Abstract
Background
The ability to lie still in an MRI scanner is essential for obtaining usable image data. To reduce motion, young children are often sedated, adding significant cost and risk.
Objective
We assessed the feasibility of using a simple and affordable behavioral desensitization program to yield high-quality brain MRI scans in sedation-free children.
Materials and methods
222 children (4–9.9 years), 147 with type 1 diabetes and 75 age-matched non-diabetic controls, participated in a multi-site study focused on effects of type 1 diabetes on the developing brain. T1-weighted and diffusion-weighted imaging (DWI) MRI scans were performed. All children underwent behavioral training and practice MRI sessions using either a commercial MRI simulator or an inexpensive mock scanner consisting of a toy tunnel, vibrating mat, and video player to simulate the sounds and feel of the MRI scanner.
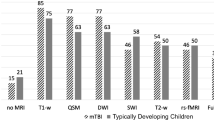
Results
205 children (92.3%), mean age 7 ± 1.7 years had high-quality T1-W scans and 174 (78.4%) had high-quality diffusion-weighted scans after the first scan session. With a second scan session, success rates were 100% and 92.5% for T1-and diffusion-weighted scans, respectively. Success rates did not differ between children with type 1 diabetes and children without diabetes, or between centers using a commercial MRI scan simulator and those using the inexpensive mock scanner.
Conclusion
Behavioral training can lead to a high success rate for obtaining high-quality T1-and diffusion-weighted brain images from a young population without sedation.


Similar content being viewed by others
References
Sun L (2010) Early childhood general anaesthesia exposure and neurocognitive development. Br J Anaesth 105:i61–i68
Loepke AW, Soriano SG (2008) An assessment of the effects of general anesthetics on developing brain structure and neurocognitive function. Anesth Analg 106:1681–1707
Rizzi S, Ori C, Jevtovic-Todorovic V (2010) Timing versus duration: Determinants of anesthesia-induced developmental apoptosis in the young mammalian brain. Ann N Y Acad Sci 1199:43–51
Jevtovic-Todorovic V, Hartman RE, Izumi Y et al (2003) Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci 23:876–882
Wilder RT, Flick RP, Sprung J et al (2009) Early exposure to anesthesia and learning disabilities in a population-based birth cohort. Anesthesiology 110:796–804
Kalkman CJ, Peelen L, Moons KG et al (2009) Behavior and development in children and age at the time of first anesthetic exposure. Anesthesiology 110:805–812
Bartels M, Althoff RR, Boomsma DI (2009) Anesthesia and cognitive performance in children: No evidence for a causal relationship. Twin Res Hum Genet 12:246–253
Cejda K, Smeltzer M, Hansbury E et al (2012) The impact of preparation and support procedures for children with sickle cell disease undergoing MRI. Pediatr Radiol 42:1223–1228
De Bie HM, Boersma M, Wattjes MP et al (2010) Preparing children with a mock scanner training protocol results in high quality structural and functional MRI scans. Eur J Pediatr 169:1079–1085
Carter AJ, Greer ML, Gray SE et al (2010) Mock MRI: Reducing the need for anaesthesia in children. Pediatr Radiol 40:1368–1374
Nordahl C, Simon T, Zierhut C et al (2008) Brief report: Methods for acquiring structural MRI data in very young children with autism without the use of sedation. J Autism Dev Disord 38:1581–1590
Wechsler D (2002) Wechsler preschool and primary scale of intelligence third edition. Psychological Corp, San Antonio
Wechsler D (1999) Wechsler adult scale of intelligence. Harcourt Brace & Co., Psychological Corp, New York
Racschle NM, Lee M, Buechler R et al (2009) Making MR imaging child’s play—pediatric neuroimaging protocol, guidelines and procedure. J Vis Exp 30:1–5
Jack CR Jr, Bernstein MA, Fox NC et al (2008) The alzheimer’s disease neuroimaging initiative (ADNI): MRI methods. J Magn Reson Imaging 27:685–691
Acknowledgements
The authors are grateful to the DirecNet study coordinators and research assistants for the recruitment, training and care of all children in the study, and to the radiology technologists who performed these scans. This research was supported by funding from Jaeb Center for Health Research and the National Institutes of Health (DIRECNET U01 HD41890, HD41890-10, HD41906-10, HD41908-10, HD41915, HD41918, HD56526) and UL1 RR024992. The DirecNet Study Group consists of the following groups and individuals (personnel are listed as PI for principal investigator, I for co-investigator and C for coordinators):
Department of Pediatrics, University of Iowa Carver College of Medicine, Iowa City, IA—Eva Tsalikian, MD (PI); Michael J. Tansey, MD (I); Julie Coffey, MSN (C); Joanne Cabbage (C); Sara Salamati (C).
Nemours Children’s Clinic, Jacksonville, FL—Nelly Mauras, MD (PI); Larry A. Fox, MD (I); Allison Cato, PhD (I); Kim Englert, RN, BSN, CDE (C); Kaitlin Sikes, ARNP, MSN (C); Tina Ewen (C).
Division of Pediatric Endocrinology and Diabetes, Stanford University, Stanford, CA—Bruce A. Buckingham, MD (PI); Darrell M. Wilson, MD (I); Tandy Aye, MD (I); Kimberly Caswell, ARNP (C).
Department of Pediatrics, Yale University School of Medicine, New Haven, CT—Stuart A. Weinzimer, MD (PI); William V. Tamborlane, MD (I); Amy Steffen, BS (C); Kate Weyman, MSN (C); Melinda Zgorski, BSN (C).
Washington University in St. Louis, St. Louis, MO—Neil H. White, MD, CDE (PI); Ana Maria Arbelaez, MD, (I); Lucy Levandoski, PA-C (C); Angie Starnes, RN, BSN, CDE (C), Tamara Hershey, PhD (I).
Coordinating Center, Jaeb Center for Health Research, Tampa, FL—Roy W. Beck, MD, PhD; Katrina J. Ruedy, MSPH; Craig Kollman, PhD; Peiyao Cheng, MPH; Beth Stevens.
Image Coordinating Center, Center for Interdisciplinary Brain Sciences Research at Stanford University—Allan L. Reiss, MD; Naama Barnea-Goraly, MD; Matthew J. Marzelli, BS; Paul M. Mazaika, PhD.
Conflicts of interest
None
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Barnea-Goraly, N., Weinzimer, S.A., Ruedy, K.J. et al. High success rates of sedation-free brain MRI scanning in young children using simple subject preparation protocols with and without a commercial mock scanner–the Diabetes Research in Children Network (DirecNet) experience. Pediatr Radiol 44, 181–186 (2014). https://doi.org/10.1007/s00247-013-2798-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-013-2798-7