Abstract
Objective
To evaluate the predictive potential of total metabolic tumor volume (MTV) reduction during neoadjuvant chemotherapy (NACT) with 18F–FDG-PET/CT in an advanced FIGO stage III/IV epithelial ovarian cancer (EOC) patient cohort.
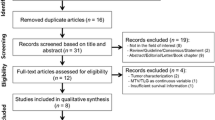
Methods
Twenty-nine primarily inoperable EOC patients underwent 18F–FDG-PET/CT before and after NACT. The pre- and post-NACT total MTV, in addition to the percentage MTV reduction during NACT, were compared with primary therapy outcome and progression-free survival (PFS). ROC-analysis determined an optimal threshold for MTV reduction identifying patients with progressive or stable disease (PD/SD) at the end of primary therapy. A multivariate analysis with residual tumor (0/>0), FIGO stage (III/IV) and MTV reduction compared to PFS was performed. The association between MTV reduction and overall survival (OS) was evaluated.
Results
The median pre- and post-NACT total MTV were 352 cm3 (range 150 to 1322 cm3) and 51 cm3 (range 0 to 417 cm3), respectively. The median MTV reduction during NACT was 89% (range 24% to 100%). Post-NACT MTV and MTV reduction associated with primary therapy outcome (MTV post-NACT p = 0.007, MTV reduction p = 0.001) and PFS (MTV post-NACT p = 0.005, MTV reduction p = 0.005). MTV reduction <85% identified the PD/SD patients (sensitivity 70%, specificity 78%, AUC 0.79). In a multivariate analysis, MTV reduction (p = 0.002) and FIGO stage (p = 0.003) were statistically significant variables associated with PFS. MTV reduction during NACT corresponded to OS (p = 0.05).
Conclusion
18F–FDG-PET/CT is helpful in NACT response evaluation. Patients with total MTV reduction <85% during NACT might be candidates for second-line chemotherapy and clinical trials, instead of interval debulking surgery.




Similar content being viewed by others
References
Benedet JL, Bender H, Jones HI, Ngan HY, Pecorelli S. FIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. Int J Gynecol Obstet. 2000;70:209–62.
Vergote I, Tropé CG, Amant F, Kristensen GB, Ehlen T, Johnson N, et al. Neoadjuvant chemotherapy or primary surgery in stage IIIC or IV ovarian cancer. N Engl J Med. 2010;363:943–53.
du Bois A, Reuss A, Pujade-Lauraine E, Harter P, Ray-Coquard I, Pfisterer J. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: by the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzin. Cancer. 2009;115:1234–44.
Ledermann JA, Raja FA, Fotopoulou C, Colombo N, Sessa C. Clinical practice guidelines newly diagnosed and relapsed epithelial ovarian carcinoma: ESMO clinical practice guidelines clinical practice guidelines. Ann Oncol. 2013;24:24–32.
Wright AA, Bohlke K, Armstrong DK, Bookman MA, Cliby WA, Coleman RL, et al. Neoadjuvant chemotherapy for newly diagnosed, advanced ovarian Cancer: Society of Gynecologic Oncology and American Society of clinical oncology clinical practice guideline. J Clin Oncol. 2016;143:3–15.
Petrillo M, Vizzielli G, Fanfani F, Gallotta V, Cosentino F, Chiantera V, et al. Definition of a dynamic laparoscopic model for the prediction of incomplete cytoreduction in advanced epithelial ovarian cancer: proof of a concept. Gynecol Oncol. 2015;139:5–9.
Vergote I, Amant F, Leunen K, du Bois A, Heitz F, Harter P. Neoadjuvant chemotherapy in advanced ovarian cancer: on what do we agree and disagree ? Gynecol Oncol. 2013;128:6–11.
Axtell AE, Lee MH, Bristow RE, Dowdy SC, Cliby WA, Raman S, et al. Multi-institutional reciprocal validation study of computed tomography predictors of suboptimal primary cytoreduction in patients with advanced ovarian cancer. J Clin Oncol. 2007;25:384–9.
Menczer J, Usviatzov I, Ben-Shem E, Golan A, Levy T. Neoadjuvant chemotherapy in ovarian, primary peritoneal and tubal carcinoma: can imaging results prior to interval debulking predict survival? J Gynecol Oncol. 2011;22:183–7.
Juweid ME, Cheson BD. Positron-emission tomography and assessment of cancer therapy. N Engl J Med. 2006;354:496–507.
Vallius T, Peter A, Auranen A, Carpén O, Kemppainen J, Matomäki J, et al. (18)F-FDG-PET/CT can identify histopathological non-responders to platinum-based neoadjuvant chemotherapy in advanced epithelial ovarian cancer. Gynecol Oncol. 2016;140:29–35.
McPherson A, Roth A, Laks E, Masud T, Bashashati A, Zhang AW, et al. Divergent modes of clonal spread and intraperitoneal mixing in high-grade serous ovarian cancer. Nat Genet. 2016;48:758–67.
Lee JW, Cho A, Lee J-H, Yun M, Lee JD, Kim YT, et al. The role of metabolic tumor volume and total lesion glycolysis on 18F-FDG PET/CT in the prognosis of epithelial ovarian cancer. Eur J Nucl Med Mol Imaging. 2014;41:1898–906.
Chung HH, Kwon HW, Kang KW, Park N-H, Song Y-S, Chung J-K, et al. Prognostic value of preoperative metabolic tumor volume and total lesion glycolysis in patients with epithelial ovarian cancer. Ann Surg Oncol. 2012;19:1966–72.
Vallius T, Hynninen J, Auranen A, Carpén O, Matomäki J, Oksa S, et al. Serum HE4 and CA125 as predictors of response and outcome during neoadjuvant chemotherapy of advanced high-grade serous ovarian cancer. Tumour Biol. 2014;35:12389–95.
Fagotti A, Ferrandina G, Fanfani F, Garganese G, Vizzielli G, Carone V, et al. Prospective validation of a laparoscopic predictive model for optimal cytoreduction in advanced ovarian carcinoma. Am J Obstet Gynecol. 2008;199:642.e1–6.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Rustin GJS, Vergote I, Eisenhauer EA, Pujade-Lauraine E, Quinn M, Thigpen T, et al. Definitions for response and progression in ovarian cancer clinical trials incorporating RECIST 1.1 and CA 125 agreed by the gynecological cancer intergroup (GCIG). Int J Gynecol Cancer. 2011;21:419–23.
Wahl RL, Jacene H, Kasamon Y, Lodge MA. From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med. 2009;50(Suppl 1):122S–50S.
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. ISBN 3–900051–07-0, http://www.R-project.org/.
Jacquet P, Jelinek JS, Steves MA, Sugarbaker PH. Evaluation of computed tomography in patients with peritoneal carcinomatosis. Cancer. 1993;72:1631–6.
Shankar LK, Van Den Abbeele A, Yap J, Benjamin R, Scheutze S, FitzGerald TJ. Considerations for the use of imaging tools for phase II treatment trials in oncology. Clin Cancer Res. 2009;15:1891–7.
Muraji M, Sudo T, Iwasaki S, Ueno S, Wakahashi S, Yamaguchi S, et al. Histopathology predicts clinical outcome in advanced epithelial ovarian cancer patients treated with neoadjuvant chemotherapy and debulking surgery. Gynecol Oncol. 2013;131:531–4.
Kitajima K, Murakami K, Yamasaki E, Kaji Y, Fukasawa I, Inaba N, et al. Diagnostic accuracy of integrated FDG-PET/contrast-enhanced CT in staging ovarian cancer: comparison with enhanced CT. Eur J Nucl Med Mol Imaging. 2008;35:1912–20.
Shim S-H, Lee SJ, Kim S-O, Kim S-N, Kim D-Y, Lee JJ, et al. Nomogram for predicting incomplete cytoreduction in advanced ovarian cancer patients. Gynecol Oncol. 2015;136:30–6.
Hynninen J, Auranen A, Carpén O, Dean K, Seppänen M, Kemppainen J, et al. FDG PET/CT in staging of advanced epithelial ovarian cancer: frequency of supradiaphragmatic lymph node metastasis challenges the traditional pattern of disease spread. Gynecol Oncol. 2012;126:64–8.
Nam EJ, Yun MJ, Oh YT, Kim JW, Kim JH, Kim S, et al. Diagnosis and staging of primary ovarian cancer: correlation between PET/CT, Doppler US, and CT or MRI. Gynecol Oncol. 2010;116:389–94.
Weber WA, Ziegler SI, Thödtmann R, Hanauske AR, Schwaiger M. Reproducibility of metabolic measurements in malignant tumors using FDG PET. J Nucl Med. 1999;40:1771–7.
Rockall AG, Avril N, Lam R, Iannone R, Mozley PD, Parkinson C, et al. Repeatability of quantitative FDG-PET/CT and contrast-enhanced CT in recurrent ovarian carcinoma: test-retest measurements for tumor FDG uptake, diameter, and volume. Clin Cancer Res. 2014;20:2751–60.
Schmidt S, Meuli RA, Achtari C, Prior JO. Peritoneal carcinomatosis in primary ovarian cancer staging: comparison between MDCT, MRI, and 18F-FDG PET/CT. Clin Nucl Med. 2015;40:371–7.
Senft A, De Bree R, Golding RP, Comans EFI, Van Waesberghe JHTM, Kuik JD, et al. Interobserver variability in chest CT and whole body FDG-PET screening for distant metastases in head and neck cancer patients. Mol Imaging Biol. 2011;13:385–90.
Jacene HA, Leboulleux S, Baba S, Chatzifotiadis D, Goudarzi B, Teytelbaum O, et al. Assessment of interobserver reproducibility in quantitative 18F-FDG PET and CT measurements of tumor response to therapy. J Nucl Med. 2009;50:1760–9.
Avril N, Sassen S, Schmalfeldt B, Naehrig J, Rutke S, Weber WA, et al. Prediction of response to neoadjuvant chemotherapy by sequential F-18-fluorodeoxyglucose positron emission tomography in patients with advanced-stage ovarian cancer. J Clin Oncol. 2005;23:7445–53.
Yamamoto M, Tujikawa T, Fujita Y, Chino Y, Kurokawa T, Kiyono Y, et al. Metabolic tumor burden predicts prognosis of ovarian cancer patients who receive platinum-based adjuvant chemotherapy. Cancer Sci. 2016;107:478–85.
Mikhaeel NG, Smith D, Dunn JT, Phillips M, Møller H, Fields PA, et al. Combination of baseline metabolic tumour volume and early response on PET/CT improves progression-free survival prediction in DLBCL. Eur J Nucl Med Mol Imaging. 2016;43:1209–19.
Roedl JB, Colen RR, Holalkere NS, Fischman AJ, Choi NC, Blake MA. Adenocarcinomas of the esophagus: response to chemoradiotherapy is associated with decrease of metabolic tumor volume as measured on PET-CT. Comparison to histopathologic and clinical response evaluation. Radiother Oncol. 2008;89:278–86.
Nakamura K, Hongo A, Kodama J, Hiramatsu Y. The pretreatment of maximum standardized uptake values (SUVmax) of the primary tumor is predictor for poor prognosis for patients with epithelial ovarian cancer. Acta Med Okayama. 2012;66:53–60.
Acknowledgements
This study was financially supported by the Clinical Research (EVO) fund of the Turku University Hospital and grants from the Turku University Foundation, the Medical Faculty of University of Turku, the Finnish Cultural Foundation and Ida Montini Foundation.
Funding
This study was financially supported by the Clinical Research (EVO) fund of the Turku University Hospital and grants from the Turku University Foundation, the Medical Faculty of University of Turku, the Finnish Cultural Foundation and Ida Montini Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Tuulia Vallius has received research grants from the Clinical Research (EVO) fund of the Turku University Hospital, the Turku University Foundation, the Medical Faculty of University of Turku, the Finnish Cultural Foundation and Ida Montini Foundation. All the other co-authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Vallius, T., Hynninen, J., Kemppainen, J. et al. 18F-FDG-PET/CT based total metabolic tumor volume change during neoadjuvant chemotherapy predicts outcome in advanced epithelial ovarian cancer. Eur J Nucl Med Mol Imaging 45, 1224–1232 (2018). https://doi.org/10.1007/s00259-018-3961-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-3961-z