Abstract
Magnetic resonance enterography (MRE) now plays a central role in diagnosing pediatric inflammatory bowel disease (IBD), and its role in other intestinal pathologies such as scleroderma is gradually expanding. MRE helps distinguish between Crohn disease and ulcerative colitis, defining extent and severity. Standard MRE protocols can be optimized in children and adolescents to be diagnostic and well tolerated, both of which are important with increasing use of serial MRE in pediatric IBD for monitoring treatment response and evaluating complications. MRI is especially suited to this role given its lack of ionizing radiation. MRE compliance can be improved through patient education. Differing from adult MRE, pediatric MRE protocols use weight-based formulas to calculate oral and intravenous contrast media and antispasmodic agent doses, using either hyoscine-N-butylbromide or glucagon. Nausea is more commonly experienced with glucagon; however vomiting occurs in <10% of children with either agent. Standard and advanced sequences applied in adults are also used in children and adolescents. These include static and cinematic balanced steady-state free precession sequences, single-shot T2-weighted sequences, diffusion-weighted imaging and pre- and post-contrast 3-D T1-weighted gradient echo sequences. Magnetization transfer imaging and quantitative assessment of bowel to distinguish inflammation and fibrosis are not yet standard in pediatric MRE, but show promise.











Similar content being viewed by others
References
Stehling MK, Evans DF, Lamont G et al (1989) Gastrointestinal tract: dynamic MR studies with echo-planar imaging. Radiology 171:41–46
Semelka RC, Shoenut JP, Silverman R et al (1991) Bowel disease: prospective comparison of CT and 1.5-T pre- and postcontrast MR imaging with T1-weighted fat-suppressed and breath-hold FLASH sequences. J Magn Reson Imaging 1:625–632
Hahn PF, Saini S, Cohen MS et al (1992) An aqueous gastrointestinal contrast agent for use in echo-planar MR imaging. Magn Reson Med 25:380–383
Levine A, Koletzko S, Turner D et al (2014) ESPGHAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr 58:795–806
Low RN, Francis IR (1997) MR imaging of the gastrointestinal tract with i.v., gadolinium and diluted barium oral contrast media compared with unenhanced MR imaging and CT. AJR Am J Roentgenol 169:1051–1059
Rimola J, Planell N, Rodríguez S et al (2015) Characterization of inflammation and fibrosis in Crohn’s disease lesions by magnetic resonance imaging. Am J Gastroenterol 110:432–440
Menys A, Atkinson D, Odille F et al (2012) Quantified terminal ileal motility during MR enterography as a potential biomarker of Crohn’s disease activity: a preliminary study. Eur Radiol 22:2494–2501
Tielbeek JA, Ziech ML, Li Z et al (2014) Evaluation of conventional, dynamic contrast enhanced and diffusion weighted MRI for quantitative Crohn’s disease assessment with histopathology of surgical specimens. Eur Radiol 24:619–629
Kovanlikaya A, Beneck D, Rose M et al (2015) Quantitative apparent diffusion coefficient (ADC) values as an imaging biomarker for fibrosis in pediatric Crohn’s disease: preliminary experience. Abdom Imaging 40:1068–1074
Pazahr S, Blume I, Frei P et al (2013) Magnetization transfer for the assessment of bowel fibrosis in patients with Crohn’s disease: initial experience. Magn Reson Mater Phys 26:291–301
Dillman JR, Swanson SD, Johnson LA et al (2015) Comparison of noncontrast MRI magnetization transfer and T2-weighted signal intensity ratios for detection of bowel wall fibrosis in a Crohn’s disease animal model. J Magn Reson Imaging 42:801–810
Mathews JD, Forsythe AV, Brady Z et al (2013) Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ 346:f2360
de Bie CI, Buderus S, Sandhu BK et al (2012) Diagnostic workup of paediatric patients with inflammatory bowel disease in Europe: results of a 5-year audit of the EUROKIDS registry. J Pediatr Gastroenterol Nutr 54:374–380
Horsthuis K, Bipat S, Bennink RJ et al (2008) Inflammatory bowel disease diagnosed with US, MR, scintigraphy, and CT: meta-analysis of prospective studies. Radiology 247:64–79
Qiu Y, Mao R, Chen BL et al (2014) Systematic review with meta-analysis: magnetic resonance enterography vs. computed tomography enterography for evaluating disease activity in small bowel Crohn’s disease. Aliment Pharmacol Ther 40:134–146
Dillman JR, Smith EA, Sanchez RJ et al (2015) Pediatric small bowel Crohn disease: correlation of US and MR enterography. Radiographics 35:835–848
Ahmad TM, Greer M-L, Walters TD et al (2016) Bowel sonography and MR enterography in children. AJR Am J Roentgenol 206:173–181
Mann GS, Greer MC, Nadel HR (2015) Paediatric Crohn’s disease. In: Rajesh A, Sinha R (eds) Crohn’s disease: current concepts. Springer, Cham, pp 130–135
Absah I, Bruining DH, Matsumoto JM et al (2012) MR enterography in pediatric inflammatory bowel disease: retrospective assessment of patient tolerance, image quality, and initial performance estimates. AJR Am J Roentgenol 199:W367–W375
Torkzad MR, Masselli G, Halligan S et al (2015) Indications and selection of MR enterography vs. MR enteroclysis with emphasis on patients who need small bowel MRI and general anaesthesia: results of a survey. Insights Imaging 6:339–346
Amzallag-Bellenger E, Oudjit A, Ruiz A et al (2012) Effectiveness of MR enterography for the assessment of small-bowel diseases beyond Crohn disease. Radiographics 32:1423–1444
Anupindi SA, Podberesky DJ, Towbin AJ et al (2015) Pediatric inflammatory bowel disease: imaging issues with targeted solutions. Abdom Imaging 40:975–992
Mollard BJ, Smith EA, Dillman JR (2015) Pediatric MR enterography: technique and approach to interpretation — how we do it. Radiology 274:29–43
de Bie CI, Paerregaard A, Kolacek S et al (2013) Disease phenotype at diagnosis in pediatric Crohn’s disease: 5-year analyses of the EUROKIDS registry. Inflamm Bowel Dis 19:378–385
Greer MC, Krajewski D, Brown N et al (2014) MRE tour at SickKids. https://www.youtube.com/watch?v=9CHml_CrAEQ. Accessed 19 Feb 2016
Carter AJ, Greer ML, Gray SE et al (2010) Mock MRI: reducing the need for anaesthesia in children. Pediatr Radiol 40:1368–1374
Courtier J, Cardenas A, Tan C et al (2015) Nonanesthesia magnetic resonance enterography in young children: feasibility, technique, and performance. J Pediatr Gastroenterol Nutr 60:754–761
Mollard BJ, Smith EA, Lai ME et al (2016) MR enterography under the age of 10 years: a single institutional experience. Pediatr Radiol 46:43–49
Rajesh A, Sinha R (2015) CT and magnetic resonance enterography in Crohn’s disease. In: Rajesh A, Sinha R (eds) Crohn’s disease: current concepts. Springer, Cham, pp 75–80
Grand DJ, Guglielmo FF, Al-Hawary MM (2015) MR enterography in Crohn’s disease: current consensus on optimal imaging technique and future advances from the SAR Crohn’s disease-focused panel. Abdom Imaging 40:953–964
Ko HS, Greer MC, Aziza A et al (2011) 3% sorbitol as oral contrast and IV hyoscine butylbromide are well tolerated in children undergoing MR enterography. Pediatr Radiol 41:S311–S428
Masselli G, Gualdi G (2012) MR imaging of the small bowel. Radiology 264:333–348
Riordan RD, Khonsari M, Jeffries J et al (2004) Pineapple juice as a negative oral contrast agent in magnetic resonance cholangiopancreatography: a preliminary evaluation. Br J Radiol 77:991–999
Kuehle CA, Ajaj W, Ladd SC et al (2006) Hydro-MRI of the small bowel: effect of contrast volume, timing of contrast administration, and data acquisition on bowel distention. AJR Am J Roentgenol 187:W375–W385
Kinner S, Kuehle CA, Herbig S et al (2008) MRI of the small bowel: can sufficient bowel distension be achieved with small volumes of oral contrast? Eur Radiol 18:2542–2548
Young BM, Fletcher JG, Booya F et al (2008) Head-to-head comparison of oral contrast agents for cross-sectional enterography: small bowel distention, timing, and side effects. J Comput Assist Tomogr 32:32–38
Siddiki H, Fidler J (2009) MR imaging of the small bowel in Crohn’s disease. Eur J Radiol 69:409–417
Dillman JR, Smith EA, Khalatbari S et al (2013) I.V. glucagon use in pediatric MR enterography: effect on image quality, length of examination, and patient tolerance. AJR Am J Roentgenol 201:185–189
Grand DJ, Beland MD, Machan JT et al (2012) Detection of Crohn’s disease: comparison of CT and MR enterography without anti-peristaltic agents performed on the same day. Eur J Radiol 81:1735–1741
(2003) Glucagon for injection (rDNA origin). U.S. Food and Drug Administration website. http://www.accessdata.fda.gov/drugsatfda_docs/label/2004/20928slr010_glucagon_lbl.pdf. Accessed 19 Feb 2016
Tytgat GN (2008) Hyoscine butylbromide — a review on its parenteral use in acute abdominal spasm and as an aid in abdominal diagnostic and therapeutic procedures. Curr Med Res Opin 24:3159–3173
Froehlich JM, Daenzer M, von Weymarn C et al (2009) Aperistaltic effect of hyoscine N-butylbromide versus glucagon on the small bowel assessed by magnetic resonance imaging. Eur Radiol 19:1387–1393
Seo N, Park SH, Kim KJ et al (2015) MR enterography for the evaluation of small-bowel inflammation in Crohn disease by using diffusion-weighted imaging without intravenous contrast material: a prospective noninferiority study. Radiology 278:762–772
Taylor SA, Punwani S, Rodriguez-Justo M et al (2009) Mural Crohn disease: correlation of dynamic contrast-enhanced MR imaging findings with angiogenesis and inflammation at histologic examination — pilot study. Radiology 251:369–379
Oto A, Kayhan A, Williams JT et al (2011) Active Crohn’s disease in the small bowel: evaluation by diffusion weighted imaging and quantitative dynamic contrast enhanced MR imaging. J Magn Reson Imaging 33:615–624
Radbruch A, Weberling LD, Kieslich PJ et al (2015) Gadolinium retention in the dentate nucleus and globus pallidus is dependent on the class of contrast agent. Radiology 275:783–791
Patak MA, von Weymarn C, Froehlich JM (2007) Small bowel MR imaging: 1.5T versus 3T. Magn Reson Imaging Clin N Am 15:383–393
Morani AC, Smith EA, Ganeshan D et al (2015) Diffusion-weighted MRI in pediatric inflammatory bowel disease. AJR Am J Roentgenol 204:1269–1277
Freiman M, Perez-Rossello JM, Callahan MJ et al (2013) Characterization of fast and slow diffusion from diffusion-weighted MRI of pediatric Crohn’s disease. J Magn Reson Imaging 37:156–163
Rosenbaum DG, Rose ML, Solomon AB et al (2015) Longitudinal diffusion-weighted imaging changes in children with small bowel Crohn’s disease: preliminary experience. Abdom Imaging 40:1075–1080
Adler J, Swanson SD, Schmiedlin-Ren P et al (2011) Magnetization transfer helps detect intestinal fibrosis in an animal model of Crohn’s disease. Radiology 259:127–135
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The author has no financial interests or investigational uses to disclose. Off-label use of hyoscine-N-butylbromide is discussed.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix 1
3% Sorbitol oral contrast preparation. Abbreviation: W/V - weight per volume. (GIF 26 kb)
Supplementary online material
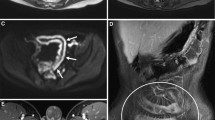
(movie clip) Coronal cine steady-state free precession image acquired at 1.5 T demonstrates a distal ileal stricture in a 17-year-old girl with Crohn disease. Each image slice is acquired as 40 images over 12 seconds, with 5–7 slices at a slice thickness of 10–15 mm (MOV 1404 kb)
Rights and permissions
About this article
Cite this article
Greer, ML.C. How we do it: MR enterography. Pediatr Radiol 46, 818–828 (2016). https://doi.org/10.1007/s00247-016-3596-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-016-3596-9