Abstract
Background
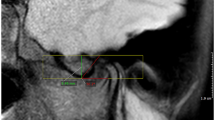
Recognition of normal temporomandibular joints (TMJs) is essential to assess arthropathic changes. Few, if any, prior studies have evaluated the morphological appearance of growing TMJs by magnetic resonance (MR) examinations in the pediatric population.
Objective
This study aimed to determine normative osseous appearance of growing TMJs according to age and gender, both qualitatively and quantitatively, concerning structural and bone marrow changes.
Materials and methods
From 1,036 MR scans screened, one joint was included from each of 157 patients (76% female; 2–18 years) presenting with at least one normal-appearing TMJ was included. Quantitatively, mandibular condyle was characterized by measuring the following: (i) head-neck angle, (ii) anteversion angle, (iii) condylar dimensions (mediolateral, craniocaudal and anteroposterior [AP]) and (iv) condylar volume. Furthermore, qualitative categorization of condylar shape, into one of three types, and condylar bone marrow type was performed.
Results
The head-neck angle significantly correlated with age (bivariable regression β =0.60, P<0.001), indicating an increase of 1.6 degrees per year. Except for AP diameter of condyles, all other mandibular dimensions and condylar volume increased with age (β =0.20–0.59, P≤0.001–0.004). Significant age difference was observed among the different condylar shapes (P<0.001), indicating a change from rounded head without anterior tilt to rectangular head with anterior tilt. Lastly, mandibular condylar size, measured by volume and by AP and mediolateral dimensions, appeared larger in males.
Conclusion
The morphology of the mandibular condyles changes with age. During development, the shape of the condyles changes from round to rectangular in contour with the development of the anterior condylar tilt, as measured by the head-neck angle.





Similar content being viewed by others
References
Ringold S, Cron RQ (2009) The temporomandibular joint in juvenile idiopathic arthritis: frequently used and frequently arthritic. Pediatr Rheumatol Online J 7:11
Billiau AD, Hu Y, Verdonck A et al (2007) Temporomandibular joint arthritis in juvenile idiopathic arthritis: prevalence, clinical and radiological signs, and relation to dentofacial morphology. J Rheumatol 34:1925–1933
Larheim TA, Hoyeraal HM, Stabrun AE et al (1982) The temporomandibular joint in juvenile rheumatoid arthritis. Radiographic changes related to clinical and laboratory parameters in 100 children. Scand J Rheumatol 11:5–12
Koos B, Twilt M, Kyank U et al (2014) Reliability of clinical symptoms in diagnosing temporomandibular joint arthritis in juvenile idiopathic arthritis. J Rheumatol 41:1871–1877
Fjeld MG, Arvidsson LZ, Smith HJ et al (2010) Relationship between disease course in the temporomandibular joints and mandibular growth rotation in patients with juvenile idiopathic arthritis followed from childhood to adulthood. Pediatr Rheumatol Online J 8:13
Larheim TA, Haanaes HR (1981) Micrognathia, temporomandibular joint changes and dental occlusion in juvenile rheumatoid arthritis of adolescents and adults. Scand J Dent Res 89:329–338
Weiss PF, Arabshahi B, Johnson A et al (2008) High prevalence of temporomandibular joint arthritis at disease onset in children with juvenile idiopathic arthritis, as detected by magnetic resonance imaging but not by ultrasound. Arthritis Rheum 58:1189–1196
Colebatch-Bourn AN, Edwards CJ, Collado P et al (2015) EULAR-PReS points to consider for the use of imaging in the diagnosis and management of juvenile idiopathic arthritis in clinical practice. Ann Rheum Dis 74:1946–1957
Roth C, Ward RJ, Tsai S et al (2005) MR imaging of the TMJ: a pictorial essay. Apply Radiol 34:9–16
Larheim TA, Doria AS, Kirkhus E et al (2015) TMJ imaging in JIA patients-an overview. Semin Orthod 21:102–110
Munir S, Patil K, Miller E et al (2014) Juvenile idiopathic arthritis of the axial joints: a systematic review of the diagnostic accuracy and predictive value of conventional MRI. AJR Am J Roentgenol 202:199–210
Krisjane Z, Urtane I, Krumina G et al (2007) Condylar and mandibular morphological criteria in the 2D and 3D MSCT imaging for patients with class II division 1 subdivision malocclusion. Stomatologija 9:67–71
Sinha VP, Pradhan H, Gupta H et al (2012) Efficacy of plain radiographs, CT scan, MRI and ultrasonography in temporomandibular joint disorders. Natl J Maxillofac Surg 3:2–9
Angenete OW, Augdal TA, Jellestad S et al (2018) Normal magnetic resonance appearances of the temporomandibular joints in children and young adults aged 2-18 years. Pediatr Radiol 48:341–349
Vaid YN, Dunnavant FD, Royal SA et al (2014) Imaging of the temporomandibular joint in juvenile idiopathic arthritis. Arthritis Care Res 66:47–54
Kellenberger CJ, Arvidsson LZ, Larheim TA (2015) Magnetic resonance imaging of temporomandibular joints in juvenile idiopathic arthritis. Semin Orthod 21:111–120
Yang ZJ, Song DH, Dong LL et al (2015) Magnetic resonance imaging of temporomandibular joint: morphometric study of asymptomatic volunteers. J Craniofac Surg 26:425–429
Karlo CA, Stolzmann P, Habernig S et al (2010) Size, shape and age-related changes of the mandibular condyle during childhood. Eur Radiol 20:2512–2517
Baek SH, Kim TK, Kim MJ (2006) Is there any difference in the condylar osition and angulation after asymmetric mandibular setback? Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:155–163
Ha MH, Kim YI, Park SB et al (2013) Cone-beam computed tomographic evaluation of the condylar remodeling occurring after mandibular set-back by bilateral sagittal split ramus osteotomy and rigid fixation. Korean J Orthod 43:263–270
Yamada M, Matsuzaka T, Uetani M et al (1995) Normal age-related conversion of bone marrow in the mandible: MR imaging findings. AJR Am J Roentgenol 165:1223–1228
Tecco S, Saccucci M, Nucera R et al (2010) Condylar volume and surface in Caucasian young adult subjects. BMC Med Imaging 10:28
Saccucci M, D’Attilio M, Rodolfino D et al (2012) Condylar volume and condylar area in class I, class II and class III young adult subjects. Head Face Med 8:34
Al-koshab M, Nambiar P, John J (2015) Assessment of condyle and glenoidfossa morphology using CBCT in south-east Asians. PLoS One 10: e0121682
Christiansen EL, Chan TT, Thompson JR et al (1987) Computed tomography of the normal temporomandibular joint. Scand J Dent Res 95:499–509
Christiansen EL, Thompson JR, Zimmerman G et al (1987) Computed tomography of condylar and articular disk positions within the temporomandibular joint. Oral Surg Oral Med Oral Pathol 64:757–767
Meng F, Liu Y, Hu K et al (2008) A comparative study of the skeletal morphology of the temporomandibular joint of children and adults. J Postgrad Med 54:191–194
Ma GMY, Amirabadi A, Inarejos E et al (2015) MRI thresholds for discrimination between normal and mild temporomandibular joint involvement in juvenile idiopathic arthritis. Pediatr Rheumatol Online J 13:53
Kottke R, Saurenmann RK, Schneider MM et al (2015) Contrast-enhanced MRI of the temporomandibular joint: findings in children without juvenile idiopathic arthritis. Acta Radiol 56:1145–1152
Resnick CM, Vakilian PM, Breen M et al (2016) Quantifying temporomandibular joint synovitis in children with juvenile idiopathic arthritis. Arthritis Care Res 68:1795–1802
von Kalle T, Winkler P, Stuber T (2013) Contrast-enhanced MRI of normal temporomandibular joints in children--is there enhancement or not? Rheumatology (Oxford) 52:363–367
von Kalle T, Stuber T, Winkler P et al (2015) Early detection of temporomandibular joint arthritis in children with juvenile idiopathic arthritis - the role of contrast-enhanced MRI. Pediatr Radiol 45:402–410
Acknowledgements
This work was presented at the 60th Annual Meeting and Categorical Course of the Society for Pediatric Radiology in Vancouver, BC, Canada, on May 18, 2017.
We would like to thank Dr. Lynn Spiegel, Rheumatology Department, The Hospital for Sick Children, for providing relevant clinical information.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Electronic supplementary material
ESM 1
(DOC 364 kb)
Rights and permissions
About this article
Cite this article
Junhasavasdikul, T., Abadeh, A., Tolend, M. et al. Developing a reference MRI database for temporomandibular joints in healthy children and adolescents. Pediatr Radiol 48, 1113–1122 (2018). https://doi.org/10.1007/s00247-018-4142-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-018-4142-8