Abstract
Background
Limb-length discrepancy (LLD) in children with congenital lower extremity shortening is constant in proportion from birth to skeletal maturity (known as constant inhibition), but its developmental pattern in utero is unknown. The popular prenatal multiplier method to predict LLD at birth assumes constant inhibition in utero to be true. Verifying the in utero developmental pattern of LLD, and thus confirming the validity of the prenatal multiplier method, is crucial for meaningful prenatal parental counseling.
Objective
To elucidate the in utero developmental pattern of LLD in fetuses with congenital lower extremity shortening.
Materials and methods
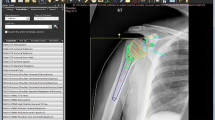
Clinical indications for 3,605 lower extremity radiographs performed on infants (<1 year old) at a large tertiary hospital over a 17-year period were reviewed. Inclusion criteria were (1) diagnosis of congenital lower extremity shortening, (2) bilateral lower limb postnatal radiographs documenting LLD and (3) fetal ultrasound (US) documenting LLD. Available measurements of femoral, tibial and fibular lengths on fetal US and postnatal radiographs were collected. Prenatal and postnatal length ratios of shorter-to-longer bones were calculated and compared.
Results
Eighteen infants met inclusion criteria. Diagnoses were proximal focal femoral deficiency=4, congenital short femur=2, tibial hemimelia=3, posteromedial tibial bowing=6 and fibular hemimelia=3. The correlations between postnatal and prenatal length ratios were high for the femur, tibia and fibula (R>0.98, P<0.0001). The relative differences in the postnatal and prenatal length ratios of these bones were small (|average|<0.026, standard deviation <0.068).
Conclusion
Our data indicate that the postnatal and prenatal length ratios were equivalent, supporting the constant inhibition pattern of LLD in utero, thus validating the prenatal multiplier method for predicting LLD.










Similar content being viewed by others
References
Shapiro F (1982) Developmental patterns in lower-extremity length discrepancies. J Bone Joint Surg Am 64:639–651
Ring PA (1959) Congenital short femur; simple femoral hypoplasia. J Bone Joint Surg Br 41B:73–79
Pappas AM (1984) Congenital posteromedial bowing of the tibia and fibula. J Pediatr Orthop 4:525–531
Westin GW, Sakai DN, Wood WL (1976) Congenital longitudinal deficiency of the fibula. J Bone Joint Surg Am 58:492–496
Achterman C, Kalamchi A (1979) Congenital deficiency of the fibula. J Bone Joint Surg Br 61B:133–137
Paley D, Bhave A, Herzenberg JE et al (2000) Multiplier method for predicting limb-length discrepancy. J Bone Joint Surg Am 82A:1432–1446
Grantz KL, Hediger ML, Liu D et al (2018) Fetal growth standards: the NICHD fetal growth study approach in context with INTERGROWTH-21st and the World Health Organization Multicentre Growth Reference Study. Am J Obstet Gynecol 218:S641–S655.e28
D’Ambrosio V, Pasquali G, Squarcella A et al (2016) Prenatal diagnosis of proximal focal femoral deficiency: literature review of prenatal sonographic findings. J Clin Ultrasound 44:252–259
Radler C, Myers AK, Hunter RJ et al (2014) Prenatal diagnosis of congenital femoral deficiency and fibular hemimelia. Prenat Diagn 34:940–945
Ramirez M, Hecht JT, Taylor S et al (1994) Tibial hemimelia syndrome: prenatal diagnosis by real-time ultrasound. Prenat Diagn 14:167–171
Dreyfus M, Baldauf JJ, Rigaut E et al (1996) Prenatal diagnosis of unilateral tibial hemimelia. Ultrasound Obstet Gynecol 7:205–207
Zollinger PE, Wessels MW, Wladimiroff JW et al (2000) Prenatal ultrasonographic diagnosis of posteromedial bowing of the leg: two case reports. Ultrasound Obstet Gynecol 15:150–153
Paley J, Gelman A, Paley D et al (2005) The prenatal multiplier method for prediction of limb length discrepancy. Prenat Diagn 25:435–438
Rogala EJ, Wynne-Davis R, Littlejohn A et al (1974) Congenital limb anomalies: frequency and aetiological factors. Data from the Edinburgh Register of the Newborn (1964-68). J Med Genet 11:221–233
Brown FW (1971) The Brown operation for total hemimelia tibia. In: Aitken GT (ed) Selected lower-limb anomalies: surgical and prosthetics management. National Academy of Sciences, Washington, DC, pp 20–28
Boakes JL, Stevens PM, Moseley RF (1991) Treatment of genu valgus deformity in congenital absence of the fibula. J Pediatr Orthop 11:721–724
Froster UG, Baird PA (1993) Congenital defects of lower limbs and associated malformations: a population based study. Am J Med Genet 45:60–64
Bronstein M, Deutsch M (1992) Early diagnosis of proximal femoral deficiency. Gynecol Obstet Investig 34:246–248
Boden SD, Fallon MD, Davidson R et al (1989) Proximal femoral focal deficiency: evidence for a defect in proliferation and maturation of chondrocytes. J Bone Joint Surg Am 71:1119–1129
Johnson RL, Tabin CJ (1997) Molecular models for vertebrate limb development. Cell 90:979–990
Zguricas J, Bakker WF, Heus H et al (1998) Genetics of limb development and congenital hand malformations. Plast Reconstr Surg 101:1126–1135
Sifakis S, Basel D, Ianakiev P et al (2001) Distal limb malformations: underlying mechanisms and clinical associations. Clin Genet 60:165–172
Gramellini D, Fieni S, Vadora E (2003) Prenatal diagnosis of isolated limb defects: an updated review. Fetal Diagn Ther 20:96–101
Bryant DD 3rd, Epps CH (1991) Proximal femoral focal deficiency evaluation and management. Orthopedics 14:775–784
Reynolds JF, Wyandt HE, Kelly TE (1985) De novo 21q interstitial deletion in a retarded boy with ulno-fibular dysostosis. Am J Med Genet 20:173–180
Zuniga A, Zeller R, Probst S (2012) The molecular basis of human congenital limb malformations. Wiley Interdiscip Rev Dev Biol 1:803–822
Deimling S, Sotiropoulos C, Lau K et al (2016) Tibial hemimelia associated with GL13 truncation. J Hum Genet 61:443–446
Pauli RM, Feldman PF (1986) Major limb malformations following intrauterine exposure to ethanol: two additional cases and literature review. Teratology 33:273–280
Hoyme HE, Jones KL, Dixon SD et al (1990) Prenatal cocaine exposure and fetal vascular disruption. Pediatrics 85:743–747
McCredie J, Willert HG (1999) Longitudinal limb deficiencies and the slcerotomes. An analysis of 378 dysmelic malformations induced by thalidomide. J Bone Joint Surg (Br) 81:9–23
Froster UG, Baird PA (1993) Maternal factors, medications, and drug exposure in congenital limb reduction defects. Environ Health Perspect 101:269–274
Kelly PM, Dimeglio A (2008) Lower-limb growth: how predictable are predictions. J Child Orthop 2:407–415
Fowler JR, Ilyas AM (2011) The accuracy of digital radiography in orthopaedic applications. Clin Orthop Relat Res 469:1781–1784
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Tsai, A., Laor, T., Estroff, J.A. et al. Constant inhibition in congenital lower extremity shortening: does it begin in utero?. Pediatr Radiol 48, 1451–1462 (2018). https://doi.org/10.1007/s00247-018-4153-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-018-4153-5