Abstract
Background
Pediatric head trauma, including abusive head trauma, is a significant cause of morbidity and mortality.
Objective
The purpose of this research was to identify and evaluate radiologic interpretation errors of head CTs performed on abusive and non-abusive pediatric head trauma patients from a community setting referred for a secondary interpretation at a tertiary pediatric hospital.
Materials and methods
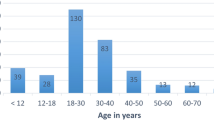
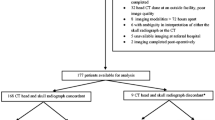
A retrospective search identified 184 patients <5 years of age with head CT for known or potential head trauma who had a primary interpretation performed at a referring community hospital by a board-certified radiologist. Two board-certified fellowship-trained neuroradiologists at an academic pediatric hospital independently interpreted the head CTs, compared their interpretations to determine inter-reader discrepancy rates, and resolved discrepancies to establish a consensus second interpretation. The primary interpretation was compared to the consensus second interpretation using the RADPEER™ scoring system to determine the primary interpretation-second interpretation overall and major discrepancy rates. MRI and/or surgical findings were used to validate the primary interpretation or second interpretation when possible. The diagnosis of abusive head trauma was made using clinical and imaging data by a child abuse specialist to separate patients into abusive head trauma and non-abusive head trauma groups. Discrepancy rates were compared for both groups. Lastly, primary interpretations and second interpretations were evaluated for discussion of imaging findings concerning for abusive head trauma.
Results
There were statistically significant differences between primary interpretation-second interpretation versus inter-reader overall and major discrepancy rates (28% vs. 6%, P=0.0001; 16% vs. 1%, P=0.0001). There were significant differences in the primary interpretation-second interpretation overall and major discrepancy rates for abusive head trauma patients compared to non-abusive head trauma patients (41% vs 23%, P=0.02; 26% vs. 12%, P=0.03). The most common findings resulting in major radiologic interpretation errors were fractures and subdural hemorrhage. Differences in the age of the patient and the percentage of patients with hemorrhage were statistically significant between the abusive head trauma versus non-abusive head trauma groups, while no statistical difference was identified for skull fractures, ischemia, head CT radiation dose, or presence of multiplanar or 3-D reformatted images. The second interpretation more frequently indicated potential for abusive head trauma compared to the primary interpretation (P=0.0001). MRI and/or surgical findings were in agreement with the second interpretation in 29/29 (100%) of patients with discrepancies.
Conclusion
A high incidence of radiologic interpretation errors may occur in pediatric trauma patients at risk for abusive head trauma who are referred from a community hospital. This suggests value for second interpretations of head CTs at a tertiary pediatric hospital for this patient population.



Similar content being viewed by others
References
Parks SE, Annest JL, Hill HA et al (2012) Pediatric abusive head trauma: recommended definitions for public health surveillance and research. Centers for Disease Control and Prevention, Atlanta
Niederkrotenthaler T, Xu L, Parks SE et al (2013) Descriptive factors of abusive head trauma in young children—United States, 2000–2009. Child Abuse Negl 37:446–455
Duhaime AC, Christian C, Moss E et al (1996) Long-term outcome in infants with the shaking-impact syndrome. Pediatr Neurosurg 24:292–298
Chevignard MP, Lind K (2014) Long-term outcome of abusive head trauma. Pediatr Radiol 44:S548–S558
Reece RM, Sege R (2000) Childhood head injuries: accidental or inflicted? Arch Pediatr Adolesc Med 154:11–15
Sills MR, Libby AM, Orton HD (2005) Prehospital and in-hospital mortality: a comparison of intentional and unintentional traumatic brain injuries in Colorado children. Arch Pediatr Adolesc Med 159:665–670
Jenny C, Hymel KP, Ritzen A et al (1999) Analysis of missed cases of abusive head trauma. JAMA 281:621–626
Jaspan T, Griffiths PD, McConachie NS et al (2003) Neuroimaging for non-accidental head injury in childhood: a proposed protocol. Clin Radiol 58:44–53
Ginde AA, Foianini A, Renner DM et al (2008) Availability and quality of computed tomography and magnetic resonance imaging equipment in U.S. emergency departments. Acad Emerg Med 15:780–783
Eakins C, Ellis WD, Pruthi S et al (2012) Second opinion interpretations by specialty radiologists at a pediatric hospital: rate of disagreement and clinical implications. AJR Am J Roentgenol 199:916–920
Loevner LA, Sonners AI, Schulman BJ et al (2002) Reinter-pretation of cross-sectional images in patients with head and neck cancer in the setting of a multidisciplinary cancer center. AJNR Am J Neuroradiol 23:1622–1626
Jordan MJ, Lightfoot JB, Jordan JE (2006) Quality outcomes of reinterpretation of brain CT imaging studies by subspecialty experts in neuroradiology. J Natl Med Assoc 98:1326–1328
Zan E, Yousem DM, Carone M et al (2010) Second opinion consultation in neuroradiology. Neuroradiology 255:135–141
Briggs GM, Flynn PA, Worthington M et al (2008) The role of specialist neuroradiology second opinion reporting: is there added value? Clin Radiol 63:791–795
Jackson VP, Cushing T, Abujudeh HH et al (2009) RADPEER scoring white paper. J Am Coll Radiol 6:21–25
Kemp AM, Jaspan T, Griffiths J et al (2011) Neuroimaging: what neuroradiological features distinguish abusive from non-abusive head trauma? A systematic review. Arch Dis Child 96:1103–1112
Piteau SJ, Ward MGK, Barrowman NJ et al (2012) Clinical and radiographic characteristics associated with abusive and nonabusive head trauma: a systemic review. Pediatrics 130:315–323
Leventhal JM, Thomas SA, Rosenfield NS et al (1993) Fractures in young children: distinguishing child abuse from unintentional injuries. Am J Dis Child 147:87–92
Thomas SA, Rosenfield NS, Leventhal JM et al (1991) Long-bone fractures in young children: distinguishing accidental injuries from child abuse. Pediatrics 88:471–476
Borgstede JP, Lewis RS, Bhargavan M et al (2004) RADPEER quality assurance program: a multifacility study of interpretive disagreement rates. J Am Coll Radiol 1:59–65
Siegle RL, Baram EM, Reuter SR et al (1998) Rates of disagreement in imaging interpretation in a group of community hospitals. Acad Radiol 5:148–154
Robinson PJ, Wilson D, Coral A et al (1999) Variation between experienced observers in the interpretation of accident and emergency radiographs. Br J Radiol 72:323–330
Soffa DJ, Lewis RS, Sunshine JH et al (2004) Disagreement in interpretation: a method for the development of benchmarks for quality assurance in imaging. J Am Coll Radiol 1:212–217
Berlin L (2007) Radiologic errors and malpractice: a blurry distinction. AJR Am J Roentgenol 189:517–522
Babiarz LS, Yousem DM (2012) Quality control in neuroradiology: discrepancies in image interpretation among academic neuroradiologists. AJNR Am J Neuroradiol 33:37–42
Orman G, Wagner MW, Seeburg D et al (2015) Pediatric skull fracture diagnosis: should 3D CT reconstructions be added as routine imaging? J Neurosurg Pediatr 16:426–431
Langford S, Panigrahy A, Narayanan S et al (2015) Multiplanar reconstructed CT images increased depiction of intracranial hemorrhages in pediatric head trauma. Neuroradiology 57:1263–1268
Hymel KP, Willson DF, Boos SC et al (2014) Derivation of a clinical prediction rule for pediatric abusive head trauma. Pediatrics 134:e1537–e1544
Hymel KP, Herman BE, Narang SK et al (2015) Potential impact of a validated screening tool for pediatric abusive head trauma. J Pediatr 167:1375–1381
Brown JL (2013) Responsibilities and risks when radiologists evaluate patients for child abuse. AJR Am J Roentgenol 200:948–949
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. R. A. Hibbard and Dr. R. A. Hicks testify in child abuse cases. Drs. Kralik, Finke, Wu and Ho report no conflicts of interest.
Rights and permissions
About this article
Cite this article
Kralik, S.F., Finke, W., Wu, I.C. et al. Radiologic head CT interpretation errors in pediatric abusive and non-abusive head trauma patients. Pediatr Radiol 47, 942–951 (2017). https://doi.org/10.1007/s00247-017-3872-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-017-3872-3