Abstract
Background
Dipyridamole and adenosine are traditional pharmacological stressors for myocardial perfusion. Regadenoson, a selective adenosine A2A agonist, has a lower side effect profile with lower incidence of bronchospasm and bradycardia. There is a growing need for myocardial perfusion assessment within pediatrics. There is no report on the utility of regadenoson as a stress agent in children.
Objective
To observe the safety and feasibility of regadenoson as a pharmacologic stressor for perfusion cardiac MR in a pilot cohort of pediatric patients weighing more than 40 kg who have congenital heart disease and pediatric acquired heart disease.
Materials and methods
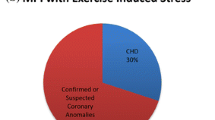
We reviewed our initial experience with regadenoson stress cardiac MR in 31 pediatric patients 15.8 ± 1.7 years (range 12–22 years) with congenital heart disease and acquired heart disease. Mean patient weight was 60 ± 15 kg (range of 40–93 kg). All patients underwent cardiac MR because of concern for ischemia. The cohort included a heterogeneous group of patients at a pediatric institution with potential risk for ischemia. Subjects’ heart rate and blood pressure were monitored and pharmacologic stress was induced by injection of 400 mcg of regadenoson. We evaluated their hemodynamic response and adverse effects using changes in vital signs and onset of symptoms. A pediatric cardiologist and radiologist qualitatively assessed myocardial perfusion and viability images.
Results
One child was unable to complete the stress perfusion portion of the examination, but did complete the remaining portion of the CMR. Resting heart rate was 72 ± 14 beats per minute (bpm) and rose to peak of 124 ± 17 bpm (95 ± 50% increase, P < 0.005) with regadenoson. Image quality was considered good or diagnostic in all cases. Three patients had irreversible perfusion defects. Four patients had reversible perfusion defects. Nine of the patients underwent cardiac catheterization with angiography and the findings showed excellent agreement.
Conclusion
Regadenoson might be a safe and feasible pharmacologic stress agent for use in cardiac MR in older pediatric patients with congenital heart disease and acquired heart disease. The ease of use as a bolus and the advantage of a prolonged hyperemia make its use appealing in pediatrics. In a limited number of cases, regadenoson stress perfusion showed excellent agreement with cardiac catheterization. Regadenoson might be a viable pharmacologic stress agent in this population.



Similar content being viewed by others
References
Hauser M, Bengel FM, Kuhn A et al (2001) Myocardial blood flow and flow reserve after coronary reimplantation in patients after arterial switch and Ross operation. Circulation 103:1875–1880
Vogel M, Smallhorn JF, Gilday D et al (1991) Assessment of myocardial perfusion in patients after the arterial switch operation. J Nucl Med 32:237–241
Secinaro A, Ntsinjana H, Tann O et al (2011) Cardiovascular magnetic resonance findings in repaired anomalous left coronary artery to pulmonary artery connection (ALCAPA). J Cardiovasc Magn Reson 13:27
Mavrogeni S, Papadopoulos G, Douskou M et al (2004) Magnetic resonance angiography is equivalent to X-ray coronary angiography for the evaluation of coronary arteries in Kawasaki disease. J Am Coll Cardiol 43:649–652
Bonnet D, Bonhoeffer P, Piechaud JF et al (1996) Long-term fate of the coronary arteries after the arterial switch operation in newborns with transposition of the great arteries. Heart 76:274–279
Hernandez-Pampaloni M, Allada V, Fishbein MC et al (2003) Myocardial perfusion and viability by positron emission tomography in infants and children with coronary abnormalities: correlation with echocardiography, coronary angiography, and histopathology. J Am Coll Cardiol 41:618–626
Tobler D, Motwani M, Wald RM et al (2014) Evaluation of a comprehensive cardiovascular magnetic resonance protocol in young adults late after the arterial switch operation for D-transposition of the great arteries. J Cardiovasc Magn Reson 16:98
Schwitter J, Wacker CM, Wilke N et al (2013) MR-IMPACT II: magnetic resonance imaging for myocardial perfusion assessment in coronary artery disease trial: perfusion-cardiac magnetic resonance vs. single-photon emission computed tomography for the detection of coronary artery disease: a comparative multicentre, multivendor trial. Eur Heart J 34:775–781
Greenwood JP, Maredia N, Younger JF et al (2012) Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease (CE-MARC): a prospective trial. Lancet 379:453–460
Prakash A, Powell AJ, Krishnamurthy R et al (2004) Magnetic resonance imaging evaluation of myocardial perfusion and viability in congenital and acquired pediatric heart disease. Am J Cardiol 93:657–661
Buechel ER, Balmer C, Bauersfeld U et al (2009) Feasibility of perfusion cardiovascular magnetic resonance in paediatric patients. J Cardiovasc Magn Reson 11:51
Tacke CE, Kuipers IM, Groenink M et al (2011) Cardiac magnetic resonance imaging for noninvasive assessment of cardiovascular disease during the follow-up of patients with Kawasaki disease. Circ Cardiovasc Imaging 4:712–720
Shryock JC, Belardinelli L (1997) Adenosine and adenosine receptors in the cardiovascular system: biochemistry, physiology, and pharmacology. Am J Cardiol 79:2–10
Al Jaroudi W, Iskandrian AE (2009) Regadenoson: a new myocardial stress agent. J Am Coll Cardiol 54:1123–1130
Nguyen KL, Bandettini WP, Shanbhag S et al (2014) Safety and tolerability of regadenoson CMR. Eur Heart J Cardiovasc Imaging 15:753–760
Vasu S, Bandettini WP, Hsu LY et al (2013) Regadenoson and adenosine are equivalent vasodilators and are superior than dipyridamole — a study of first pass quantitative perfusion cardiovascular magnetic resonance. J Cardiovasc Magn Reson 15:85
Pijls NH, van Nunen LX (2015) Fractional flow reserve, maximum hyperemia, adenosine, and regadenoson. Cardiovasc Revasc Med 16:263–265
Gerber BL, Raman SV, Nayak K et al (2008) Myocardial first-pass perfusion cardiovascular magnetic resonance: history, theory, and current state of the art. J Cardiovasc Magn Reson 10:18
Strigl S, Beroukhim R, Valente AM et al (2009) Feasibility of dobutamine stress cardiovascular magnetic resonance imaging in children. J Magn Reson Imaging 29:313–319
Macwar RR, Williams BA, Shirani J (2013) Prognostic value of adenosine cardiac magnetic resonance imaging in patients presenting with chest pain. Am J Cardiol 112:46–50
Gargiulo P, Dellegrottaglie S, Bruzzese D et al (2013) The prognostic value of normal stress cardiac magnetic resonance in patients with known or suspected coronary artery disease: a meta-analysis. Circ Cardiovasc Imaging 6:574–582
Salgado Garcia C, Jimenez Heffernan A, Sanchez de Mora E et al (2014) Comparative study of the safety of regadenoson between patients with mild/moderate chronic obstructive pulmonary disease and asthma. Eur J Nucl Med Mol Imaging 41:119–125
Cerqueira MD, Nguyen P, Staehr P et al (2008) Effects of age, gender, obesity, and diabetes on the efficacy and safety of the selective A2A agonist regadenoson versus adenosine in myocardial perfusion imaging integrated ADVANCE-MPI trial results. JACC Cardiovasc Imaging 1:307–316
Gordi T, Frohna P, Sun HL et al (2006) A population pharmacokinetic/pharmacodynamic analysis of regadenoson, an adenosine A2A-receptor agonist, in healthy male volunteers. Clin Pharmacokinet 45:1201–1212
Hojjati MR, Muthupillai R, Wilson JM et al (2014) Assessment of perfusion and wall-motion abnormalities and transient ischemic dilation in regadenoson stress cardiac magnetic resonance perfusion imaging. Int J Cardiovasc Imaging 30:949–957
Rangel TB, Assreuy AM, Pires Ade F et al (2011) Crystallization and characterization of an inflammatory lectin purified from the seeds of Dioclea wilsonii. Molecules 16:5087–5103
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Noel, C.V., Krishnamurthy, R., Moffett, B. et al. Myocardial stress perfusion magnetic resonance: initial experience in a pediatric and young adult population using regadenoson. Pediatr Radiol 47, 280–289 (2017). https://doi.org/10.1007/s00247-016-3762-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-016-3762-0