Abstract
Background
The diagnosis of intestinal malrotation is based on an upper gastrointestinal contrast series (UGI), which is considered the imaging reference standard. It may however be challenging even for experienced paediatric radiologists.
Objective
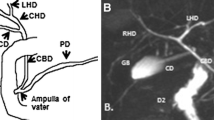
The purpose of this study was to demonstrate the agreement between UGI and US in assessing the position of the third portion of the duodenum (D3) and to show that a retroperitoneal duodenum indicates normal forgut rotation.
Materials and methods
In a prospective study, US assessment of the duodenum and the superior mesenteric vessels was performed in consecutive children who were referred for clinically indicated UGI at a single institution.
Results
Eighty-five children, 5 months to 14 years old, were studied. In 82/85 (96%), both US and UGI suggested normal forgut rotation. In three children, US demonstrated a normal position of the D3 whereas UGI showed an abnormal position of the duodeno-jejunal junction.
Conclusion
US is a non-invasive, easily performed technique for excluding malrotation. UGI may be reserved for situations where US does not demonstrate a normal position of the D3.






Similar content being viewed by others
References
Yousefzadeh DK, Soper RT, Jackson JH Jr (1980) Diagnostic advantages of manual compression fluoroscopy in the radiologic work-up of vomiting neonates. J Pediatr Surg 15:270–278
Katz ME, Siegel MJ, Shackelford GD et al (1987) The position and mobility of the duodenum in children. AJR 148:947–951
Loyer E, Eggli KD (1989) Sonographic evaluation of superior mesenteric vascular relationship in malrotation. Pediatr Radiol 19:173–175
Dufour D, Delaet MH, Dassonville M et al (1992) Midgut malrotation, the reliability of sonographic diagnosis. Pediatr Radiol 22:21–23
Millar AJ, Rode H, Brown RA et al (1987) The deadly vomit: malrotation and midgut volvulus. A review of 137 cases. Pediatr Surg Int 2:172–174
Rescorla FJ, Shedd FJ, Grosfeld JL et al (1990) Anomalies of intestinal rotation in childhood: analysis of 447 cases. Surgery 108:710–715
Long FR, Kramer SS, Markowitz RI et al (1996) Intestinal malrotation in children: tutorial on radiographic diagnosis in difficult cases. Radiology 198:775–780
Dilley AV, Pereira J, Shi EC et al (2000) The radiologist says malrotation: does the surgeon operate? Pediatr Surg Int 16:45–49
Ashley LM, Allen S, Teele RL (2001) A normal sonogram does not exclude malrotation. Pediatr Radiol 31:354–356
Strouse PJ (2004) Disorders of intestinal rotation and fixation ("malrotation"). Pediatr Radiol 34:837–851
Applegate KE, Anderson JM, Klatte EC (2006) Intestinal malrotation in children: a problem-solving approach to the upper gastrointestinal series. Radiographics 26:1485–1500
Orzech N, Navarro OM, Langer JC (2006) Is ultrasonography a good screening test for intestinal malrotation? J Pediatr Surg 41:1005–1009
Daneman A (2009) Malrotation: the balance of evidence. Pediatr Radiol 39(Suppl 2):S164–S166
Pracros JP, Sann L, Genin G et al (1992) Ultrasound diagnosis of midgut volvulus: the "whirlpool" sign. Pediatr Radiol 22(1):18–20
Shimanuki Y, Aihara T et al (1996) Clockwise whirlpool sign at color Doppler US: an objective and definite sign of midgut volvulus. Radiology 199(1):261–264
Yousefzadeh DK (2009) The position of the duodenojejunal junction: the wrong horse to bet on in diagnosing or excluding malrotation. Pediatr Radiol 39(Suppl 2):S172–S177
Yousefzadeh DK, Kang L, Tessicini L (2010) Assessment of retromesenteric position of the third portion of the duodenum: an US feasibility study in 33 newborns. Pediatr Radiol 40:1476–1484
Applegate KE (2009) Evidence-based diagnosis of malrotation and volvulus. Pediatr Radiol 39(Suppl 2):S161–S163
Taylor GA (2011) CT appearance of the duodenum and mesenteric vessels in children with normal and abnormal bowel. Pediatr Radiol 41:1378–1383
Yousefzadeh DK (2011) Regarding online publication of ‘CT appearance of the duodenum and mesenteric vessels in children with normal and abnormal bowel’. Pediatr Radiol 41:1481–1482
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Menten, R., Reding, R., Godding, V. et al. Sonographic assessment of the retroperitoneal position of the third portion of the duodenum: an indicator of normal intestinal rotation. Pediatr Radiol 42, 941–945 (2012). https://doi.org/10.1007/s00247-012-2403-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-012-2403-5