Abstract
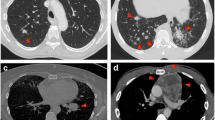
Background: A wide variety of diseases in children can present with peripheral lung lesions. Minimally invasive percutaneous techniques are preferred diagnostic tools when thoracoscopic resection is not indicated. Significant improvements in US resolution have increased the range of its applications for many diagnostic and therapeutic purposes. Objective: To determine the adequacy and safety of US-guided biopsy of peripheral pulmonary lesions in children. Materials and methods: A retrospective review was performed of the clinical, imaging and pathology records of 33 children (13 females and 20 males) in whom 38 US-guided percutaneous lung lesion biopsies had been performed between January 1996 and March 2004. Their mean age was 8.3 years (range 1–19 years, median 6.6 years). All procedures were done under general anesthesia and controlled respiration. Two techniques were used: a single-needle technique and a coaxial-needle technique. In each case, the data recorded included age, sex, lesion’s location and size, number of cores, pathology results (adequate, inadequate and indeterminate), and complications. In order to categorize the sample, the lesions were divided into four groups based on the size of the pleural surface: group 1 1–5 mm, group 2 6–10 mm, group 3 11–20 mm, and group 4 21 mm or more. Results: The mean pleural surface size of the lesions was 12 mm (range 2.3–24 mm). The coaxial-needle technique was used for 13 biopsies and the single-needle technique for 25 biopsies. Of the 38 biopsies, 32 were considered adequate (technical success 84%), 4 were truly inadequate, and 2 were indeterminate at the time of the biopsy, requiring surgical biopsy for confirmation. Minor complications occurred following 44% of the procedures, including: pain (n=5), small pneumothorax (n=4), pulmonary hematoma (n=4), atelectasis (n=4), small hemothorax (n=3), respiratory distress (n=1) and hemoptysis (n=1). No major complications occurred. No significant correlation was found between the size of the pleural surface and technical success (P=0.106) or the incidence of complications (P=0.23). Minor complications occurred following 6 out of 13 procedures using the coaxial-needle technique (16% of total) and following 11 out of 25 procedures using the single-needle technique (28% of total), with no statistically significant difference (P=0.1081). Conclusion: This small retrospective study suggests that US-guided lung biopsies are a safe and adequate method to sample peripheral pulmonary lesions in children, with a high rate of technical success and low morbidity, even for lesions with a small pleural surface (<5 mm).





Similar content being viewed by others
References
Lim GY, Newman B, Kurland G, et al (2002) Post-transplantation lymphoproliferative disorder: manifestations in pediatric thoracic organ recipients. Radiology 222:699–708
Koizumu K (2005) Thoracoscopic surgery in children. J Nippon Med Sch 72:34–42
Hayes-Jordan A, Connolly B, Temple M, et al (2003) Image-guided percutaneous approach is superior to the thoracoscopic approach in the diagnosis of pulmonary nodules in children. J Pediatr Surg 38:745–748
Yang PC (2000) Ultrasound-guided transthoracic biopsy of the chest. Radiol Clin North Am 38:323–343
Yang PC, Luh KT, Sheu JC, et al (1985) Peripheral pulmonary lesions: ultrasonography and ultrasonically guided aspiration biopsy. Radiology 155:451–456
Pang JA, Tsang V, Hom BL, et al (1987) Ultrasound-guided tissue-core biopsy of thoracic lesions with Trucut and Surecut needles. Chest 91:823–828
Koh DM, Burke S, Davies N, et al (2002) Transthoracic US of the chest: clinical uses and applications. Radiographics 22(1):e1
Chandrasekhar AJ, Reynes CJ, Churchill RJ (1976) Ultrasonically guided percutaneous biopsy of peripheral pulmonary masses. Chest 70:627–630
Sheth S, Hamper UM, Stanley DB, et al (1999) US guidance for thoracic biopsy: a valuable alternative to CT. Radiology 210:721–726
Cahill AM, Baskin KM, Kaye RD, et al (2004) CT-guided percutaneous lung biopsy in children. J Vasc Interv Radiol 15:955–960
Sailhamer E, Jackson CC, Vogel AM, et al (2003) Minimally invasive surgery for pediatric solid neoplasms. Am Surg 69:566–568
Liao WY, Chen MZ, Chang YL, et al (2000) US-guided transthoracic cutting biopsy for peripheral thoracic lesions less than 3cm in diameter. Radiology 217:685–691
Klein JS, Salomon G, Stewart EA (1996) Transthoracic needle biopsy with a coaxially placed 20-gauge automated cutting needle: results in 122 patients. Radiology 198:715–720
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fontalvo, L.F., Amaral, J.G., Temple, M. et al. Percutaneous US-guided biopsies of peripheral pulmonary lesions in children. Pediatr Radiol 36, 491–497 (2006). https://doi.org/10.1007/s00247-005-0094-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-005-0094-x