Abstract
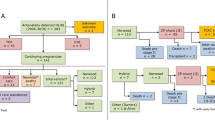
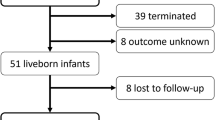
To assess the outcomes of neonates prenatally diagnosed with ventricular asymmetry and not operated on within the neonatal period and to determine the risk factors for left heart obstruction occurrence at follow-up. All neonates with prenatal asymmetry of the ventricles, diagnosed from August 1993 to July 2015, not operated on within the neonatal period, were retrospectively included in the study. Left heart echocardiographic measurements at birth and at last follow-up were collected and compared. Left heart anomaly included isthmus and/or aortic valve and/or mitral valve obstruction. There were a total of 34 newborns included in the study. The median follow-up was 2 years. There was no death. Eleven patients were operated on at a median age of three months; seven of them had an obstruction of the left heart (five coarctations of the aorta, one sub-aortic and aortic valve stenosis, and one mitral stenosis). Estimated freedom of left heart surgery was 80% at 6 months and 75% at 10 years. The main risk factor for progression to a left heart anomaly was a hypoplasia of the aortic isthmus (p = 0.0003), while the presence of a left superior vena cava was more frequent in these patients although the difference was not significant. Patients with an aortic isthmus z-score below − 2 at the closure of arterial duct are at risk of later coarctation and therefore follow-up should be extended to at least 3 months. Furthermore, the prenatal ventricular asymmetry does not only identify patients at risk of coarctation but also of other left heart anomalies. This last point should be a better approach with future parents to improve prenatal counseling on a more complex postnatal diagnostic than a simple isolated coarctation.



Similar content being viewed by others
References
Li YF, Zhou KY, Fang J, Wang C, Hua YM, Mu DZ (2016) Efficacy of prenatal diagnosis of major congenital heart disease on perinatal management and perioperative mortality: a meta-analysis. World J Pediatr 12(3):298–307
Franklin O, Burch M, Manning N, Sleeman K, Gould S, Archer N (2002) Prenatal diagnosis of coarctation of the aorta improves survival and reduces morbidity. Heart 87(1):67–69
Pettersen MD, Du W, Skeens ME, Humes RA (2008) Regression equations for calculation of z scores of cardiac structures in a large cohort of healthy infants, children, and adolescents: an echocardiographic study. J Am Soc Echocardiogr 21(8):922–934
Akita A, Harima N, Nawata S, Nakata M, Kato H (1991) Two-dimensional and Doppler echocardiographic evaluation of intrauterine blood flow dynamics in the fetuses with a ventricular septal defect. Nihon Sanka Fujinka Gakkai Zasshi 43(12):1606–1612
Johnson P, Maxwell DJ, Tynan MJ, Allan LD (2000) Intracardiac pressures in the human fetus. Heart 84(1):59–63
Moulaert AJ, Bruins CC, Oppenheimer-Dekker A (1976) Anomalies of the aortic arch and ventricular septal defects. Circulation 53(6):1011–1015
Sugiura J, Nakano T, Kado H (2016) Left ventricular outflow tract obstruction in aortic arch anomalies with ventricular septal defect. Ann Thorac Surg 101(6):2302–2308
Peng DM, Punn R, Maeda K, Selamet Tierney ES (2016) Diagnosing neonatal aortic coarctation in the setting of patent ductus arteriosus. Ann Thorac Surg 101(3):1005–1010
Morrow WR, Huhta JC, Murphy DJ Jr, McNamara DG (1986) Quantitative morphology of the aortic arch in neonatal coarctation. J Am Coll Cardiol 8(3):616–620
Ho SY, Anderson RH (1979) Coarctation, tubular hypoplasia, and the ductus arteriosus. Histological study of 35 specimens. Br Heart J 41(3):268–274
Agnoleti G, Annecchino F, Preda L, Borghi A (1999) Persistence of the left superior caval vein: can it potentiate obstructive lesions of the left ventricle? Cardiol Young 9(3):285–290
Head CE, Jowett VC, Sharland GK, Simpson JM (2005) Timing of presentation and postnatal outcome of infants suspected of having coarctation of the aorta during fetal life. Heart 91(8):1070–1074
Miranda JO, Hunter L, Tibby S, Sharland G, Miller O, Simpson JM (2017) Myocardial deformation in fetuses with coarctation of the aorta: a case-control study. Ultrasound Obstet Gynecol 49(5):623–629
IJsselhof R, Liu H, Pigula F, Gauvreau K, Mayer JE, Nido PD, et al. (2018) Rates of interventions in isolated coarctation repair in neonates versus infants: does age matter?. Ann Thorac Surg.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None
Research involving Human and Animal Participants
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Bertail-Galoin, C., Joly, H., Pangaud, N. et al. Outcomes of Newborns with Prenatal Ventricular Asymmetry not Requiring Neonatal Surgical Intervention: a 22-Year Retrospective Single-Center Study. Pediatr Cardiol 40, 276–282 (2019). https://doi.org/10.1007/s00246-018-2047-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-018-2047-9