Abstract
Purpose
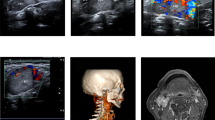
The Shamblin classification is the commonest method to predict complications and outcomes during carotid body tumor (CBT) resection. The aim of this study is to describe the utility of the three-dimensional volumetric reconstruction (3DVR) analysis of the CBT and its relationship with postoperative outcomes.
Methods
Preoperative computed tomography angiography (CTA) was obtained to perform 3DVR of the CBT. Imaging data were analyzed and correlated with surgical outcomes: estimated blood loss (EBL), surgical time (ST), and hospital length of stay (HLOS). The Pearson test was used to determine the correlation between volume and postoperative outcomes.
Results
Fifty-seven patients were studied, 13 had Shamblin type I tumors with a mean 3DVR of 7.69 cm3 (standard deviation [SD 8.27]), 21 were type II with a mean 3DVR of 15.57 cm3 (SD 8.40), and 23 were type III with a mean 3DVR of 30.58 cm3 (SD 20.16). EBL mean was 559 milliliters (mL) (standard error [SE] 80.44), the mean ST of resection was 202 min (SD 67), and the mean HLOS was 5.8 days (SD 3.23). The Pearson test showed a correlation of r = 0.69 (p < 0.0001) between 3DVR and EBL, a r = 0.4 (p = 0.05) was obtained between 3DVR and ST, and finally, a r = 0.3 (p = 0.05) between 3DVR and HLOS was obtained.
Conclusion
The preoperative 3DVR determination of CBTs allows to analyze possible predictors of surgical outcomes. We found a positive correlation between the 3DVR volume and EBL. Further research is necessary to validate this method in the evaluation of these rare neoplasms.


Similar content being viewed by others
References
Hinojosa CA, Ortiz-Lopez LJ, Anaya-Ayala JE, Orozco-Sevilla V, Nunez-Salgado AE (2015) Comparison of retrocarotid and caudocranial dissection techniques for the surgical treatment of carotid body tumors. J Vasc Surg 62:958–964
Wang ZY, Bisgard GE (2002) Chronic hypoxia-induced morphological and neurochemical changes in the carotid body. Microsc Res Tech 59:168–177
Rodriguez-Cuevas S, Lopez-Garza J, Labastida-Almendaro S (1998) Carotid body tumors in inhabitants of altitudes higher than 2000 meters above sea level. Head Neck 20:374–378
Davila VJ, Chang JM, Stone WM, Fowl RJ, Bower TC, Hinni ML, Money SR (2016) Current surgical management of carotid body tumors. J Vasc Surg 64:1703–1710
Jech M, Alvarado-Cabrero I, Albores-Saavedra J, Dahia PL, Tischler AS (2006) Genetic analysis of high altitude paragangliomas. Endocr Pathol 17:201–202
Hinojosa CA, Anaya-Ayala JE, Laparra-Escareno H, Torres-Machorro A, Lizola R, Gamboa-Dominguez A (2017) Concomitant surgical treatment of symptomatic carotid artery disease with a coexisting Shamblin I carotid body tumor. Vasc Endovasc Surg 51:103–107
Schulz SA, Wohler A, Beutner D, Angelov DN (2016) Microsurgical anatomy of the human carotid body (glomus caroticum): features of its detailed topography, syntopy and morphology. Ann Anat 204:106–113
Hinojosa CA, Anaya-Ayala JE, Olivares-Cruz S, Laparra-Escareno H, Trolle-Silva A, Angeles-Angeles H (2018) Malignant Shamblin III carotid body tumors resected with use of the retrocarotid dissection technique in 2 patients. Tex Heart Inst J 45:92–95
Metheetrairut C, Chotikavanich C, Keskool P, Suphaphongs N (2016) Carotid body tumor: a 25-year experience. Eur Arch Otorhinolaryngol 273:2171–2179
Fokkema M, de Borst GJ, Nolan BW, Indes J, Buck DB, Lo RC, Moll FL, Schermerhorn ML (2014) Clinical relevance of cranial nerve injury following carotid endarterectomy. Eur J Vasc Endovasc Surg 47:2–7
Shamblin WR, ReMine WH, Sheps SG, Harrison EG Jr (1971) Carotid body tumor (chemodectoma). Clinicopathologic analysis of ninety cases. Am J Surg 122:732–739
Luna-Ortiz K, Rascon-Ortiz M, Villavicencio-Valencia V, Herrera-Gomez A (2006) Does Shamblin’s classification predict postoperative morbidity in carotid body tumors? A proposal to modify Shamblin’s classification. Eur Arch Otorhinolaryngol 263:171–175
Michalowska I, Lewczuk A, Cwikla J, Prejbisz A, Swoboda-Rydz U, Furmanek M et al (2016) Evaluation of head and neck paragangliomas by computed tomography in patients with pheochromocytoma-paraganglioma syndromes. Pol J Radiol 81:510–518
Jin ZQ, He W, Wu DF, Lin MY, Jiang HT (2016) Color doppler ultrasound in diagnosis and assessment of carotid body tumors: comparison with computed tomography angiography. Ultrasound Med Biol 42:2106–2113
Law Y, Chan YC, Cheng SW (2017) Surgical management of carotid body tumor. Is Shamblin classification sufficient to predict surgical outcome? Vascular 25:184–189
Straughan DM, Neychev VK, Sadowski SM, Ellis RJ, Thomas F, Patronas NJ, Pacak K, Kebebew E, Nilubol N (2015) Preoperative imaging features are associated with surgical complications following carotid body tumor resection. World J Surg 39:2084–2089
Kim GY, Lawrence PF, Moridzadeh RS, Zimmerman K, Munoz A, Luna-Ortiz K, Oderich GS, de Francisco J, Ospina J, Huertas S, de Souza LR, Bower TC, Farley S, Gelabert HA, Kret MR, Harris EJ Jr, de Caridi G, Spinelli F, Smeds MR, Liapis CD, Kakisis J, Papapetrou AP, Debus ES, Behrendt CA, Kleinspehn E, Horton JD, Mussa FF, Cheng SWK, Morasch MD, Rasheed K, Bennett ME, Bismuth J, Lumsden AB, Abularrage CJ, Farber A (2017) New predictors of complications in carotid body tumor resection. J Vasc Surg 65:1673–1679
Lambin P, Rios-Velazquez E, Leijenaar R, Carvalho S, van Stiphout RG, Granton P et al (2012) Radiomics: extracting more information from medical images using advanced feature analysis. Eur J Cancer 48:441–446
Heesterman BL, de Pont LMH, Verbist BM, van der Mey AGL, Corssmit EPM, Hes FJ et al (2017) Age and tumor volume predict growth of carotid and vagal body paragangliomas. J Neurol Surg B Skull Base 78:497–505
Heesterman BL, Verbist BM, van der Mey AG, Bayley JP, Corssmit EP, Hes FJ, Jansen JC (2016) Measurement of head and neck paragangliomas: is volumetric analysis worth the effort? A method comparison study. Clin Otolaryngol 41:571–578
Weathley JM, Rosenfield NS, Heller G, Feldstein D, Michael P, Laquaglia MP (1994) Validation of a technique of computer-aided tumor volume determination. J Surg Res 59(6):621–626
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Informed consent
For this type of retrospective study formal consent is not required; all study data was anonymized and is not traceable to the patient.
Rights and permissions
About this article
Cite this article
Lozano-Corona, R., Anaya-Ayala, J.E., Martínez-Martínez, R. et al. Usefulness of preoperative three-dimensional volumetric analysis of carotid body tumors. Neuroradiology 60, 1281–1286 (2018). https://doi.org/10.1007/s00234-018-2095-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-018-2095-0