Abstract
Background
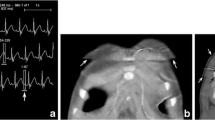
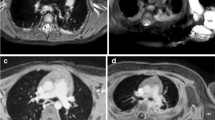
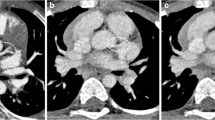
General anesthesia (GA) or sedation has been used to obtain good-quality motion-free breath-hold chest CT scans in young children; however pulmonary atelectasis is a common and problematic accompaniment that can confound diagnostic utility. Dual-source multidetector CT permits ultrafast high-pitch sub-second examinations, minimizing motion artifact and potentially eliminating the need for a breath-hold.
Objective
The purpose of this study was to evaluate the feasibility of free-breathing ultrafast pediatric chest CT without GA and to compare it with breath-hold and non-breath-hold CT with GA.
Materials and methods
Young (≤3 years old) pediatric outpatients scheduled for chest CT under GA were recruited into the study and scanned using one of three protocols: GA with intubation, lung recruitment and breath-hold; GA without breath-hold; and free-breathing CT without anesthesia. In all three protocols an ultrafast high-pitch CT technique was used. We evaluated CT images for overall image quality, presence of atelectasis and motion artifacts.
Results
We included 101 scans in the study. However the GA non-breath-hold technique was discontinued after 15 scans, when it became clear that atelectasis was a major issue despite diligent attempts to mitigate it. This technique was therefore not included in statistical evaluation (86 remaining patients). Overall image quality was higher (P=0.001) and motion artifacts were fewer (P<.001) for scans using the GA with intubation and recruitment technique compared to scans in the non-GA free-breathing group. However no significant differences were observed regarding the presence of atelectasis between these groups.
Conclusion
We demonstrated that although overall image quality was best and motion artifact least with a GA-breath-hold intubation and recruitment technique, free-breathing ultrafast pediatric chest CT without anesthesia provides sufficient image quality for diagnostic purposes and can be successfully performed both without and with contrast agent in young infants.




Similar content being viewed by others
References
Newman B, Krane EJ, Gawande R et al (2014) Chest CT in children: anesthesia and atelectasis. Pediatr Radiol 44:164–172
Sargent MA, McEachern AM, Jamieson DH, Kahwaji R (1999) Atelectasis on pediatric chest CT: comparison of sedation techniques. Pediatr Radiol 29:509–513
Lam WW, Chen PP, So NM, Metreweli C (1998) Sedation versus general anaesthesia in paediatric patients undergoing chest CT. Acta Radiol 39:298–300
Tusman G, Böhm SH, Tempra A et al (2003) Effects of recruitment maneuver on atelectasis in anesthetized children. Anesthesiology 98:14–22
Deak PD, Smal Y, Kalender WA (2010) Multisection CT protocols: sex- and age-specific conversion factors used to determine effective dose from dose-length product. Radiology 257:158–166
Edmark L, Auner U, Enlund M et al (2011) Oxygen concentration and characteristics of progressive atelectasis formation during anaesthesia. Acta Anaesthesiol Scand 55:75–81
Serafini G, Cornara G, Cavalloro F et al (1999) Pulmonary atelectasis during paediatric anaesthesia: CT scan evaluation and effect of positive endexpiratory [sic] pressure (PEEP). Paediatr Anaesth 9:225–228
Cravero JP, Callahan MJ (2017) The radiological home: pediatric anesthesiologist’s role in risk assessment for imaging procedures. Paediatr Anaesth 27:878–879
Tucker E, Jain SK, Mahesh M (2017) Balancing the risks of radiation and anesthesia in pediatric patients. J Am Coll Radiol 14:1459–1461
Pappas JN, Donnelly LF, Frush DP (2000) Reduced frequency of sedation of young children with multisection helical CT. Radiology 215:897–899
Kim SH, Choi YH, Cho HH et al (2016) Comparison of image quality and radiation dose between high-pitch mode and low-pitch mode spiral chest CT in small uncooperative children: the effect of respiratory rate. Eur Radiol 26:1149–1158
Lell MM, May M, Deak P et al (2011) High-pitch spiral computed tomography: effect on image quality and radiation dose in pediatric chest computed tomography. Investig Radiol 46:116–123
Newman B, Ganguly A, Kim JE, Robinson T (2012) Comparison of different methods of calculating CT radiation effective dose in children. AJR Am J Roentgenol 199:W232–W239
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Kino, A., Zucker, E.J., Honkanen, A. et al. Ultrafast pediatric chest computed tomography: comparison of free-breathing vs. breath-hold imaging with and without anesthesia in young children. Pediatr Radiol 49, 301–307 (2019). https://doi.org/10.1007/s00247-018-4295-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-018-4295-5