Abstract
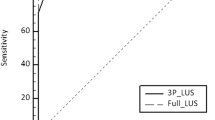
This study aimed to explore the pattern of lung ultrasound (LUS) in newborns with congenital heart disease (CHD) and to investigate the accuracy of LUS assessing pulmonary overflow (PO) during the first days of life. Lung ultrasound was performed in 51 newborns during the first days of life, and newborns were classified in two groups depending on the predisposition to develop POas evaluated by the abundance of B-lines. The results were compared to the physical examination (PE), chest X-ray, and echocardiography. In both groups there were no differences in abundance of B-lines during the first days of life, but those with a type of CHD with a trend to develop PO had a higher B-lines score after 72 h (p < 0.05) with a good correlation with echocardiography findings and with a better sensibility than PE and chest X-ray. We found that LUS is a reliable tool for the diagnosis of PO and may be useful to monitor and optimize therapy, which should be further validated in multicentre studies.

Similar content being viewed by others
References
Matthews IL, Bjørnstad PG, Kaldestad RH, Heiberg L, Thaulow E, Grønn M (2009) The impact of shunt size on lung function in infants with univentricular heart physiology. Pediatr Crit Care Med 10(1):60–65
Weintraub AS, Cadet CT, Perez R, DeLorenzo E, Holzaman IR, Stroustrup A (2013) Antibiotic use in newborns with transient tachypnea of the newborn. Neonatology 103(3):235–240
Reuter S, Moser C, Baack M (2014) Respiratory distress in the newborn. Pediatr Rev 35(10):417–428
Oba Y, Zaza T (2010) Abandoning daily routine chest radiography in the intensive care unit: meta-analysis. Radiology 255:386–395
Nakahata Y, Hiraishi S, Oowada N, Ando H, Kimura S, Furukawa S et al (2009) Quantitative assessment of pulmonary vascular resistance and reactivity in children with pulmonary hypertension due to congenital heart disease using a noninvasive method: new Doppler-derived indexes. Pediatr Cardiol 30:232–239
Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW et al (2012) International Liaison Committee on Lung Ultrasound (ILC-LUS) for International Consensus Conference on Lung Ultrasound (ICC-LUS). International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 38(4):577–591
Lichtenstein DA, Mauriat P (2012) Lung ultrasound in the critically ill neonate. Curr Pediatr Rev. 8(3):217–223
Lichtenstein DA, Meziere GA (2008) Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest 134:117–125
Peris A, Tutino L, Zagli G et al (2010) The use of point-of-care bedside lung ultrasound significantly reduces the number of radiographs and computed tomography scans in critically ill patients. Anesth Analg 111:687–692
Jambrik Z, Monti S, Coppola V, Agricola E, Mottola G, Miniati M et al (2004) Usefulness of ultrasound lung comets as a nonradiologic sign of extravascular lung water. Am J Cardiol 93(10):1265–1270
Lichtenstein D, Mézière G, Biderman P, Gepner A, Barré O (1997) The comet-tail artifact. An ultrasound sign of alveolar-interstitial syndrome. Am J Respir Crit Care Med 156(5):1640–1646
Agricola E, Bove T, Oppizzi M, Marino G, Zangrillo A, Margonato A et al (2005) “Ultrasound comet-tail images”: a marker of pulmonary edema: a comparative study with wedge pressure and extravascular lung water. Chest 127(5):1690–1695
Copetti R, Soldati G, Copetti P (2008) Chest sonography: a useful tool to differentiate acute cardiogenic pulmonary edema from acute respiratory distress syndrome. Cardiovasc Ultrasound 29(6):16
Cibinel GA, Casoli G, Elia F, Padoan M, Pivetta E, Lupia E et al (2012) Diagnostic accuracy and reproducibility of pleural and lung ultrasound in discriminating cardiogenic causes of acute dyspnea in the ermegency department. Intern Emerg Med 7:65–70
Copetti R, Cattarossi L (2007) The, “double lung point”: an ultrasound sign diagnostic of transient tachypnea of the newborn. Neonatology 91(3):203–209
Piastra M, Yousef N, Brat R, Manzoni P, Mokhtari M, De Luca D (2014) Lung ultrasound findings in meconium aspiration syndrome. Early Hum Dev 90(Suppl 2):41–43
Copetti R, Cattarossi L, Macagno F, Violino M, Furlan R (2008) Lung ultrasound in respiratory distress syndrome: a useful tool for early diagnosis. Neonatology 94(1):52–59
Martelius L, Janér C, Süvari L, Helve O, Lauerma K, Pitkänen O et al (2013) Delayed lung liquid absorption after caesarean section at term. Neonatology 104(2):133–136
Vitale V, Ricci Z, Cogo P (2014) Lung ultrasonography and pediatric cardiac surgery: first experience with a new tool for postoperative lung complications. Ann Thorac Surg 97(4):121–124
Biasucci DG, Ricci Z, Contig G, Cogo P (2014) Sonographic dynamic assessment of lung injury in a child with hypoplastic left heart syndrome undergoing extracorporeal membrane oxygenation. Pediatr Pulmonol 49(12):147–150
Teitel D (2016) Recognition of undiagnosed neonatal heart disease. Clin Perinatol 43(1):81–98
Khan AN, Hamdan A-J, Al-Ghanem S, Gouda A (2009) Reading chest radiographs in the critically ill (Part II): radiography of lung pathologies common in the ICU patient. Ann Thorac Med. 4(3):149–157
Cattarossi L (2013) Lung ultrasound: its role in neonatology and pediatrics. Early Hum Dev 89(Suppl. 1):S17–S19
Ramindo F, Migliaro F, Sodano A, Umbaldo A, Romano A, Vallone G et al (2012) Can neonatal lung ultrasound monitor fluid clearance and predict the need of respiratory support? Crit Care 16(6):R220
Helve O, Pitkanen O, Janer C, Andersson S (2009) Pulmonary fluid balance in the human newborn infant. Neonatology 95:347–352
Liu J, Wang Y, Fu W, Yang CS, Huang JJ (2014) Diagnosis of neonatal transient tachypnea and its differentiation from respiratory distress syndrome using lung ultrasound. Medicine (Baltimore) 93(27):e197
Yau KI, Fang LJ, Wu MH (1996) Lung mechanics in infants with left-to-right shunt congenital heart disease. Pediatr Pulmonol 21:42–47
Matthews IL, Kaldestad RH, Bjornstad PG, Thaulow E, Gronn M (2007) Preoperative lung function in newborn with univentricular hearts compared with healthy controls. Acta Paediatr 96:44–48
DiCarlo JV, Steven JM (1994) Respiratory failure in congenital heart disease. Pediatr Clin N Am 41:525–542
Pringitore A, Garbella E, Pi Piaggi, Menicucci D, Frassi F, Lionetti V et al (2011) Early subclinical increase in pulmonary water content in athletes performing sustained heavy exercise at sea level: ultrasound lung comet-tail evidence. Am J Physiol Heart Circ Physiol 301(5):161–167
Gargani L, Frassi F, Soldati G, Tesorio P, Georghiade M, Picano E (2008) Ultrasound lung comets for the differential diagnosis of acute cardiogenic dyspnea: a comparison with natriuretic peptides. Eur J Heart Fail 10:70–77
Strnad M, Prosen G, Borovnik V (2016) Bedside lung ultrasound for monitoring the effectiveness of prehospital treatment with continuous for positive airway pressure in acute decompensated hear failure. Eur J Emerg Med. 23:50–55
Agricola E, Bove T, Oppizzi M, Marino G, Zangrillo A, Margonato A et al (2005) Ultrasound comet-tail images: a marker of pulmonary edema: a comparative study with wedge pressure and extravascular lung water. Chest 127:1690–1695
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rodríguez-Fanjul, J., Llop, A.S., Balaguer, M. et al. Usefulness of Lung Ultrasound in Neonatal Congenital Heart Disease (LUSNEHDI): Lung Ultrasound to Assess Pulmonary Overflow in Neonatal Congenital Heart Disease. Pediatr Cardiol 37, 1482–1487 (2016). https://doi.org/10.1007/s00246-016-1461-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-016-1461-0