Abstract
Background
Aspiration of liquids is a serious complication of neurological impairments such as traumatic brain injury or stroke. Carbonated liquids have been examined as a possible alternative to thickened liquids to help reduce aspiration in cases of dysphagia in adults, but no published literature to the best of our knowledge has evaluated this technique in children. If carbonated liquids result in safer swallowing in children, they could provide a preferred alternative to thickened liquids.
Objective
This pilot study examined whether carbonated thin liquids (CARB) improved swallowing compared to non-carbonated thin liquids (NOCARB) for children with neurogenic dysphagia.
Materials and methods
Twenty-four children admitted to a level I trauma center for acute neurological injury/disease were evaluated via videofluoroscopic swallow studies. Four descriptive outcome measures were contrasted.
Results
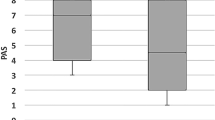
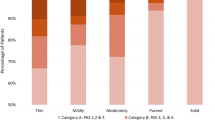
CARB significantly decreased pooling (P = 0.0006), laryngeal penetration/aspiration (P = 0.0044) and Penetration-Aspiration Scale scores (P = 0.0127) when compared to NOCARB. On average, CARB improved scores on the Penetration-Aspiration Scale by 3.7 points for participants who aspirated NOCARB. There was no significant difference in pharyngeal residue noted between CARB and NOCARB (P = 0.0625).
Conclusion
These findings support the hypothesis that carbonated thin liquids may provide an alternative to thickened liquids for children with neurogenic dysphagia. Implications for future research and clinical practice are discussed.
Similar content being viewed by others
References
Morgan AT (2010) Dysphagia in childhood traumatic brain injury: a reflection on the evidence and its implications for practice. Dev Neurorehabil 3:192–203
Plowman EK, Mehdizadeh O, Leder SB et al (2012) A bibliometric review of published abstracts presented at the dysphagia research society: 2001-2011. Dysphagia 28:128–130
Ylvisaker M, Logemann JA (1985) Therapy for feeding and swallowing disorders following head injury. In: Ylsivaker M (ed) Head injury rehabilitation: children and adolescents. College-Hill Press, Boston, pp 195–215
Dodds WJ, Logemann JA, Stewart E (1990) Radiologic assessment of abnormal oral and pharyngeal phases of swallowing. AJR Am J Roentgenol 5:965–974
Morgan A, Ward E, Murdoch B et al (2003) Incidence, characteristics, and predictive factors for dysphagia after pediatric traumatic brain injury. J Head Trauma Rehabil 3:239–251
Arvedson J, Rogers B, Buck G et al (1994) Silent aspiration prominent in children with dysphagia. Int J Pediatr Otorhinolaryngol 2-3:173–181
Weir K, McMahon S, Barry L et al (2007) Oropharyngeal aspiration and pneumonia in children. Pediatr Pulmonol 11:1024–1031
Dusick A (2003) Investigation and management of dysphagia. Semin Pediatr Neurol 4:255–264
Carrau RL, Murry T (eds) (1999) Comprehensive management of swallowing disorders. Plural Publishing, San Diego
Arvedson JC (2008) Assessment of pediatric dysphagia and feeding disorders: clinical and instrumental approaches. Dev Disabil Res Rev 2:118–127
Rogers B, Arvedson J (2005) Assessment of infant oral sensorimotor and swallowing function. Ment Retard Dev Disabil Res Rev 1:74–82
Tutor JD, Gosa MM (2012) Dysphagia and aspiration in children. Pediatr Pulmonol 4:321–337
Smith Hammond CA, Goldstein LB (2006) Cough and aspiration of food and liquids due to oral-pharyngeal dysphagia: ACCP evidence-based clinical practice guidelines. Chest 129:154S–168S
Robey RR (2004) A five-phase model for clinical-outcome research. J Commun Disord 5:401–411
Rosenbek JC, Robbins JA, Roecker EB et al (1996) A penetration-aspiration scale. Dysphagia 2:93–98
Bulow M, Olsson R, Ekberg O (2003) Videoradiographic analysis of how carbonated thin liquids and thickened liquids affect the physiology of swallowing in subjects with aspiration on thin liquids. Acta Radiol 44:366–372
Sdravou K, Walshe M, Dagdilelis L (2012) Effects of carbonated liquids on oropharyngeal swallowing measures in people with neurogenic dysphagia. Dysphagia 2:240–250
Martin-Harris B, Brodsky MB, Michel Y et al (2007) Delayed initiation of the pharyngeal swallow: normal variability in adult swallows. J Speech Lang Hear Res 3:585–594
Krival CR (2007) Effects of carbonated vs. thin and thickened liquids on swallowing in adults with neurogenic oropharyngeal dysphagia. Dissertation, University of Cincinnati. http://etd.ohiolink.edu
Eisenhuber E, Schima W, Schober E et al (2002) Videofluoroscopic assessment of patients with dysphagia: pharyngeal retention is a predictive factor for aspiration. AJR Am J Roentgenol 178:393–398
Gravetter FJ, Wallnau LB (2009) Statistics for the behavioral sciences. Wadsworth Cengage Learning, Belmont
Arvedson JC (1998) Management of pediatric dysphagia. Otolaryngol Clin N Am 3:453–476
Prasse JE, Kikano GE (2009) An overview of pediatric dysphagia. Clin Pediatr (Phila) 48:247–251
Ding R, Logemann JA, Larson CR et al (2003) The effects of taste and consistency on swallow physiology in younger and older healthy individuals: a surface electromyographic study. J Speech Lang Hear Res 46:977–989
Leow LP, Huckabee ML, Sharma S et al (2007) The influence of taste on swallowing apnea, oral preparation time, and duration and amplitude of submental muscle contraction. Chem Senses 32:119–128
Todd JT, Butler SG, Plonk DP (2012) Effects of chemesthetic stimuli mixtures with barium on swallowing apnea duration. Laryngoscope 10:2248–2251
Logemann JA, Pauloski BR, Colangelo L et al (1995) Effects of a sour bolus on oropharyngeal swallowing measures in patients with neurogenic dysphagia. J Speech Hear Res 38:556–563
Pelletier CA, Lawless HT (2003) Effect of citric acid and citric acid-sucrose mixtures on swallowing in neurogenic oropharyngeal dysphagia. Dysphagia 4:231–241
Chee C, Arshad S, Singh S et al (2005) The influence of chemical gustatory stimuli and oral anaesthesia on healthy human pharyngeal swallowing. Chem Senses 5:393–400
Pelletier CA, Dhanaraj GE (2006) The effect of taste and palatability on lingual swallowing pressure. Dysphagia 2:121–128
Swank Nixon T (1997) Use of carbonated liquids in the treatment of dysphagia. In: Network: a newsletter of dietetics in physical medicine and rehabilitation. American Dietetic Association, New York
Bradley RM (2000) Sensory receptors of the larynx. Am J Med 108:47S–50S
Mastan A, Michou E, Mistry S et al (2011) Evidence for an enhancing effect of carbonated liquids on complex human swallowing behavior. Gut 60:A162
Michou E, Mastan A, Ahmed S et al (2012) Examining the role of carbonation and temperature on water swallowing performance: a swallowing reaction-time study. Chem Senses 37:799–807
Newman L, Armstrong R, Rogers T et al (2001) The effect of carbonation on sensory dysphagia in the pediatric population: abstracts of scientific papers presented at the Ninth Annual Dysphagia Research Society Meeting, Savannah, Georgia, USA, October 26-28, 2000. Dysphagia 16:146–150
Krival K, Bates C (2012) Effects of club soda and ginger brew on linguapalatal pressures in healthy swallowing. Dysphagia 2:228–239
Matsuo K, Palmer JB (2008) Anatomy and physiology of feeding and swallowing: normal and abnormal. Phys Med Rehabil Clin N Am 4:691–707, vii
Stephen JR, Taves DH, Smith RC et al (2005) Bolus location at the initiation of the pharyngeal stage of swallowing in healthy older adults. Dysphagia 4:266–272
Marik PE (2001) Aspiration pneumonitis and aspiration pneumonia. N Engl J Med 9:665–671
Hind JA, Gensler G, Brandt DK et al (2009) Comparison of trained clinician ratings with expert ratings of aspiration on videofluoroscopic images from a randomized clinical trial. Dysphagia 2:211–217
Rosenbek JC, Power M, Lefton-Greif M et al (2006) Translation to treatment: the clinical implications of penetration/aspiration. Clinical presentation at the Annual Convention of the American Speech Hearing Association, Miami, Florida, 16-18 Nov 2006
Gosa MM, Suiter DM (2011) Reliability of the penetration-aspiration scale for use with pediatric populations. Paper presented at the Annual Convention of the American Speech Hearing Association, San Diego, 16-19 Nov 2011
Weir KA, McMahon S, Taylor S et al (2011) Oropharyngeal aspiration and silent aspiration in children. Chest 140:589–597
Osborn AJ, de Alarcon A, Tabangin ME et al (2014) Swallowing function after laryngeal cleft repair: more than just fixing the cleft. Laryngoscope 124:1965–1969
Daniels SK, Schroeder MF, McClain M et al (2006) Dysphagia in stroke: development of a standard method to examine swallowing recovery. J Rehabil Res Dev 3:347–356
Pearson WG, Molfenter SM, Smith ZM et al (2013) Image-based measurement of post-swallow residue: the normalized residue ratio scale. Dysphagia 28:167–177
Amis ES, Butler PF, Applegate KE et al (2007) American College of Radiology white paper on radiation dose in medicine. J Am Coll Radiol 4:272–284
Strauss KJ, Kaste SC (2006) The ALARA (as low as reasonably achievable) concept in pediatric interventional and fluoroscopic imaging: Striving to keep radiation dose as low as possible during fluoroscopy of pediatric patients – a white paper executive summary. Pediatr Radiol 36:110–112
Cohen MD (2007) Are we doing enough to minimize fluoroscopic radiation exposure in children? Pediatr Radiol 37:1020–1024
Cohen MD (2009) Can we use pulsed fluoroscopy to decrease the radiation dose during video fluoroscopic feeding studies in children? Clin Radiol 64:70–73
Bonilha HS, Blair J, Carnes B et al (2013) Preliminary investigation of the effect of pulse rate on judgments of swallowing impairment and treatment recommendations. Dysphagia 28:528–538
Ohio Administrative Code (2011) Chap5101:3-10-26: medical supplies, durable medical equipment, orthoses, and prosthesis providers: enteral nutritional products. http://codesohiogov/oac/5101%3A3-10-26, 2011. Accessed 20 Jan 2013
Acknowledgments
This project was funded in part by the Maternal and Child Health Bureau Grant T73MC00049 and CTSA grant UL1TR001070.
Jennifer P. Lundine would like to thank the following people for their support with the organization and analysis of this study: Kelsey Egelhoff, PhD, Michael Trudeau, PhD, Linda Lowes, PhD, Adriane Baylis, PhD, Tamela Thompson, MA, Stephanie Oswald, MA, and Caitlin Sirois, MS. Much gratitude to Brad Hoehne in the Department of Radiology for his assistance with the video edits required for this study.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
NOCARB via spoon, slowed by 50%. Vallecular/pyriform pooling prior to swallow. Aspiration on last swallow. (MP4 21102 kb)
ESM 2
CARB via spoon, slowed by 50%. Residue from aspiration with NOCARB present on surface of vocal folds prior to first swallow. No pyriform pooling prior to swallow. No new laryngeal penetration or aspiration observed. (MP4 14505 kb)
Rights and permissions
About this article
Cite this article
Lundine, J.P., Bates, D.G. & Yin, H. Analysis of carbonated thin liquids in pediatric neurogenic dysphagia. Pediatr Radiol 45, 1323–1332 (2015). https://doi.org/10.1007/s00247-015-3314-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-015-3314-z