Abstract
Background
There is a need for updated radiation dose estimates in pediatric fluoroscopy given the routine use of new dose-saving technologies and increased radiation safety awareness in pediatric imaging.
Objective
To estimate effective doses for standardized pediatric upper gastrointestinal (UGI) examinations at our institute using direct dose measurement, as well as provide dose-area product (DAP) to effective dose conversion factors to be used for the estimation of UGI effective doses for boys and girls up to 10 years of age at other centers.
Materials and methods
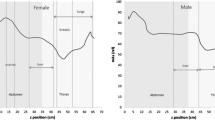
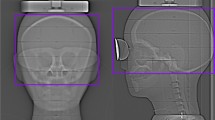
Metal oxide semiconductor field-effect transistor (MOSFET) dosimeters were placed within four anthropomorphic phantoms representing children ≤10 years of age and exposed to mock UGI examinations using exposures much greater than used clinically to minimize measurement error. Measured effective dose was calculated using ICRP 103 weights and scaled to our institution’s standardized clinical UGI (3.6-min fluoroscopy, four spot exposures and four examination beam projections) as determined from patient logs. Results were compared to Monte Carlo simulations and related to fluoroscope-displayed DAP.
Results
Measured effective doses for standardized pediatric UGI examinations in our institute ranged from 0.35 to 0.79 mSv in girls and were 3–8% lower for boys. Simulation-derived and measured effective doses were in agreement (percentage differences <19%, T > 0.18). DAP-to-effective dose conversion factors ranged from 6.5 ×10−4 mSv per Gy-cm2 to 4.3 × 10−3 mSv per Gy-cm2 for girls and were similarly lower for boys.
Conclusion
Using modern fluoroscopy equipment, the effective dose associated with the UGI examination in children ≤10 years at our institute is < 1 mSv. Estimations of effective dose associated with pediatric UGI examinations can be made for children up to the age of 10 using the DAP-normalized conversion factors provided in this study. These estimates can be further refined to reflect individual hospital examination protocols through the use of direct organ dose measurement using MOSFETs, which were shown to agree with Monte Carlo simulated doses.



Similar content being viewed by others
References
Council NR (2006) Health risks of exposure to low level of ionizing radiation. BEIR VII. National Academic Press, Washington, DC
International Commission on Radiological Protection (ICRP) (2007) The 2007 Recommendations of the ICRP, Annals of the ICRP. Publication 103. Elsevier, Amsterdam
Geleijns J, Broerse JJ, Chandie Shaw MP et al (1998) A comparison of patient dose for examinations of the upper gastrointestinal tract at 11 conventional and digital X-ray units in The Netherlands. Br J Radiol 71:745–753
Hart D, Wall BF (1994) Estimation of effective dose from dose-area product measurements for barium meals and barium enemas. Br J Radiol 67:485–489
Ruiz-Cruces R, Ruiz F, Perez-Martinez M et al (2000) Patient dose from barium procedures. Br J Radiol 73:752–761
Dimitriadis A, Gialousis G, Makri T et al (2011) Monte Carlo estimation of radiation doses during paediatric barium meal and cystourethrography examinations. Phys Med Biol 56:367–382
Strauss KJ (2006) Pediatric interventional radiography equipment: safety considerations. Pediatr Radiol 36:126–135
Hiorns MP, Saini A, Marsden PJ (2006) A review of current local dose-area product levels for paediatric fluoroscopy in a tertiary referral centre compared with national standards. Why are they so different? Br J Radiol 79:326–330
Peet D, Pryor MD (1999) Evaluation of a MOSFET radiation sensor for the measurement of entrance surface dose in diagnostic radiology. Br J Radiol 72:562–568
Yoshizumi T, Goodman PC, Frush DP et al (2007) Validation of metal oxide semiconductor field effect transistor technology for organ dose assessment during CT: comparison with thermoluminescent dosimetry. AJR Am J Roentgenol 188:1332–1336
Glennie D, Connolly BL, Gordon C (2008) Entrance skin dose measured with MOSFETs in children undergoing interventional radiology procedures. Pediatr Radiol 38:1180–1187
Lee R, Thomas K, Connolly B et al (2009) Effective dose estimation for pediatric voiding cystourethrography using an anthropomorphic phantom set and metal oxide semiconductor field-effect transistor (MOSFET) technology. Pediatr Radiol 39:608–615
Miksys N, Gordon CL, Thomas K et al (2010) Estimating effective dose to pediatric patients undergoing interventional radiology procedures using anthropomorphic phantoms and MOSFET dosimeters. AJR Am J Roentgenol 194:1315–1322
Gaca A, Jaffe TA, Delaney S et al (2008) Radiation doses from small-bowel follow-through and abdomen/pelvis MDCT in pediatric Crohn disease. Pediatr Radiol 38:285–291
Hollingsworth C, Yoshizumi TT, Frush DP et al (2007) Pediatric cardiac-gated CT angiography: assessment of radiation dose. AJR Am J Roentgenol 189:12–18
Varchena V (2002) Pediatric phantoms. Pediatr Radiol 32:280–284
Cygler J, Saoudi A, Perry G et al (2006) Feasibility study of using MOSFET detector for in vivo dosimetry during permanent low-dose-rate prostate implants. Radiother Oncol 80:296–301
Dong SL, Chu TC, Lan GY et al (2002) Characterization of high-sensitivity metal oxide semiconductor field effect transistor dosimeters system and LiF:Mg, Cu, P thermoluminescence dosimeters for use in diagnostic radiology. Appl Radiat Isotopes 57:883–891
Sessions J, Roshau JN, Tressler MA et al (2002) Comparisons of point and average organ dose within an anthropomorphic physical phantom and a computational model of the newborn patient. Med Phys 29:1080–1089
Jones A, Pazik FD, Hintenlang DE et al (2005) MOSFET dosimeter depth-dose measurements in heterogeneous tissue-equivalent phantoms at diagnostic X-ray energies. Med Phys 32:3209–3213
Cristy M (1981) Active bone marrow distribution as a function of age in humans. Phys Med Biol 26:389–400
Cristy M (1980) Mathematical phantoms representing children of various ages for use in estimating internal dose. In: Commission UNR (ed), Oak Ridge, TN
Ward V, Strauss KJ, Barnewolt CE et al (2008) Pediatric radiation exposure and effective dose reduction during voiding cystourethrography. Radiology 249:1002–1009
Newman B, John S, Goske M et al (2011) Pause and pulse: radiation dose in pediatric fluoroscopy. Pediatr Rev 32:e83–e90
Staton R, Williams JL, Arreola MM et al (2007) Organ and effective doses in infants undergoing upper gastrointestinal (UGI) fluoroscopic examination. Med Phys 34:703–710
Damilakis J, Stratakis J, Raissaki M et al (2006) Normalized dose data for upper gastrointestinal tract contrast studies performed to infants. Med Phys 33:1033–1040
Board NRP (2002) Doses to patients from medical X-ray examinations in the UK—2000 review. National Radiological Protection Board, Chilton
Delichas M, Hatziionannou K, Papanastassiou E et al (2004) Radiation doses to patients undergoing barium meal and barium enema examinations. Radiat Prot Dosim 109:243–247
Hall E (2002) Lessons we have learned from our children: cancer risks from diagnostic radiology. Pediatr Radiol 32:700–706
Perisinakis K, Raissaki M, Damilakis J et al (2006) Fluoroscopy-controlled voiding cystourethrography in infants and children: are the radiation risks trivial? Eur Radiol 16:846–851
Rosenstein M, Suleiman OH, Burkhart RL et al (1992) Handbook of selected tissue doses for the upper gastrointestinal fluoroscopic examination. In: Health CfDaR (ed), Rockville, MD
Conflicts of interest
Authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Emigh, B., Gordon, C.L., Connolly, B.L. et al. Effective dose estimation for pediatric upper gastrointestinal examinations using an anthropomorphic phantom set and metal oxide semiconductor field-effect transistor (MOSFET) technology. Pediatr Radiol 43, 1108–1116 (2013). https://doi.org/10.1007/s00247-013-2674-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-013-2674-5