Abstract
Background
Knowledge of normal appearances of the temporomandibular joint (TMJ) is paramount when assessing the joint for disease in juvenile idiopathic arthritis. Reliable features defining normal TMJs in children are limited.
Objective
To establish reliable normal standards for the TMJ at magnetic resonance imaging (MRI).
Materials and methods
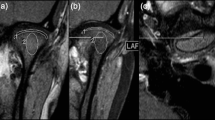
We included children and young adults aged 2–18 years undergoing a head MRI for reasons not believed to affect the TMJs. We assessed TMJ anatomy and contrast enhancement using a high-resolution 3-D T1-weighted sequence. We noted joint fluid and bone marrow oedema based on a T2-weighted sequence. Three experienced radiologists read all examinations twice in consensus and defined intraobserver consensus agreement.
Results
We evaluated the TMJs in 101 children and young adults (45 female), mean age 10.7 years (range 2–18 years). The intraobserver consensus agreement for the assessment of anterior condylar inclination in the sagittal/oblique plane was moderate to good (Cohen κ=0.7 for the right side). Cohen κ for intraobserver consensus agreement for condylar shape in the coronal plane on a 0–2 scale was 0.4 for the right and 0.6 for the left. Intraobserver agreement for measurement of joint space height and assessment of bone marrow oedema was poor. There was a statistically significant increase in anterior inclination by age in the sagittal plane on a 0–2 scale (P<0.0001). Eighty percent of the condyles showed a rounded shape in the coronal plane while 20% showed mild flattening. Thirty-five of 36 right TMJs showed contrast enhancement (mild enhancement in 32 joints, moderate in 3 joints).
Conclusion
Subjective assessment of the anterior condylar inclination in the sagittal/oblique plane and condylar flattening in the coronal plane can be considered precise features for describing TMJ anatomy in healthy children. There is an increasing anterior inclination by age. Mild contrast enhancement of the TMJs should be considered a normal finding.








Similar content being viewed by others

References
Stoll ML, Sharpe T, Beukelman T et al (2012) Risk factors for temporomandibular joint arthritis in children with juvenile idiopathic arthritis. J Rheumatol 39:1880–1887
Cannizzaro E, Schroeder S, Muller LM et al (2011) Temporomandibular joint involvement in children with juvenile idiopathic arthritis. J Rheumatol 38:510–515
Ringold S, Cron RQ (2009) The temporomandibular joint in juvenile idiopathic arthritis: frequently used and frequently arthritic. Pediatr Rheumatol Online J 7:11
Abramowicz S, Cheon JE, Kim S et al (2011) Magnetic resonance imaging of temporomandibular joints in children with arthritis. J Oral Maxillofac Surg 69:2321–2328
Arvidsson LZ, Smith HJ, Flato B et al (2010) Temporomandibular joint findings in adults with long-standing juvenile idiopathic arthritis: CT and MR imaging assessment. Radiology 256:191–200
Twilt M, Mobers SM, Arends LR et al (2004) Temporomandibular involvement in juvenile idiopathic arthritis. J Rheumatol 31:1418–1422
Weiss PF, Arabshahi B, Johnson A et al (2008) High prevalence of temporomandibular joint arthritis at disease onset in children with juvenile idiopathic arthritis, as detected by magnetic resonance imaging but not by ultrasound. Arthritis Rheum 58:1189–1196
Kuseler A, Pedersen TK, Gelineck J et al (2005) A 2 year followup study of enhanced magnetic resonance imaging and clinical examination of the temporomandibular joint in children with juvenile idiopathic arthritis. J Rheumatol 32:162–169
Moe JS, Desai NK, Aiken AH et al (2016) Magnetic resonance imaging of temporomandibular joints of children. J Oral Maxillofac Surg 74:1723–1727
Arabshahi B, Cron RQ (2006) Temporomandibular joint arthritis in juvenile idiopathic arthritis: the forgotten joint. Curr Opin Rheumatol 18:490–495
Muller L, Kellenberger CJ, Cannizzaro E et al (2009) Early diagnosis of temporomandibular joint involvement in juvenile idiopathic arthritis: a pilot study comparing clinical examination and ultrasound to magnetic resonance imaging. Rheumatology 48:680–685
Kuseler A, Pedersen TK, Herlin T et al (1998) Contrast enhanced magnetic resonance imaging as a method to diagnose early inflammatory changes in the temporomandibular joint in children with juvenile chronic arthritis. J Rheumatol 25:1406–1412
Karlo CA, Stolzmann P, Habernig S et al (2010) Size, shape and age-related changes of the mandibular condyle during childhood. Eur Radiol 20:2512–2517
Kottke R, Saurenmann RK, Schneider MM et al (2014) Contrast-enhanced MRI of the temporomandibular joint: findings in children without juvenile idiopathic arthritis. Acta Radiol 56:1145–1152
Meng F, Liu Y, Hu K et al (2008) A comparative study of the skeletal morphology of the temporo-mandibular joint of children and adults. J Postgrad Med 54:191–194
Katsavrias EG (2002) Changes in articular eminence inclination during the craniofacial growth period. Angle Orthod 72:258–264
Tzaribachev N, Fritz J, Horger M (2009) Spectrum of magnetic resonance imaging appearances of juvenile temporomandibular joints (TMJ) in non-rheumatic children. Acta Radiol 50:1182–1186
Christiansen EL, Chan TT, Thompson JR et al (1987) Computed tomography of the normal temporomandibular joint. Scand J Dent Res 95:499–509
Kinniburgh RD, Major PW, Nebbe B et al (2000) Osseous morphology and spatial relationships of the temporomandibular joint: comparisons of normal and anterior disc positions. Angle Orthod 70:70–80
Kottke RST, Grotzer M, Kellenberger C (2008) MRI of paediatric temporomandibular joints, normal findings. Pediatr Radiol 38:S534–S569
von Kalle T, Winkler P, Stuber T (2013) Contrast-enhanced MRI of normal temporomandibular joints in children — is there enhancement or not? Rheumatology 52:363–367
Ma GM, Amirabadi A, Inarejos E et al (2015) MRI thresholds for discrimination between normal and mild temporomandibular joint involvement in juvenile idiopathic arthritis. Pediatr Rheumatol Online J 13:53
Resnick CM, Vakilian PM, Breen M et al (2016) Quantifying temporomandibular joint synovitis in children with juvenile idiopathic arthritis. Arthritis Care Res 68:1795–1802
Arvidsson LZ, Flato B, Larheim TA (2009) Radiographic TMJ abnormalities in patients with juvenile idiopathic arthritis followed for 27 years. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108:114–123
Cohen J (1960) Weighted kappa: nominal scale agreement provision for scaled agreement or partial credit. Psychol Bull 70:213–220
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Engesaeter IO, Laborie LB, Lehmann TG et al (2012) Radiological findings for hip dysplasia at skeletal maturity. Validation of digital and manual measurement techniques. Skelet Radiol 41:775–785
Acknowledgements
Parts of this study were funded by the Liaison Committee between the Central Norway Regional Health Authority (RHA) and the Norwegian University of Science and Technology (NTNU).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Angenete, O.W., Augdal, T.A., Jellestad, S. et al. Normal magnetic resonance appearances of the temporomandibular joints in children and young adults aged 2–18 years. Pediatr Radiol 48, 341–349 (2018). https://doi.org/10.1007/s00247-017-4048-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-017-4048-x