Abstract
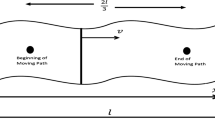
This paper presents an hyperbolic Pennes bioheat equation in cylindrical coordinate for modeling the Microwave Ablation (MWA) applied in prostate cancer. Due to recent reports, the number of patients of prostate cancer is growing by 15 million in the world each year. Since, it is shown that application of uniform microwave in prostate area of different patients may produce different temperature, the Pennes bioheat equation is considered to study the effect of perfusion term on produced temperature profiles. The solution method is Eigen value method which results in a closed form solution. The hyperbolic behavior of temperature profiles under high heat release against Fourier model is shown. Results show the importance of tissue perfusion term in estimation of temperature profiles and establish that the thermal tissue damage is expected to initiate from 1 to 3 mm above the catheter surface and to promote up to 7 mm. The solutions can be applied as a verification branch for other numerical works and can be very useful to reduce uncertainty about MWA treatments and improve the reliability of clinical protocols giving insight to the Surgeons.











Similar content being viewed by others
Abbreviations
- n :
-
Series counter
- t :
-
Time (s)
- r :
-
Cylindrical coordinate (mm)
- z :
-
Cylindrical coordinate (mm)
- r i :
-
Radius of catheter (mm)
- r o :
-
Outer radius of biological tissue (mm)
- H :
-
Height of affected area (mm)
- A t :
-
Constant of proportionality
- Q :
-
volumetric rate of heating (Wm−3)
- P :
-
experimental power function
- P r :
-
Reference power (J)
- T :
-
Temperature (°C )
- T b :
-
Blood temperature (°C )
- T m :
-
Reference temperatures (°C )
- T 0 :
-
Initial temperatures (°C )
- c t :
-
Tissue specific heat (JKg−1 ° C−1)
- c b :
-
Blood specific heat (JKg−1 ° C−1)
- h :
-
Convection coefficient (Wm−2 ° C−1)
- w :
-
Heat propagation speed (ms−1)
- η :
-
Dimensionless coordinate
- ζ :
-
Dimensionless coordinate
- ρ t :
-
Tissue density (Kgm−3)
- α t :
-
Thermal diffusivity (m2s−1)
- κ t :
-
Thermal conductivity (Wm−1 ° C−1)
- ρ b :
-
Blood density (Kgm−3)
- τ q :
-
Thermal relaxation time (s)
- ω b :
-
Blood perfusion rate (s−1)
- β :
-
Microwaves rate of absorption (m−1)
- θ :
-
Dimensionless temperature
- τ :
-
Dimensionless time
- γ :
-
Dimensionless constant
- ψ :
-
Dimensionless heat source
- ψ 0 :
-
Dimensionless constant
References
Kundu B (2016) Exact analysis for propagation of heat in a biological tissue subject to different surface conditions for therapeutic applications. Appl Math Comput 285:204–216
Talaee MR, Kabiri A (2017) Analytical solution of hyperbolic bioheat equation in spherical coordinates applied in radiofrequency heating. J Mech Med Biol 17(04):1750072
Deshazer G, Prakash P, Merck D, Haemmerich D (2017) Experimental measurement of microwave ablation heating pattern and comparison to computer simulations. Int J Hyperth 33(1):74–82
Lin SM, Li CY (2017) Semi-analytical solution of bioheat conduction for multi-layers skin subjected to laser heating and fluid cooling. J Mech Med Biol 17(02):1750029
Ghosh S, Gupta DD, Chakraborty S, Das SK (2013) Superparamagnetic nanoparticle assisted hyperthermia and cooling protocol for optimum damage of internal carcinoma using computational predictive model. Heat Mass Transf 49(9):1217–1229
Lv Y, Zou Y, Yang L (2012) Theoretical model for thermal protection by microencapsulated phase change micro/nanoparticles during hyperthermia. Heat Mass Transf 48(4):573–584
Ramadhyani S, Abraham JP, Sparrow EM (2009) A mathematical model to predict tissue temperatures and necrosis during microwave thermal ablation of the prostate. Adv Num Heat Trans 3:345–371
Abraham JP, Sparrow EM, Ramadhyani S (2007) Numerical simulation of a BPH thermal therapy—a case study involving TUMT. J Biomech Eng 129(4):548–557
Lopresto V, Pinto R, Farina L, Cavagnaro M (2017) Microwave thermal ablation: effects of tissue properties variations on predictive models for treatment planning. Med Eng Phys 46:63–70
Liu D, Brace CL (2017) Numerical simulation of microwave ablation incorporating tissue contraction based on thermal dose. Phys Med Biol 62(6):2070
Anvari B, Rastegar S, Motamedi M (1994) Modeling of intraluminal heating of biological tissue: implications for treatment of benign prostatic hyperplasia. IEEE Trans Biomed Eng 41(9):854–864
He X, McGee S, Coad JE, Schmidlin F, Iaizzo PA, Swanlund DJ et al (2004) Investigation of the thermal and tissue injury behavior in microwave thermal therapy using a porcine kidney model. Int J Hyperth 20(6):567–593
Loyd D, Karlsson M, Erlandsson BE, Sjödin JG, Ask P (1997) Computer analysis of hyperthermia treatment of the prostate. Adv Eng Softw 28(6):347–351
Bernardi P, Cavagnaro M, Lin JC, Pisa S, Piuzzi E (2004) Distribution of SAR and temperature elevation induced in a phantom by a microwave cardiac ablation catheter. IEEE Trans Micro Theory Techniq 52(8):1978–1986
Navarro MC, Burgos J (2017) A spectral method for numerical modeling of radial microwave heating in cylindrical samples with temperature dependent dielectric properties. Appl Math Model 43:268–278
Schramm W, Yang D, Haemmerich D (2006). Contribution of direct heating, thermal conduction and perfusion during radiofrequency and microwave ablation. In Engineering in Medicine and Biology Society, 2006. EMBS'06. 28th Annual International Conference of the IEEE (pp. 5013–5016). IEEE
Wren J (2004) Microwave thermotherapy of prostatic enlargement-analysis of radiometric thermometry using a hybrid bio-heat equation. Comput Methods Biomech Biomed Eng 7(3):177–185
Wu X, Liu B, Xu B (2016) Theoretical evaluation of high frequency microwave ablation applied in cancer therapy. Appl Therm Eng 107:501–507
Wang T, Zhao G, Qiu B (2015) Theoretical evaluation of the treatment effectiveness of a novel coaxial multi-slot antenna for conformal microwave ablation of tumors. Int J Heat Mass Transf 90:81–91
Chaichanyut, M., & Tungjitkusolmun, S. (2016). Microwave Ablation Using Four-Tine Antenna: Effects of Blood Flow Velocity, Vessel Location, and Total Displacement on Porous Hepatic Cancer Tissue. Computational and Mathematical Methods in Medicine, 2016
Gao H, Wu S, Wang X, Hu R, Zhou Z, Sun X (2017) Temperature simulation of microwave ablation based on improved specific absorption rate method compared to phantom measurements. Comput Assis Surg 22(sup1):9–17
Tung MM, Trujillo M, Molina JL, Rivera MJ, Berjano EJ (2009) Modeling the heating of biological tissue based on the hyperbolic heat transfer equation. Math Comput Model 50(5–6):665–672
Lee HL, Lai TH, Chen WL, Yang YC (2013) An inverse hyperbolic heat conduction problem in estimating surface heat flux of a living skin tissue. Appl Math Model 37(5):2630–2643
Molina JAL, Rivera MJ, Berjano E (2014) Fourier, hyperbolic and relativistic heat transfer equations: a comparative analytical study. Proc R Soc A 470(2172):20140547
Ezzat MA, AlSowayan NS, Al-Muhiameed ZI, Ezzat SM (2014) Fractional modelling of Pennes’ bioheat transfer equation. Heat Mass Transf 50(7):907–914
Kumar D, Singh S, Rai KN (2016) Analysis of classical Fourier, SPL and DPL heat transfer model in biological tissues in presence of metabolic and external heat source. Heat Mass Transf 52(6):1089–1107
Kumar A, Kumar S, Katiyar VK, Telles S (2017) Phase change heat transfer during cryosurgery of lung cancer using hyperbolic heat conduction model. Comput Biol Med 84:20–29
Atefi G, Talaee MR (2011) Non-fourier temperature field in a solid homogeneous finite hollow cylinder. Arch Appl Mech 81(5):569–583
Talaee MR, Atefi G (2011) Non-Fourier heat conduction in a finite hollow cylinder with periodic surface heat flux. Arch Appl Mech 81(12):1793–1806
Talaee MR, Kabiri A, Khodarahmi R (2018) Analytical solution of hyperbolic heat conduction equation in a finite medium under pulsatile heat source. Iran J Sci Technol, Trans Mech Eng 42(3):269–277
Talaee MR, Kabiri A (2017) Exact analytical solution of bioheat equation subjected to intensive moving heat source. J Mech Med Biol 17(05):1750081
Talaee M, Alizadeh M, Bakhshandeh S (2014) An exact analytical solution of non-Fourier thermal stress in cylindrical shell under periodic boundary condition. Eng Solid Mech 2(4):293–302
Asmar NH (2016) Partial differential equations with Fourier series and boundary value problems. Courier Dover Publications
Henriques FC Jr, Moritz AR (1947) Studies of thermal injury: I. The conduction of heat to and through skin and the temperatures attained therein. A theoretical and an experimental investigation. Am J Pathol 23(4):530
Bhowmick P, Coad JE, Bhowmick S, Pryor JL, Larson T, De La Rosette J, Bischof JC (2004) In vitro assessment of the efficacy of thermal therapy in human benign prostatic hyperplasia. Int J Hyperth 20(4):421–439
Van de Sompel D, Kong TY, Ventikos Y (2009) Modelling of experimentally created partial-thickness human skin burns and subsequent therapeutic cooling: a new measure for cooling effectiveness. Med Eng Phys 31(6):624–631
Ahmadikia H, Moradi A, Fazlali R, Parsa AB (2012) Analytical solution of non-Fourier and Fourier bioheat transfer analysis during laser irradiation of skin tissue. J Mech Sci Technol 26(6):1937–1947
Mitra K, Kumar S, Vedevarz A, Moallemi MK (1995) Experimental evidence of hyperbolic heat conduction in processed meat. J Heat Transf 117(3):568–573
Wootton JH, Ross AB, Diederich CJ (2007) Prostate thermal therapy with high intensity transurethral ultrasound: the impact of pelvic bone heating on treatment delivery. Int J Hyperth 23(8):609–622
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of intrest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kabiri, A., Talaee, M.R. Theoretical investigation of thermal wave model of microwave ablation applied in prostate Cancer therapy. Heat Mass Transfer 55, 2199–2208 (2019). https://doi.org/10.1007/s00231-019-02562-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00231-019-02562-9