Abstract
Background
Contrast-enhanced MRI is often used for diagnosis and follow-up of children with inflammatory bowel disease.
Objective
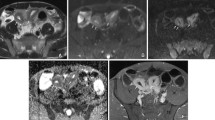
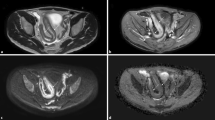
To compare the accuracy of diffusion-weighted MRI (DWI) to contrast-enhanced MRI in children with known or suspected inflammatory bowel disease.
Materials and methods
This retrospective, consecutive study included 55 children. We used ileo-colonoscopy and histology as the reference standard from the terminal ileum to the rectum, and contrast-enhanced MRI as the reference standard proximal to the terminal ileum. DWI and contrast-enhanced MRI sequences were independently reviewed and compared per patient and per segment to these reference standards and to the follow-up for each child.
Results
We obtained endoscopic data for 340/385 colonic and ileal segments (88%). The rate of agreement per segment between DWI and endoscopy was 64%, and the rate of agreement between contrast-enhanced MRI and endoscopy was 59%. Per patient, sensitivity and specificity of bowel wall abnormalities as compared to the endoscopy were 87% and 100% for DWI, and 70% and 100% for contrast-enhanced MRI, respectively. Positive and negative predictive values were, respectively, 100% and 57% for DWI, and 96% and 41% for contrast-enhanced MRI. The sensitivity, specificity, positive predictive value, negative predictive value and accuracy of DWI compare to contrast-enhanced MRI in the segments proximal to the terminal ileum were 90%, 98%, 90%, 98% and 96%, respectively.
Conclusion
The diagnostic performance of DWI is competitive to that of contrast-enhanced MRI in children with known or suspected inflammatory bowel disease.



Similar content being viewed by others
References
Laghi A, Borrelli O, Paolantonio P et al (2003) Contrast-enhanced magnetic resonance imaging of the terminal ileum in children with Crohn’s disease. Gut 52:393–397
Paolantonio P, Ferrari R, Vecchietti F et al (2009) Current status of MR imaging in the evaluation of IBD in a pediatric population of patients. Eur J Radiol 69:418–424
Absah I, Bruining DH, Matsumoto JM et al (2012) MR enterography in pediatric inflammatory bowel disease: retrospective assessment of patient tolerance, image quality, and initial performance estimates. AJR Am J Roentgenol 199:W367–W375
Martin DR, Lauenstein T, Sitaraman SV (2007) Utility of magnetic resonance imaging in small bowel Crohn’s disease. Gastroenterology 133:385–390
Ramalho M, Herédia V, Cardoso C et al (2012) Magnetic resonance imaging of small bowel Crohn’s disease. Acta Medica Port 25:231–240
Maccioni F, Al Ansari N, Mazzamurro F et al (2014) Detection of Crohn disease lesions of the small and large bowel in pediatric patients: diagnostic value of MR enterography versus reference examinations. AJR Am J Roentgenol 203:W533–W542
Makanyanga JC, Taylor SA (2013) Current and future role of MR enterography in the management of Crohn disease. AJR Am J Roentgenol 201:56–64
Mentzel H-J, Reinsch S, Kurzai M, Stenzel M (2014) Magnetic resonance imaging in children and adolescents with chronic inflammatory bowel disease. World J Gastroenterol 20:1180–1191
Dillman JR, Smith EA, Khalatbari S, Strouse PJ (2013) I.V. glucagon use in pediatric MR enterography: effect on image quality, length of examination, and patient tolerance. AJR Am J Roentgenol 201:185–189
Kuo PH, Kanal E, Abu-Alfa AK, Cowper SE (2007) Gadolinium-based MR contrast agents and nephrogenic systemic fibrosis. Radiology 242:647–649
Roberts DR, Holden KR (2016) Progressive increase of T1 signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted MR images in the pediatric brain exposed to multiple doses of gadolinium contrast. Brain Dev 38:331–336
Choi SH, Kim KW, Lee JY et al (2016) Diffusion-weighted magnetic resonance enterography for evaluating bowel inflammation in Crohn’s disease: a systematic review and meta-analysis. Inflamm Bowel Dis 22:669–679
Oussalah A, Laurent V, Bruot O et al (2010) Diffusion-weighted magnetic resonance without bowel preparation for detecting colonic inflammation in inflammatory bowel disease. Gut 59:1056–1065
Seo N, Park SH, Kim K-J et al (2015) MR enterography for the evaluation of small-bowel inflammation in Crohn disease by using diffusion-weighted imaging without intravenous contrast material: a prospective noninferiority study. Radiology 278:762–772
Hordonneau C, Buisson A, Scanzi J et al (2014) Diffusion-weighted magnetic resonance imaging in ileocolonic Crohn’s disease: validation of quantitative index of activity. Am J Gastroenterol 109:89–98
Oto A, Zhu F, Kulkarni K et al (2009) Evaluation of diffusion-weighted MR imaging for detection of bowel inflammation in patients with Crohn’s disease. Acad Radiol 16:597–603
Dubron C, Avni F, Boutry N et al (2016) Prospective evaluation of free-breathing diffusion-weighted imaging for the detection of inflammatory bowel disease with MR enterography in childhood population. Br J Radiol 89:20150840
Neubauer H, Pabst T, Dick A et al (2013) Small-bowel MRI in children and young adults with Crohn disease: retrospective head-to-head comparison of contrast-enhanced and diffusion-weighted MRI. Pediatr Radiol 43:103–114
Sirin S, Kathemann S, Schweiger B et al (2015) Magnetic resonance colonography including diffusion-weighted imaging in children and adolescents with inflammatory bowel disease: do we really need intravenous contrast? Investig Radiol 50:32–39
Shenoy-Bhangle AS, Nimkin K, Aranson T, Gee MS (2016) Value of diffusion-weighted imaging when added to magnetic resonance enterographic evaluation of Crohn disease in children. Pediatr Radiol 46:34–42
Dillman JR, Smith EA, Sanchez R et al (2016) DWI in pediatric small-bowel Crohn disease: are apparent diffusion coefficients surrogates for disease activity in patients receiving infliximab therapy? AJR Am J Roentgenol 207:1002–1008
Oto A, Kayhan A, Williams JTB et al (2011) Active Crohn’s disease in the small bowel: evaluation by diffusion weighted imaging and quantitative dynamic contrast enhanced MR imaging. J Magn Reson Imaging 33:615–624
Kiryu S, Dodanuki K, Takao H et al (2009) Free-breathing diffusion-weighted imaging for the assessment of inflammatory activity in Crohn’s disease. J Magn Reson Imaging 29:880–886
Levine A, Koletzko S, Turner D et al (2014) ESPGHAN revised Porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr 58:795–806
IBD Working Group of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (2005) Inflammatory bowel disease in children and adolescents: recommendations for diagnosis -- the Porto criteria. J Pediatr Gastroenterol Nutr 41:1–7
Lee SS, Kim AY, Yang S-K et al (2009) Crohn disease of the small bowel: comparison of CT enterography, MR enterography, and small-bowel follow-through as diagnostic techniques. Radiology 251:751–761
Gallego JC, Echarri AI, Porta A, Ollero V (2011) Ileal Crohn’s disease: MRI with endoscopic correlation. Eur J Radiol 80:e8–e12
Chalian M, Ozturk A, Oliva-Hemker M et al (2011) MR enterography findings of inflammatory bowel disease in pediatric patients. AJR Am J Roentgenol 196:W810–W816
Leyendecker JR, Bloomfeld RS, DiSantis DJ et al (2009) MR enterography in the management of patients with Crohn disease. Radiographics 29:1827–1846
Hawass NE (1997) Comparing the sensitivities and specificities of two diagnostic procedures performed on the same group of patients. Br J Radiol 70:360–366
van de Schoot R, Kaplan D, Denissen J et al (2014) A gentle introduction to Bayesian analysis: applications to developmental research. Child Dev 85:842–860
Lunn DJ, Thomas A, Best N, Spiegelhalter D (2000) WinBUGS—A Bayesian modelling framework: concepts, structure, and extensibility. Stat Comput 10:325–337
R Development Core Team (2014) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria http://wwwR-projectorg. Accessed 26 Apr 2018
Sturtz S, Ligges U, Gelman AE et al (2005) R2WinBUGS: a package for running WinBUGS from R. J Stat Softw 12:1–16
Taylor SA, Avni F, Cronin CG et al (2017) The first joint ESGAR/ESPR consensus statement on the technical performance of cross-sectional small bowel and colonic imaging. Eur Radiol 27:2570–2582
Grand DJ, Beland MD, Machan JT, Mayo-Smith WW (2012) Detection of Crohn’s disease: comparison of CT and MR enterography without anti-peristaltic agents performed on the same day. Eur J Radiol 81:1735–1741
Park SH, Huh J, Park SH et al (2016) Diffusion-weighted MR enterography for evaluating Crohn’s disease: effect of anti-peristaltic agent on the diagnosis of bowel inflammation. Eur Radiol 27:2554–2562
Dohan A, Taylor S, Hoeffel C et al (2016) Diffusion-weighted MRI in Crohn’s disease: current status and recommendations. J Magn Reson Imaging 44:1381–1396
Sohn B, Kim M-J, Koh H et al (2014) Intestinal lesions in pediatric Crohn disease: comparative detectability among pulse sequences at MR enterography. Pediatr Radiol 44:821–830
Dillman JR, Ladino-Torres MF, Adler J et al (2011) Comparison of MR enterography and histopathology in the evaluation of pediatric Crohn disease. Pediatr Radiol 41:1552–1558
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Khachab, F., Loundou, A., Roman, C. et al. Can diffusion weighting replace gadolinium enhancement in magnetic resonance enterography for inflammatory bowel disease in children?. Pediatr Radiol 48, 1432–1440 (2018). https://doi.org/10.1007/s00247-018-4169-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-018-4169-x