Abstract
Background
Deep white matter hemorrhagic venous infarction with subsequent cavitation due to necrosis and liquefaction has been described in neonates and may be associated with infection and meningitis. In our experience, the MRI pattern of these lesions is confused with the pattern seen with cerebral abscesses.
Objective
The purpose of our study was to characterize the MRI findings of post infarction necrosis and liquefaction after hemorrhagic deep white matter venous infarction in infants and to distinguish these lesions from cerebral abscesses.
Materials and methods
An institutional review board approved a retrospective review of imaging records to identify all patients with cerebral venous infarction at a children’s hospital during a 10-year period. Nine infants had deep white matter hemorrhagic venous infarction with white matter fluid signal cavitary lesions. A diagnosis of cerebral abscess was considered in all. The imaging and laboratory findings in these patients are reviewed and compared to descriptions of abscesses found in the literature.
Results
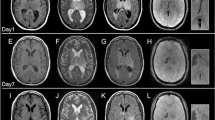
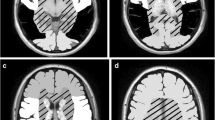
There were six female and three male infants. The mean age at presentation was 20 days (range: 0–90 days), while the corrected age at presentation was less than 30 days for all patients. Seven patients presented with seizures and signs of infection; one infant presented with lethargy and later proved to have protein C deficiency. MRI was performed 0–12 days from presentation in these eight patients. Another patient with known protein C deficiency underwent MRI at 30 days for follow-up of screening US abnormalities. There were a total of 38 deep cerebral white matter fluid signal cavitary lesions: 25 frontal, 9 parietal, 2 temporal, 2 occipital. Larger lesions had dependent debris. All lesions had associated hemorrhage and many lesions had evidence of adjacent small vessel venous thrombosis. Lesions imaged after gadolinium showed peripheral enhancement. Three lesions increased in size on follow-up imaging. Three patients, two with meningitis confirmed via microbiology and one with presumed meningitis by CSF counts, underwent surgical aspiration of a total of six lesions. All specimens were sent for pathology and culture and were negative for microorganisms.
Conclusion
Recognizing the MR appearance of cavitary necrosis and liquefaction after deep white matter cerebral venous infarction in neonates can distinguish this entity from cerebral abscess and potentially avoid an unnecessary neurosurgical aspiration procedure.




Similar content being viewed by others
References
Barron TF, Gusnard DA, Zimmerman RA et al (1992) Cerebral venous thrombosis in neonates and children. Pediatr Neurol 8:112–116
Sébire G, Tabarki B, Saunders DE et al (2005) Cerebral venous sinus thrombosis in children: risk factors, presentation, diagnosis and outcome. Brain 128:477–489
Wasay M, Dai AI, Ansari M et al (2008) Cerebral venous sinus thrombosis in children: a multicenter cohort from the United States. J Child Neurol 23:26–31
Berfelo FJ, Kersbergen KJ, van Ommen CH et al (2011) Neonatal cerebral sinovenous thrombosis from symptom to outcome. Stroke 41:1382–1388
Burger PC, Graham DG, Burch JG et al (1978) Hemorrhagic cerebral white matter: infarction with cerebral deep venous thrombosis and hypoxia. Arch Pathol Lab Med 102:40–42
Jan W, Zimmerman RA, Bilaniuk LT et al (2003) Diffusion-weighted imaging in acute bacterial meningitis in infancy. Neuroradiology 45:634–639
Triulzi F, Parazzini C, Righini A (2006) Patterns of damage in the mature neonatal brain. Pediatr Radiol 36:608–620
Kersbergen KJ, Groenendaal F, Benders MJ et al (2011) The spectrum of associated brain lesions in cerebral sinovenous thrombosis: relation to gestational age and outcome. Arch Dis Child Fetal Neonatal Ed 96:404–409
Teksam M, Moharir M, Deveber G et al (2008) Frequency and topographic distribution of brain lesions in pediatric cerebral venous thrombosis. AJNR Am J Neuroradiol 29:1961–1965
Nagaraj UD, Rusin JA, McBride KL et al (2013) Magnetic resonance imaging in neonatal citrullinemia. J Pediatr Neurol 2:169–173
Rutherford MA, Supramaniam V, Ederies A et al (2010) Magnetic resonance imaging of white matter diseases of prematurity. Neuroradiology 52:505–521
Hedlund GL, Boyer RS (1999) Neuroimaging of postnatal pediatric central nervous system infections. Semin Pediatr Neurol 6:299–317
Eason JD, Peacock D (1996) Plesiomonas shigelloides septicemia and meningitis in a neonate. Can J Infect Dis 7:380–382
Burdette JH, Santos C (2000) Enterobacter sakazakii brain abscess in the neonate: the importance of neuroradiologic imaging. Pediatr Radiol 30:33–34
Fanning NF, Laffan EE, Shroff MM (2006) Serial diffusion-weighted MRI correlates with clinical course and treatment response in children with intracranial pus collections. Pediatr Radiol 36:26–37
de Oliveira RS, Pinho VF, Madureira JF et al (2007) Brain abscess in a neonate: an unusual presentation. Childs Nerv Syst 23:139–142
Takeuchi H, Fujita Y, Ogawa H et al (2009) Multiple brain abscesses in neonate caused by Edwardsiella tarda: case report. Neurol Med Chir (Tokyo) 49:85–89
Drazin D, Lehman D, Danielpour M (2010) Successful surgical drainage and aggressive medical therapy in a preterm neonate with Bacillus cereus meningitis. Pediatr Neurosurg 46:466–471
Phan H, Lehman D (2012) Cerebral abscess complicating Proteus mirabilis meningitis in a newborn infant. J Child Neurol 27:405–407
Qureshi UA, Wani NA, Charoo BA et al (2011) Klebsiella brain abscess in a neonate. Arch Dis Child Fetal Neonatal Ed 96:F19
Barnes PD, Poussaint TY, Burrows PE (1994) Imaging of pediatric central nervous system infections. Neuroimaging Clin N Am 4:367–391
Hernández MI, Sandoval CC, Tapia JL et al (2011) Stroke patterns in neonatal group B streptococcal meningitis. Pediatr Neurol 44:282–288
Blaser S, Jay V, Becker LE et al (2002) Neonatal brain infection. In: Rutherford M (ed) MRI of the neonatal brain. Saunders, London, pp 201–223
Willis J, Robinson JE (1988) Enterobacter sakazakii meningitis in neonates. Pediatr Infect Dis J 7:196–199
Meier A, Chusid MJ, Sty JR (1998) Neonatal citrobacter meningitis: neurosonographic observations. J Ultrasound Med 17:399–401
Gallagher PG, Ball WS (1991) Cerebral infarctions due to CNS infection with Enterobacter sakazakii. Pediatr Radiol 21:135–136
Britt RH, Enzmann DR, Yeager AS (1981) Neuropathological and computerized tomographic findings in experimental brain abscess. J Neurosurg 55:590–603
Haimes AB, Zimmerman RD, Morgello S et al (1989) MR imaging of brain abscesses. AJR Am J Roentgenol 152:1073–1085
Dev R, Gupta RK, Poptani H et al (1998) Role of in vivo proton magnetic resonance spectroscopy in the diagnosis and management of brain abscesses. Neurosurgery 42:37–42
Pal D, Bhattacharyya A, Husain M et al (2010) In vivo proton MR spectroscopy evaluation of pyogenic brain abscesses: a report of 194 cases. AJNR Am J Neuroradiol 31:360–366
Abou Zeid N, Pirko I, Erickson B et al (2012) Diffusion-weighted imaging characteristics of biopsy-proven demyelinating brain lesions. Neurology 78:1655–1662
Hartmann M, Jansen O, Heiland S et al (2001) Restricted diffusion within ring enhancement is not pathognomonic for brain abscess. AJNR Am J Neuroradiol 22:1738–1742
Burtscher IM, Holtås S (1999) In vivo proton MR spectroscopy of untreated and treated brain abscesses. AJNR Am J Neuroradiol 20:1049–1053
Forbes KP, Pipe JG, Heiserman JE (2001) Evidence for cytotoxic edema in the pathogenesis of cerebral venous infarction. AJNR Am J Neuroradiol 22:450–455
Atlas SW, DuBois P, Singer MB et al (2000) Diffusion measurements in intracranial hematomas: implications for MR imaging of acute stroke. AJNR Am J Neuroradiol 21:1190–1194
Hsu LC, Lirng JF, Fuh JL et al (1998) Proton magnetic resonance spectroscopy in deep cerebral venous thrombosis. Clin Neurol Neurosurg 100:27–30
Govaert P, Ramenghi L, Toal R et al (2009) Diagnosis of perinatal stroke 1: definitions, differential diagnosis and registration. Acta Paediatr 98:1720–1726
Gould SJ, Howard S, Hope PL et al (1987) Periventricular intraparenchymal cerebral haemorrhage in preterm infants: the role of venous infarction. J Pathol 151:197–202
Takashima S, Mito T, Ando Y (1986) Pathogenesis of periventricular white matter hemorrhages in preterm infants. Brain Dev 8:25–30
Dudink J, Lequin M, Weisglas-Kuperus N et al (2008) Venous subtypes of preterm periventricular haemorrhagic infarction. Arch Dis Child Fetal Neonatal Ed 93:201–206
Foreman SD, Smith EE, Ryan NJ et al (1984) Neonatal Citrobacter meningitis: pathogenesis of cerebral abscess formation. Ann Neurol 16:655–659
Acknowledgments
Presented at the Annual Meeting of the Society for Pediatric Radiology, San Francisco, CA April 17–20, 2012.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ruess, L., Dent, C.M., Tiarks, H.J. et al. Neonatal deep white matter venous infarction and liquefaction: a pseudo-abscess lesion. Pediatr Radiol 44, 1393–1402 (2014). https://doi.org/10.1007/s00247-014-3006-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-014-3006-0