Abstract
Background
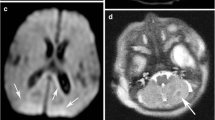
Gradient echo T2*-W sequences are more sensitive than T2-W spin-echo sequences for detecting hemorrhages in the brain.
Objective
The aim of this study is to correlate presence of hemosiderin deposits in the brain of very preterm infants (gestational age <32 weeks) detected by T2*-W gradient echo MRI to white matter injury and neurodevelopmental outcome at 2 years.
Materials and methods
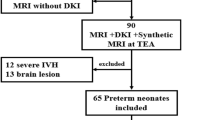
In 101 preterm infants, presence and location of hemosiderin were assessed on T2*-W gradient echo MRI performed around term-equivalent age (range: 40–60 weeks). White matter injury was defined as the presence of >6 non-hemorrhagic punctate white matter lesions (PWML), cysts and/or ventricular dilatation. Six infants with post-hemorrhagic ventricular dilatation detected by US in the neonatal period were excluded. Infants were seen for follow-up at 2 years. Univariate and regression analysis assessed the relation between presence and location of hemosiderin, white matter injury and neurodevelopmental outcome.
Results
In 38/95 (40%) of the infants, hemosiderin was detected. Twenty percent (19/95) of the infants were lost to follow-up. There was a correlation between hemosiderin in the ventricular wall with >6 PWML (P < 0.001) and cysts (P < 0.001) at term-equivalent age, and with a lower psychomotor development index (PDI) (P=0.02) at 2 years. After correcting for known confounders (gestational age, gender, intrauterine growth retardation and white matter injury), the correlation with PDI was no longer significant.
Conclusion
The clinical importance of detecting small hemosiderin deposits is limited as there is no independent association with neurodevelopmental outcome.




Similar content being viewed by others
References
Barkovich AJ, Maroldo TV (1993) Magnetic resonance imaging of normal and abnormal brain development. Top Magn Reson Imaging 5:96–122
Counsell SJ, Rutherford MA, Cowan FM et al (2003) Magnetic resonance imaging of preterm brain injury. Arch Dis Child Fetal Neonatal Ed 88:F269–F274
Rutherford M, Biarge MM, Allsop J et al (2010) MRI of perinatal brain injury. Pediatr Radiol 40:819–833
van Wezel-Meijler G, Leijser LM, de Bruïne FT et al (2009) Magnetic resonance imaging of the brain in newborn infants: practical aspects. Early Hum Dev 85:85–92
Dyet LE, Kennea N, Counsell SJ et al (2006) Natural history of brain lesions in extremely preterm infants studied with serial magnetic resonance imaging from birth and neurodevelopmental assessment. Pediatrics 118:536–548
Leijser LM, de Bruïne FT, Steggerda SJ et al (2009) Brain imaging findings in very preterm infants throughout the neonatal period: part I. Incidences and evolution of lesions, comparison between ultrasound and MRI. Early Hum Dev 85:101–109
Volpe JJ (2009) Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol 8:110–124
Grunnet ML, Shields WD (1976) Cerebellar hemorrhage in the premature infant. J Pediatr 88:605–608
Limperopoulos C, Benson CB, Bassan H et al (2005) Cerebellar hemorrhage in the preterm infant: ultrasonographic findings and risk factors. Pediatrics 116:717–724
Steggerda SJ, Leijser LM, Wiggers-de Bruïne FT (2009) Cerebellar injury in preterm infants: incidence and findings on US and MR images. Radiology 252:190–199
Tam EW, Rosenbluth G, Rogers EE (2011) Cerebellar hemorrhage on magnetic resonance imaging in preterm newborns associated with abnormal neurologic outcome. J Pediatr 158:245–250
Limperopoulos C, Bassan H, Gauvreau K et al (2007) Does cerebellar injury in premature infants contribute to the high prevalence of long-term cognitive, learning, and behavioral disability in survivors? Pediatrics 120:584–593
Miller SP, Ferriero DM (2009) From selective vulnerability to connectivity: insights from newborn brain imaging. Trends Neurosci 32:496–505
Tam EW, Miller SP, Studholme C et al (2011) Differential effects of intraventricular hemorrhage and white matter injury on preterm cerebellar growth. J Pediatr 158:366–371
Woodward LJ, Clark CA, Pritchard VE et al (2011) Neonatal white matter abnormalities predict global executive function impairment in children born very preterm. Dev Neuropsychol 36:22–41
Inder T, Mocatta T, Darlow B et al (2002) Elevated free radical products in the cerebrospinal fluid of VLBW infants with cerebral white matter injury. Pediatr Res 52:213–218
Savman K, Nilsson UA, Blennow M (2001) Non-protein-bound iron is elevated in cerebrospinal fluid from preterm infants with posthemorrhagic ventricular dilatation. Pediatr Res 49:208–212
Atlas SW, Mark AS, Grossman RI et al (1988) Intracranial hemorrhage: gradient-echo MR imaging at 1.5 T. Comparison with spin-echo imaging and clinical applications. Radiology 168:803–807
Greenberg SM, Vernooij MW, Cordonnier C (2009) Cerebral microbleeds: a guide to detection and interpretation. Lancet Neurol 8:165–174
Levene MI (1981) Measurement of the growth of the lateral ventricles in preterm infants with real-time ultrasound. Arch Dis Child 56:900–904
Leijser LM, de Bruïne FT, Steggerda SJ et al (2009) Brain imaging findings in very preterm infants throughout the neonatal period: part I. Incidences and evolution of lesions, comparison between ultrasound and MRI. Early Hum Dev 85:101–109
de Bruïne FT, van den Berg-Huysmans AA, Leijser LM et al (2011) Clinical implications of MR imaging findings in the white matter in very preterm infants: a 2-year follow-up study. Radiology 261:899–906
Palisano RJ, Hanna SE, Rosenbaum PL et al (2000) Validation of a model of gross motor function for children with cerebral palsy. Phys Ther 80:974–985
Achenbach TM, Ruffle TM (2000) The child behavior checklist and related forms for assessing behavioral/emotional problems and competencies. Pediatr Rev 21:265–271
Goos JD, van der Flier WM, Knol DL et al (2011) Clinical relevance of improved microbleed detection by susceptibility-weighted magnetic resonance imaging. Stroke 42:1894–1900
Haacke EM, Xu Y, Cheng YC et al (2004) Susceptibility weighted imaging (SWI). Magn Reson Med 52:612–618
Niwa T, Aida N, Takahara T et al (2010) Imaging and clinical characteristics of children with multiple foci of microsusceptibility changes in the brain on susceptibility-weighted MRI. Pediatr Radiol 40:1657–1662
Tong KA, Ashwal S, Obenaus A (2008) Susceptibility-weighted MR imaging: a review of clinical applications in children. AJNR Am J Neuroradiol 29:9–17
Niwa T, de Vries LS, Benders MJ et al (2011) Punctate white matter lesions in infants: new insights using susceptibility-weighted imaging. Neuroradiology 53:669–679
Beaino G, Khoshnood B, Kaminski M et al (2010) Predictors of cerebral palsy in very preterm infants: the EPIPAGE prospective population-based cohort study. Dev Med Child Neurol 52:e119–e125
Brouwer A, Groenendaal F, Van Haastert I et al (2008) Neurodevelopmental outcome of preterm infants with severe intraventricular hemorrhage and therapy for post-hemorrhagic ventricular dilatation. J Pediatr 152:648–654
de Vries LS, Van Haastert I, Rademaker KJ et al (2004) Ultrasound abnormalities preceding cerebral palsy in high-risk preterm infants. J Pediatr 144:815–820
Patra K, Wilson-Costello D, Taylor HG et al (2006) Grades I-II intraventricular hemorrhage in extremely low birth weight infants: effects on neurodevelopment. J Pediatr 149:169–173
Inder TE, Warfield SK, Wang H et al (2005) Abnormal cerebral structure is present at term in premature infants. Pediatrics 115:286–294
Ment LR, Hirtz D, Huppi PS (2009) Imaging biomarkers of outcome in the developing preterm brain. Lancet Neurol 8:1042–1055
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Bruïne, F.T., Steggerda, S.J., van den Berg-Huysmans, A.A. et al. Prognostic value of gradient echo T2* sequences for brain MR imaging in preterm infants. Pediatr Radiol 44, 305–312 (2014). https://doi.org/10.1007/s00247-013-2803-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-013-2803-1