Abstract
Purpose
Commonly used methods for determining split renal function (SRF) from dynamic scintigraphic data require extrarenal background subtraction and additional correction for intrarenal vascular activity. The use of these additional regions of interest (ROIs) can produce inaccurate results and be challenging, e.g. if the heart is out of the camera field of view. The purpose of this study was to evaluate a new method for determining SRF called the blood pool compensation (BPC) technique, which is simple to implement, does not require extrarenal background correction and intrinsically corrects for intrarenal vascular activity.
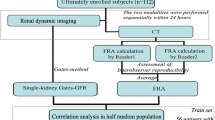
Methods
In the BPC method SRF is derived from a parametric plot of the curves generated by one blood-pool and two renal ROIs. Data from 107 patients who underwent 99mTc-MAG3 scintigraphy were used to determine SRF values. Values calculated using the BPC method were compared to those obtained with the integral (IN) and Patlak-Rutland (PR) techniques using Bland-Altman plotting and Passing-Bablok regression. The interobserver variability of the BPC technique was also assessed for two observers.
Results
The SRF values obtained with the BPC method did not differ significantly from those obtained with the PR method and showed no consistent bias, while SRF values obtained with the IN method showed significant differences with some bias in comparison to those obtained with either the PR or BPC method. No significant interobserver variability was found between two observers calculating SRF using the BPC method.
Conclusion
The BPC method requires only three ROIs to produce reliable estimates of SRF, was simple to implement, and in this study yielded statistically equivalent results to the PR method with appreciable interobserver agreement. As such, it adds a new reliable method for quality control of monitoring relative kidney function.




Similar content being viewed by others
References
Summerlin AL, Lockhart ME, Strang AM, Kolettis PN, Fineberg NS, Smith JK. Determination of split renal function by 3D reconstruction of CT angiograms: a comparison with gamma camera renography. AJR Am J Roentgenol. 2008;191:1552–8.
Lee VS, Rusinek H, Noz ME, Lee PMR, Kramer EL. Dynamic three-dimensional MR renography for the measurement of single kidney function: initial experience. Radiology. 2003;227:289–94.
Prigent A, Cosgriff P, Gates GF, Granerus G, Fine EJ, Itoh K, et al. Consensus report on quality control of quantitative measurements of renal function obtained from the renogram: International Consensus Committee from the Scientific Committee of Radionuclides in Nephrourology. Semin Nucl Med. 1999;29:146–59.
Piepsz A, Tondeur M, Ham H. Relative 99mTc-MAG3 renal uptake: reproducibility and accuracy. J Nucl Med. 1999;40:972–6.
Moonen M, Jacobsson L, Granerus G, Friberg P, Volkmann R. Determination of split renal function from gamma camera renography: a study of three methods. Nucl Med Commun. 1994;15:704–11.
Piepsz A, Dobbeleir A, Ham H. Effect of background correction on separate technetium-99m-DTPA renal clearance. J Nucl Med. 1990;31:430–5.
Rutland MD. A comprehensive analysis of renal DTPA studies. I. Theory and normal values. Nucl Med Commun. 1985;6:11–20.
Piepsz A, Kinthaert J, Tondeur M, Ham HR. The robustness of the Patlak-Rutland slope for determination of split renal function. Nucl Med Commun. 1996;17:817–21.
Patlak CS, Blasberg RG, Fenstermacher JD. Graphical evaluation of blood-to-brain transfer constants from multiple-time uptake data. J Cereb Blood Flow Metab. 1983;3:1–7.
Fleming JS, Kemp PM. A comparison of deconvolution and the Patlak-Rutland plot in renography analysis. J Nucl Med. 1999;40:1503–7.
Šámal M, Piepsz A, Brolin G, Heikkinen JO, Valoušek J. Database of dynamic renal scintigraphy. www.dynamicrenalstudy.org; 2012.
Russell CD, Taylor A, Eshima D. Estimation of technetium-99m-MAG3 plasma clearance in adults from one or two blood samples. J Nucl Med. 1989;30:1955–9.
MATLAB and Statistics Toolbox Release 2013a. Natick, MA: The MathWorks, Inc.; 2013.
Bland JM, Altman DG. Applying the right statistics: analyses of measurement studies. Ultrasound Obstet Gynecol. 2003;22:85–93.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;327:307–10.
Passing H, Bablok W. A new biometrical procedure for testing the equality of measurements from two different analytical methods. J Clin Chem Clin Biochem. 1983;21:709–20.
Bablok W, Passing H. Application of statistical procedures in analytical instrument testing. J Automat Chem. 1985;7(2):74–9.
Tondeur M, Nogarede C, Donoso G, Piepsz A. Inter- and intra-observer reproducibility of quantitative renographic parameters of differential function and renal drainage in children. Scand J Clin Lab Invest. 2013;73:414–21.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was partially supported by the Sylvia Fedoruk Canadian Centre for Nuclear Innovation (grant no. J2012-114), and data collection for the Database of Dynamic Renal Scintigraphy was supported by the Czech Science Foundation (grant no. 303/07/0950).
Conflicts of interest
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the principles of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Prior presentation
A subset of this material was presented in a preliminary form as a poster at the XV ISCORN meeting in Varese, Italy, 15 – 17 October 2013.
Appendix: model of renal activity during the early extraction phase, to illustrate the linear parametric relationship between renal and hepatic activity
Appendix: model of renal activity during the early extraction phase, to illustrate the linear parametric relationship between renal and hepatic activity
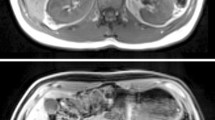
In addition to the kidneys, which excrete MAG3, radionuclide images show nonexcretory blood pooling in blood-rich organs such as the heart, liver and spleen. The aim of background correction is to isolate the count rate that represents MAG3 accumulation in the kidneys from the total count rate in the kidney ROI. Assuming that the time-course of the summed intravascular and interstitial signal (loosely termed ‘blood-pool’ in this paper) is similar in the kidney and in other blood-rich nonexcretory organs such as the heart, liver and spleen, the latter organs can be used as models of the kidneys without excretory function. For example, following injection, the liver count rate peaks (typically during the first minute) and subsequently decreases with time, while the renal counts increase before the peak of the renal curve, which normally occurs at 2.5 – 3.0 min, although this timing can vary between patients. The count rate from the liver ROI acts as a model of the contribution to total kidney count rate from mostly blood pooling, where the blood pool is defined here as intrarenal vascular plus interstitial organ activity during the ascending portion of the renal TAC. The blood pool compensation (BPC) model is then based on similar assumptions to those of the Patlak-Rutland (PR) model, as follows:
Let K(t) represent a renal activity versus time function and H(t) represent a hepatic region activity versus time function. Let us assume, as is assumed for the PR technique, that after the bolus arrives in the kidney, and before urine has emptied from the intrarenal collecting structures at time T, that there is a monoexponential decay in the blood pool within the kidney and that the kidney accumulates extracted activity in proportion to that in the blood pool. That is, we are assuming that the renal blood pool is a scaled renal feed function, f (t), thus
and
where α > 0 is proportional to the extraction fraction and τ is a dummy variable. Substituting Eq. A1 into Eq. A2 yields:
Now, let us assume (ignoring trace hepatocyte extraction of MAG3), that H(t) is some constant, h, multiplied by f (t) over the time interval of interest, then
and
Note that this has the same form as
where \( s=\left(1-\frac{\alpha }{\lambda}\right)\frac{1}{h} \) and \( b=\frac{\alpha c}{\lambda } \). Note that the slope, s, is positive when \( \left(1-\frac{\alpha }{\lambda}\right)>0 \) or negative when \( \left(1-\frac{\alpha }{\lambda}\right)<0 \), while b is strictly positive. Since we can obtain s and b directly from ordinary least squares linear regression of a parametric function of the data, it is not necessary to inspect the plot or know the values of c, α and λ to determine b. The parameter b relates to the extracted count rate in a kidney with the decaying blood pooling removed, which occurs at a time when the parametric liver count rate is zero.
Equation A6 shows that if the blood pool is monoexponentially decreasing during the time interval of fitting, the parametric plot of K(t) and H(t) is linear for t = {t 1,t 2,t 3,…t n }. However, the linearity of the result in Eq. A6 is more general than our selection for an input function.
The renal modelling outlined here is appropriate but of necessity somewhat simplistic. It can be shown that other forms of the renal input functions can yield collinear and/or almost linear relationships between K(t) and H(t) in more complex renal models or states. However, the good agreement of the BPC technique with the best of other methods (PR), while being simpler and making fewer assumptions, provides the best justification for the BPC technique. That is, the BPC model is appropriate in the sense that good models are generally thought to be as simple as possible while still explaining the data. Finally, as the parametric relationship between K(t) and H(t) is collinear during the desired period of observation, quality assurance is possible by testing the linear goodness of fit for the least squares analysis of K(t) and H(t).
Rights and permissions
About this article
Cite this article
Wesolowski, M.J., Conrad, G.R., Šámal, M. et al. A simple method for determining split renal function from dynamic 99mTc-MAG3 scintigraphic data. Eur J Nucl Med Mol Imaging 43, 550–558 (2016). https://doi.org/10.1007/s00259-015-3216-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-015-3216-1