Abstract
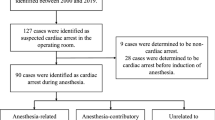
Patients with Williams syndrome are considered at high risk for anesthesia-related adverse events. At our institution, all William syndrome patients undergoing cardiac surgical, cardiac catheterization/interventional procedures, and cardiac imaging studies are cared for by cardiac anesthesiologists. All William syndrome patients undergoing non-cardiac surgical, interventional, or imaging studies are cared for by main operating room pediatric anesthesiologists with consultative input from a cardiac anesthesiologist. We reviewed our experience with 75 patients undergoing 202 separate anesthetics for 95 non-cardiac procedures and 107 cardiac procedures from 2012 to 2016. The mean age was 7.5 ± 7.0 years and the mean weight was 22.3 ± 17.0 kg. One hundred and eighty-seven patients had a general anesthetic (92.6%). Medications used included etomidate in 26.2%, propofol in 37.6%, isoflurane in 47.5%, and sevoflurane in 68.3%. Vasopressors and inotropes were required including calcium (22.8%), dopamine (10.4%), norepinephrine (17.3%), phenylephrine (35.1%), vasopressin (0.5%), and ephedrine (5.4%). The median length of stay after anesthesia was 2.8 days (range 0–32). No adverse events occurred in 89.6% of anesthetics. There were two cases of cardiac arrest, one of which required extracorporeal life support for resuscitation. Of the non-cardiac surgical procedures, 95.7% did not have a cardiovascular adverse event. Patients with Williams syndrome are at high risk for anesthesia, especially when undergoing cardiac procedures. The risk can be mitigated with appropriate planning and adherence to the hemodynamic goals for non-cardiac surgical procedures.

Similar content being viewed by others

References
Collins IIRT (2013) Cardiovascular disease in Williams Syndrome. Circulation 127:2125–2134
Adams GN (2012) SchmaierAH. The Williams-Beuren Syndrome: a window into genetic variants leading to the development of cardiovascular disease. PLoS Genet 8:e1002479
Leung DY, Glagov S, Mathews MB (1977) Elastin and collagen accumulation in rabbit ascending aorta and pulmonary trunk during postnatal growth: correlation of cellular synthetic response with medial tension. Circ Res 41:316–323
Pober BR (2010) Williams-Beuren syndrome. N Engl J Med 362:239–252
Stramm C, Li J, Ho SY, Redington AN, Anderson RH (1997) The aortic root in supravalvular aortic stenosis: the potential surgical relevance of morphologic findings. J Thorac Cardiovasc Surg 114:16–24
Stamm C, Friehs I, Ho SY, Moran AM, Jonas RA, Del Nido PJ (2001) Congenital supravalvar aortic stenosis: a simple lesion? Eur J Cardiothorac Surg 19:195–202
Burch TM, McGowan FX, Kussman BD, Powell AJ, DiNardo JA (2008) Congenital supravalvular aortic stenosis and sudden death associated with anesthesia: what the mystery? Anesth Analg 107:1848–1854
Wiwanitkit V (2010) Prevention of cardiac arrest due to anesthesia in Williams syndrome. Ann Card Anaesth 13:269
Matisoff AJ, Olivieri L, Schwartz JM, Deutsch N (2015) Risk assessment and anesthetic management of patients with Williams syndrome: a comprehensive review. Paediatr Anaesth 25:1207–1215
Hornik CP, Collins RT 2nd, Jaquiss RD, Jacobs JP, Jacobs ML, Pasquali SK, Wallace AS, Hill KD (2015) Adverse cardiac events in children with Williams syndrome undergoing cardiovascular surgery: an analysis of the Society of Thoracic Surgeons Congenital Heart Surgery Database. J Thorac Cardiovasc Surg 149:1516–1522
Latham G, Ross FJ, Eisses MJ, Richards MJ, Geiduschek JM, Joffe DC (2016) Perioperative morbidity in children with elastin arteriopathy. Pediatr Anesth 26:926–935
Olsen M, Fahy CJ, Costi DA, Kelly AJ, Burgoyne LL (2014) Anaesthesia-related haemodynamic complications in Williams syndrome patients: a review of one institution’s experience. Anaesth Intensive Care 42:619–624
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest to disclose.
Ethical Approval
All medical record review was in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later declaration or comparable ethical standards.
Informed Consent
A waiver of informed consent was granted by the institutional review board for the conduct of this study.
Rights and permissions
About this article
Cite this article
Brown, M.L., Nasr, V.G., Toohey, R. et al. Williams Syndrome and Anesthesia for Non-cardiac Surgery: High Risk Can Be Mitigated with Appropriate Planning. Pediatr Cardiol 39, 1123–1128 (2018). https://doi.org/10.1007/s00246-018-1864-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-018-1864-1