Abstract
Background
Digital radiography (DR) is one of several new products that have changed our work processes from hard copy to digital formats. The transition from analog screen-film radiography to DR requires thorough user education because of differences in image production, processing, storage and evaluation between the forms of radiography. Without adequate education, radiologic technologists could unknowingly expose children to higher radiation doses than necessary for adequate radiograph quality.
Objective
To evaluate knowledge about image quality and dose management in pediatric DR among radiologic technologists in the U.S.
Materials and methods
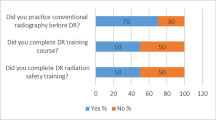
This communication describes a survey of 493 radiologic technologists who are members of the American Society of Radiologic Technologists (ASRT) and who evaluated the current state of radiological technologist education in image quality and dose management in pediatric DR. The survey included 23 survey questions regarding image acquisition issues, quality assurance, radiation exposure and education in DR of infants and children.
Results
Radiologic technologists express many needs in areas of training and education in pediatric DR. Suggested improvements include better tools for immediate feedback about image quality and exposure, more information about appropriate technique settings for pediatric patients, more user-friendly vendor manuals and educational materials, more reliable measures of radiation exposure to patients, and more regular and frequent follow-up by equipment vendors.
Conclusion
There is a clear and widespread need for comprehensive and practical education in digital image technology for radiologic technologists, especially those engaged in pediatric radiography. The creation of better educational materials and training programs, and the continuation of educational opportunities will require a broad commitment from equipment manufacturers and vendors, educational institutions, pediatric radiology specialty organizations, and individual imaging specialists.





Similar content being viewed by others
References
Applegate KE, Seibert JA (2007) Practice guideline for digital radiography. American College of Radiology
Willis CE, Slovis TL (2004) The ALARA concept in pediatric CR and DR: dose reduction in pediatric radiographic exams—a white paper conference executive summary. Pediatr Radiol 34(suppl 3):S162–S164
Fauber TL (2009) Exposure variability and image quality in computed radiography. Radiol Tech 80:209–215
Gregoire S (2006) The CASL study: dose reduction in a computed radiography environment. Radiol Tech 78:160–163
Brenner DJ, Hall EJ, Phil D (2007) Computed tomography—an increasing source of radiation exposure. New Engl J Med 357:2277–2284
Willis CE (2004) Strategies for dose reduction in ordinary radiographic examinations using CR and DR. Pediatr Radiol 34(Suppl 3):S196–S200
Author information
Authors and Affiliations
Corresponding author
Appendix 1
Appendix 1

Image acquisition
-
1.
What percentage of your work is with pediatric patients?
-
0%–25%
-
26%–50%
-
51%–75%
-
76%–100%
-
-
2.
Do you work in a dedicated children's institution?
-
Yes
-
No
-
-
3.
In what percentage of procedures do you use automatic exposure control?
-
0%–25%
-
26%–50%
-
51%–75%
-
76%–100%
-
-
4.
In what situations are grids used?
-
5.
In what percentage of procedures do you use lead markers?
-
0%–25%
-
26%–50%
-
51%–75%
-
76%–100%
-
-
6.
In what percentage of procedures do you use electronic markers?
-
0%–25%
-
26%–50%
-
51%–75%
-
76%–100%
-
Quality control workstation
-
7.
In what percentage of procedures are the electronic collimators (mask, shutter) used?
-
0%–25%
-
26%–50%
-
51%–75%
-
76%–100%
-
-
8.
In what percentage of procedures is the image adjusted at the quality-control workstation?
0%–25%
26%–50%
51%–75%
76%–100%
-
9.
Does adjusting the image at the quality-control workstation affect the exposure index?
-
Yes
-
No
-
Quality assurance
-
10.
Do you have a way to monitor your repeat rate?
-
Yes
-
No
-
-
11.
What are the common causes of repeat exposures?
-
12.
What percentage of procedures requires repeat images?
-
0%–25%
-
26%–50%
-
51%–75%
-
76%–100%
-
-
13.
Do you have a quality control technologist who checks images, or does the radiologic technologist on shift perform this function?
-
Yes, there is a quality control technologist
-
No, many technologists must perform quality control
-
Other (please specify below)
-
Please specify:
-
-
14.
Do other radiologic technologists approve exams they did not perform?
-
Yes
-
No
-
-
15.
Are there established exposure values that are acceptable?
-
Yes
-
No
-
-
16.
Is there a mechanism in place to determine the percentage of examinations that fall into the acceptable range, or that produce too much or too little exposure?
-
Yes
-
No
-
-
17.
How do radiologists' expectations affect your ability to produce high-quality, low dose Computed Radiography/Direct Radiography images?
Radiation exposure
-
18.
What do you feel contributes to or causes excess radiation exposure when performing pediatric computed radiography procedures?
-
19.
What do you feel contributes to or causes excess radiation exposure when performing pediatric direct radiography procedures?
Computed Radiography/Direct Radiography education
-
20.
What was the primary source used to provide Computed Radiography/Direct Radiography education in your institution?
-
On-the-job training
-
Equipment manufacturer
-
Off-site training
-
Other (please specify below)
-
Please specify:
-
-
21.
What educational materials would you like manufacturers to provide to those who operate the equipment?
-
22.
What educational materials would you like manufacturers or others to provide regarding radiation dose?
-
23.
What emphasis is placed on radiation dose reduction for Computed Radiography/Direct Radiography at your institution?
-
Emphasized all of the time
-
Emphasized most of the time
-
Emphasized some of the time
-
Never emphasized
-
Rights and permissions
About this article
Cite this article
Morrison, G., John, S.D., Goske, M.J. et al. Pediatric digital radiography education for radiologic technologists: current state. Pediatr Radiol 41, 602–610 (2011). https://doi.org/10.1007/s00247-010-1904-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-010-1904-3