Abstract
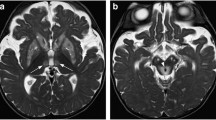
The dentate nuclei lie deep within the cerebellum and play a vital role in the pathways involved in fine motor control and coordination. They are susceptible to a variety of diseases. Some pathological processes preferentially affect the dentate nuclei, while concomitant basal ganglia or white matter involvement can be a striking finding in others. A familiarity with the normal appearance of the dentate nuclei at different ages in combination with the radiological distribution of pathology in the brain allows the paediatric radiologist to develop a logical approach to the interpretation of MR imaging of these deep cerebellar nuclei. In this article we review the normal appearance and MR features of the dentate nuclei, including changes that are seen with myelination. We describe the specific imaging characteristics of childhood diseases that involve the dentate nuclei, and develop a systematic approach to the differential diagnosis of dentate nucleus abnormalities on MR imaging.






















Similar content being viewed by others
References
Barkovich AJ (1998) MR of the normal neonatal brain: assessment of deep structures. AJNR 19:1397–1403
Kizildag B, Dusunceli E, Fitoz S et al (2005) The role of classic spin echo and FLAIR sequences for the evaluation of myelination in MR imaging. Diagn Interv Radiol 11:130–136
Valanne L, Ketonen L, Majander A et al (1998) Neuroradiologic findings in children with mitochondrial disorders. AJNR 19:369–377
Hendriksz CJ (2009) Inborn errors of metabolism for the diagnostic radiologist. Pediatr Radiol 39:211–220
Finsterer J (2008) Leigh and Leigh-like syndrome in children and adults. Pediatr Neurol 39:223–235
Lee HF, Tsai CR, Chi CS et al (2009) Leigh syndrome: clinical and neuroimaging follow-up. Pediatr Neurol 40:88–93
Rossi A, Biancheri R, Bruno C et al (2003) Leigh Syndrome with COX Deficiency and SURF-1 gene mutations: MR imaging findings. AJNR 24:1188–1191
Twomey EL, Naughten ER, Donoghue VB et al (2003) Neuroimaging findings in glutaric aciduria type 1. Pediatr Radiol 33:823–830
Oguz KK, Ozturk A, Cila A (2005) Diffusion-weighted MR imaging and MR spectroscopy in glutaric aciduria type 1. Neuroradiology 47:229–234
Takanashi J, Fujii K, Sugita K et al (1999) Neuroradiologic findings in glutaric aciduria type II. Pediatr Neurol 20:142–145
Topçu M, Erdem G, Saatçi I et al (1996) Clinical and magnetic resonance imaging features of L-2-hydroxyglutaric acidemia: report of three cases in comparison with Canavan disease. J Child Neurol 11:373–377
Kara S, Sherr EH, Barkovich AJ (2008) Dilated perivascular spaces: an informative radiologic finding in Sanfilippo syndrome type A. Pediatr Neurol 38:363–366
Aicardi J, Goutières F (1984) A progressive familial encephalopathy in infancy with calcifications of the basal ganglia and chronic cerebrospinal fluid lymphocytosis. Ann Neurol 15:49–54
Uggetti C, La Piana R, Orcesi S et al (2009) Aicardi-Goutières syndrome: neuroradiologic findings and follow-up. AJNR 30:1971–1976
Choksi V, Hoeffner E, Karaarslan E et al (2003) Infantile Refsum disease: case report. AJNR 24:2082–2084
Di Rocco M, Biancheri R, Rossi A et al (2004) MRI in acute intermittent maple syrup urine disease. Neurology 63:1078
Patay Z (2005) Diffusion-weighted MR imaging in leukodystrophies. Eur Radiol 15:2284–2303
Provenzale JM, Peddi S, Kurtzberg J et al (2009) Correlation of neurodevelopmental features and MRI findings in infantile Krabbe’s disease. AJR 192:59–65
Nagar VA, Ursekar MA, Krishnan P et al (2006) Krabbe disease: unusual MRI findings. Pediatr Radiol 36:61–64
Sener RN (2000) van der Knapp syndrome: MR imaging findings including FLAIR, diffusion imaging and proton MR spectroscopy. Eur Radiol 10:1452–1455
van der Knaap MS, Smit LM, Barth PG et al (1997) Magnetic resonance imaging in classification of congenital muscular dystrophies with brain abnormalities. Ann Neurol 42:50–59
Fulham MJ, Brooks RA, Hallett M et al (1992) Cerebellar diaschisis revisited: pontine hypometabolism and dentate sparing. Neurology 42:2267–2273
Huang BY, Castillo M (2008) Hypoxic-ischemic brain injury: imaging findings from birth to adulthood. Radiographics 28:417–439
Baker LL, Stevenson DK, Enzmann DR (1988) End-stage periventricular leucomalacia: MR evaluation. Radiology 168:809–815
Baskin HJ, Hedlund G (2007) Neuroimaging of herpes infections in children. Pediatr Radiol 37:949–963
Montenegro MA, Santos SL, Li LM et al (2002) Neuroimaging of acute cerebellitis. J Neuroimaging 12:72–74
Prayer D, Grois N, Prosch H et al (2004) MR imaging presentation of intracranial disease associated with Langerhans cell histiocytosis. AJNR 25:880–891
Martin-Duverneuil N, Idbaih A, Hoang-Xuan K et al (2006) MRI features of neurodegenerative Langerhans cell histiocytosis. Eur Radiol 16:2074–2082
Itoh T, Magnaldi S, White RM et al (1994) Neurofibromatosis type 1: the evolution of deep gray and white matter MR abnormalities. AJNR 15:1513–1519
Herron J, Darrah R, Quaghebeur G (2000) Intra-cranial manifestations of neurocutaneous syndromes. Clin Radiol 55:82–98
Jacques C, Dietemann JL (2005) Imaging features of neurofibromatosis type 1. Neuroradiology 32:180–197
Griffiths PD, Blaser S, Mukonoweshuro W et al (1999) Neurofibromatosis bright objects in children with Neurofibromatosis type 1: a proliferative potential? Pediatrics 104:e49
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McErlean, A., Abdalla, K., Donoghue, V. et al. The dentate nucleus in children: normal development and patterns of disease. Pediatr Radiol 40, 326–339 (2010). https://doi.org/10.1007/s00247-009-1504-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-009-1504-2