Abstract
Background
The cardiothoracic ratio by chest radiograph is widely used as a marker of cardiac size.
Objective
The purpose of this study is to correlate cardiothoracic ratio and cardiac volumes as measured by cardiovascular magnetic resonance (MR) in common structural and myopathic heart disease with increased cardiac size due to volume overload or hypertrophy.
Material and methods
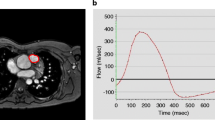
A retrospective single center study was performed in all patients between 2007 and 2013 with repaired tetralogy of Fallot (TOF), aortic regurgitation, isolated left-to-right shunt and hypertrophic cardiomyopathy (HCM) who underwent cardiovascular MR and chest radiograph within 6 months of each other. Cardiothoracic ratios by chest radiograph (frontal and lateral) were compared to cardiac volumes (indexed for body surface area) by cardiovascular MR.
Results
One hundred twenty-seven patients (mean age: 11.2 ± 5.5 years) were included in this study (76 with TOF, 23 with isolated left-to-right shunt, 16 with aortic regurgitation and 12 with HCM). Frontal cardiothoracic ratio of all groups correlated with indexed right ventricular (RV) end-diastolic volume (EDVI) (r = 0.40, P < 0.01) and indexed total heart volume (THVI) (r = 0.27, P < 0.01). In TOF patients, frontal cardiothoracic ratio correlated with RVEDVI (r = 0.34, P < 0.01; coefficient of variation = 27.6%), indexed RV end-systolic volume (ESVI) (r = 0.44, P < 0.01; coefficient of variation = 33.3%) and THVI (r = 0.35, P < 0.01; coefficient of variation = 19.6%), although RV volumes and THVI showed widespread variation given the high coefficients of variation. In patients with aortic regurgitation, frontal cardiothoracic ratio correlated with left ventricular (LV) EDVI (r = 0.50, P = 0.047), but not with THVI and aortic regurgitant fraction, and widespread variation for LV EDVI (coefficient of variation = 19.2%), LV ESVI (coefficient of variation = 32.5%) and THVI (coefficient of variation = 13.6%) was also observed. Frontal cardiothoracic ratio was not correlated with cardiac volumes or mass in patients with a left-to-right shunt or HCM. Lateral cardiothoracic ratio showed no correlation with any cardiac volume in all four groups.
Conclusion
Although increased cardiothoracic ratio on frontal chest radiograph is associated with increased biventricular volumes in patients with pulmonary and aortic regurgitation, significant variation in ventricular volumes and total heart volume for any given frontal cardiothoracic ratio limits the use of cardiothoracic ratio in monitoring the individual patient’s heart size. Frontal cardiothoracic ratio did not correlate with cardiac chamber volumes in patients with a left-to-right shunt or HCM and lateral cardiothoracic ratio offered no additional value for cardiac size assessment.





Similar content being viewed by others
Abbreviations
- EF:
-
Ejection fraction
- EDVI:
-
End-diastolic volume
- ESVI:
-
End-systolic volume
- HCM:
-
Hypertrophic cardiomyopathy
- LAVI:
-
Indexed left atrial volume
- LVMI:
-
Indexed left ventricular myocardial mass
- LVMVI:
-
Indexed left ventricular myocardial volume
- RAVI:
-
Indexed right atrial volume
- THVI:
-
Indexed total heart volume
- LV:
-
Left ventricular
- Qp:
-
Pulmonary blood flow
- RV:
-
Right ventricular
- Qs:
-
Systemic blood flow
- TOF:
-
Tetralogy of Fallot
References
Yoo SJ, MacDonald C, Babyn P (2009) Heart size, overall configuration and specific chamber enlargement. In: Chest radiographic interpretation in pediatric cardiac patients. Thieme, New York, pp 79–105
Jun SJ, Jeong HC, Ku YH et al (2013) An optimal cardiothoracic ratio cut-off to predict clinical outcomes in patients with acute myocardial infarction. Int J Cardiovasc Imaging 29:1889–1897
Dimopoulos K, Giannakoulas G, Bendayan I et al (2013) Cardiothoracic ratio from postero-anterior chest radiographs: a simple, reproducible and independent marker of disease severity and outcome in adults with congenital heart disease. Int J Cardiol 20:453–457
Spiewak M, Małek LA, Biernacka EK et al (2014) Cardiothoracic ratio may be misleading in the assessment of right- and left-ventricular size in patients with repaired tetralogy of Fallot. Clin Radiol 69:e1–8
Kono T, Suwa M, Hanada H et al (1992) Clinical significance of normal cardiac silhouette in dilated cardiomyopathy–evaluation based upon echocardiography and magnetic resonance imaging. Jpn Circ J 56:359–365
Clark AL, Coats AJ (2000) Unreliability of cardiothoracic ratio as a marker of left ventricular impairment: comparison with radionuclide ventriculography and echocardiography. Postgrad Med J 76:289–291
Fukuta H, Ohte N, Brucks S et al (2007) Contribution of right-sided heart enlargement to cardiomegaly on chest roentgenogram in diastolic and systolic heart failure. Am J Cardiol 99:62–67
Zaman MJ, Sanders J, Crook AM et al (2007) Cardiothoracic ratio within the “normal” range independently predicts mortality in patients undergoing coronary angiography. Heart 93:491–494
Giamouzis G, Sui X, Love TE et al (2008) A propensity-matched study of the association of cardiothoracic ratio with morbidity and mortality in chronic heart failure. Am J Cardiol 101:343–347
Lee W, Yoo SJ, Roche SL et al (2013) Determinants and functional impact of restrictive physiology after repair of tetralogy of Fallot: new insights from magnetic resonance imaging. Int J Cardiol 167:1347–1353
Gulati A, Ismail TF, Jabbour A et al (2013) Clinical utility and prognostic value of left atrial volume assessment by cardiovascular magnetic resonance in non-ischaemic dilated cardiomyopathy. Eur J Heart Fail 15:660–670
Oosterhof T, van Straten A, Vliegen HW et al (2007) Preoperative thresholds for pulmonary valve replacement in patients with corrected tetralogy of Fallot using cardiovascular magnetic resonance. Circulation 116:545–551
Apitz C, Webb GD, Redington AN (2009) Tetralogy of fallot. Lancet 374:1462–1471
Hemingway H, Shipley M, Christie D et al (1998) Cardiothoracic ratio and relative heart volume as predictors of coronary heart disease mortality. The Whitehall study 25 year follow-up. Eur Heart J 19:859–869
Maron BJ, Maron MS (2013) Hypertrophic cardiomyopathy. Lancet 381:242–255
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Grotenhuis, H.B., Zhou, C., Tomlinson, G. et al. Cardiothoracic ratio on chest radiograph in pediatric heart disease: How does it correlate with heart volumes at magnetic resonance imaging?. Pediatr Radiol 45, 1616–1623 (2015). https://doi.org/10.1007/s00247-015-3386-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-015-3386-9