holland-Letz T, et al. The clinical impact of additional late PET/CT imaging with 68Ga-PSMA-11 (HBED-CC) in the diagnosis of prostate cancer. J Nucl Med. 2017;58(5):750–755
Sahlmann C-O, Meller B, Bouter C, Ritter CO, Ströbel P, Lotz J, et al. Biphasic 68Ga-PSMA-HBED-CC-PET/CT in patients with recurrent and high-risk prostate carcinoma. Eur J Nucl Med Mol Imaging. 2016;43:898–905.
Wondergem M, van der Zant F, Knol R, Lazarenko S, Pruim J, de Jong IJ. 18F-DCFPyL PET/CT in the detection of prostate cancer at 60 and 120 minutes; detection rate, image quality, activity kinetics and biodistribution. J Nucl Med. 2017;58(11):1797–1804
Acknowledgements
A large number of people helped to plan, investigate, and analyze the patients in past years. Amongst them are (in alphabetic order): Heidrun Adam, Stephanie Biedenstein, Renate Brück, Elena Dahlke, Larissa Engel, Tanja Gerwert, Prof. Frederik Giesel, Daniela Johna, Dr. Christian Kleist, Dr. Susanne Krämer, Dr. Clemens Kratochwil, Kirsten Kunze, Viktoria Reiswich, Franziska Seybold-Epting, Peter Seybold-Epting, Fabian Spohn, and Natalia Zimmermann.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All patients published in this manuscript signed a written informed consent form for the purpose of anonymized evaluation and publication of their data. All reported investigations were conducted in accordance with the Helsinki Declaration and with our national regulations (German Medicinal Products Act, AMG §13 2b). This evaluation was approved by the ethics committee of the University of Heidelberg (S-321-2012).
Conflicts of interest
All authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Afshar-Oromieh, A., Sattler, L.P., Steiger, K. et al. Tracer uptake in mediastinal and paraaortal thoracic lymph nodes as a potential pitfall in image interpretation of PSMA ligand PET/CT. Eur J Nucl Med Mol Imaging 45, 1179–1187 (2018). https://doi.org/10.1007/s00259-018-3965-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-3965-8