Abstract
Objective
To investigate the influence of adherence to psychotropic medications upon the risk of completed suicide by comparing person-level prescriptions and postmortem toxicological findings among complete-suicide cases and non-suicide controls in Sweden 2006–2013.
Methods
Using national registries with full coverage on dispensed prescriptions, results of medico-legal autopsies, causes of death, and diagnoses from inpatient care, estimated continuous drug use for 30 commonly prescribed psychotropic medications was compared with forensic-toxicological findings. Subjects who had died by suicide (cases) were matched (1:2) with subjects who had died of other causes (controls) for age, sex, and year of death. Odds ratios were calculated using logistic regression to estimate the risk of completed suicide conferred by partial adherence and non-adherence to pharmacotherapy. Adjustments were made for previous inpatient care and the ratio of initiated and discontinued dispensed prescriptions, a measure of the continued need of treatment preceding death.
Results
In 5294 suicide cases and 9879 non-suicide controls, after adjusting for the dispensation ratio and other covariates, partial adherence and non-adherence to antipsychotics were associated with 6.7-fold and 12.4-fold risks of completed suicide, respectively, whereas corresponding risk estimates for antidepressant treatment were not statistically significant and corresponding risk increases for incomplete adherence to antidepressant treatment were lower (1.6-fold and 1.5-fold, respectively) and lacked statistical significance.
Conclusion
After adjustment for the need of treatment, biochemically verified incomplete adherence to antipsychotic pharmacotherapy was associated with markedly increased risks of completed suicide.
Similar content being viewed by others
Introduction
Associations between the use of psychotropic medications and the risk of suicidality are a topic of recurrent discussion. Whereas antipsychotic agents—particularly clozapine and the mood-stabilizer lithium—seem to have protective effects on both non-lethal suicidality and completed acts of suicide in schizophrenia and affective disorders [1,2,3,4], concerns have been raised regarding antidepressants [5,6,7,8,9]. Indeed, despite numerous large, population-based studies investigating possible antisuicidal or prosuicidal properties of antidepressants, results regarding their overall effect on suicide risk remain inconclusive [10,11,12,13].
In the few studies that have demonstrated protective effects for psychotropic agents on the suicide risk, the effects appear to be more specifically associated with continuous medication use [3, 14,15,16,17,18]. Although poor adherence to, discontinuation of, and switches between psychotropic medications have been identified as reproducible risk factors for suicide, early discontinuation of antidepressant treatment has been reported to decrease suicide risk in the elderly [19, 20]. Further, in two studies matching for suicidal propensity in Canada and Sweden, initiation of selective-serotonin-reuptake-inhibitor therapy increased the risk of violent suicide during the first month of treatment [21, 22].
In a few studies of completed suicide, adherence to psychotropic medications has been confirmed by biochemical methods, but never in comparison to adherence in non-suicide controls [23,24,25]. Further, even in registry-based studies including controls, discrepancies exist regarding how continuous medication use has been operationalized vis-à-vis the timing of prescription dispensation [26, 27]. Also, whereas non-biochemical registry-based studies rely on the assumption that single or consecutive medication purchases reflect genuine intake, toxicological analyses can verify medication use in relation to therapeutic concentrations.
Apart from published reports using Swedish registry data to assess adherence to non-addictive medications in the general population [28]; to psychotropic medications in homicide offenders and victims [29]; and to antidepressants among young suicide victims [30], no previous study has exploited discrepancies between person-level prescription and toxicology data derived from nationwide registries to investigate biochemically verified pharmacoadherence.
Aims of the study
In this population-based forensic-toxicological study with a matched case-control design, our primary objective was to investigate biochemically verified adherence to treatment with psychotropic medications in all instances of completed suicide (by means other than self-poisoning; cases) and instances of non-suicide deaths (controls) occurring in Sweden 2006–2013. A second objective was to investigate a novel measure of the continued need for treatment based on the ratio of initiated and discontinue prescriptions. Based upon previous research implying that pharmacoadherence to psychotropic agents reduces suicide risk, we hypothesized that toxicologically verifiable incomplete adherence to antidepressant and antipsychotic medications would be associated with increased risks of completed suicide.
Material and methods
Setting
During forensic autopsies—conducted by the National Board of Forensic Medicine (NBFM) to clarify the cause of death in instances of suspected unnatural death—blood samples are routinely collected for toxicological analyses performed using a test panel capable of detecting the most common legal and illegal pharmacologically active substances and their metabolites [31]. Results of toxicological analyses and causes of death are registered, respectively, in the NBFM database Toxbase and the National Board of Health and Welfare’s (NBHW) Cause of Death Registry. NBHW’s Prescription Registry contains complete individual-level information for all dispensed prescriptions since July 1, 2005, while its National Patient Registry contains individual-level information for all instances of inpatient care since 1987. For this study, we linked complete records, retrieved from Toxbase, for all forensically investigated deaths in Sweden during the period January 1, 2006, to December 31, 2013, to NBHW’s prescription and patient registries. For further comparisons between study subjects and the Swedish general population, official annual statistics were retrieved from publicly available statistical databases at Statistics Sweden and NBHW.
Subjects
From 34,513 forensic autopsies, complete records regarding age, sex, date and cause of death, postmortem toxicological findings, and prescription history were available for 23,684 subjects, after exclusion of 2394 subjects for whom information on date of death or sex was unavailable; 4982 subjects who had died in an ambulance or at hospital, been admitted to a hospital in the 3 days preceding death, or spent more than 30 days cumulatively on a hospital ward during the 183 days preceding death (to remove instances of non-registered pharmacological treatment from ambulance or hospital care); and 3453 subjects who had died from self-poisoning of intentional or undetermined intent (ICD-9 codes E966-E969; and ICD-10 codes X60-X69 and Y10-Y19; to minimize the possibility of false-positive pharmacoadherence; Fig. 1). Approximate 1:2 matching was performed for age, sex, and year of death, rendering 5294 completed-suicide cases and 9879 non-suicide controls. Prevalence of comorbid conditions from previous inpatient care was operationalized as one possible main diagnosis per person and year. The study was approved by the Regional Ethical Review Board in Stockholm (2013/1411-31/5).
Analyses
Virtually all deaths investigated by NBFM undergo initial screening for nearly 200 substances by the use of liquid-chromatography time-of-flight technology. Upon positive finding, substances’ concentrations are then quantified by gas chromatography–mass spectrometry or liquid-chromatography–tandem mass spectrometry and recorded in Toxbase [32]. The methods have been accredited with validated detection thresholds for analyzed substances.
Exposure
All psychotropic medications whose active substances or metabolites NBFM routinely screens for were included, with the exception of addictive substances readily acquired illegally (benzodiazepines and stimulants). To minimize the risk of underestimation of adherence—which, in the presence of differences in treatment regimens between cases and controls, could give rise to spurious associations—included substances were required to have half-lives longer than 5 h and to be detectable at concentrations near the lower limit of the recognized therapeutic range (Supplementary table 3) [33]. Possible variations in substances’ postmortem blood dilution were accounted for as in previous studies [34,35,36,37]. Altogether, data on 30 psychotropic medications were modeled and compared with corresponding forensic-toxicological findings. All medications were categorized according to the Anatomical Therapeutic Chemical classification system and, in accordance with intended indications in a psychiatric setting, defined as antidepressants (N06A) or antipsychotics (N05A, excluding lithium).
PRE2DUP
Expected medication-use periods were modeled using the Prescription Registry by PRE2DUP, as previously described [26, 28]. The method is based on sliding averages of daily defined doses (DDD) calculated for each medication over time, taking personal medication-purchasing behavior and medication stockpiling into account; in the case of single purchases, the expected duration of the purchased package was used [38]. In this study, the last purchase was the primary evaluated factor when medication use at the time of death was assessed; dates of death were not known to PRE2DUP modelers (HT, AT). A prescription history of at least 365 days before death was available for all included subjects, except for subjects who had died before July 1, 2006.
Statistics
Based on modeled medication data, total purchased DDDs, total number of changes (initiations and discontinuations) of dispensed prescriptions, and dispensation ratio (the number of initiations divided by the number of discontinuations) with 95% confidence intervals (CIs) were calculated for the year preceding death (or the 183 days preceding death for subjects who had died before July 1, 2006) for: psychotropic medications whose active substances or metabolites met toxicological inclusion criteria; all dispensed psychotropic medications; and all dispensed medications. Above calculations were also performed separately for antidepressants and antipsychotics. Dispensation ratios equal or exceeding 1.0 were interpreted as representing ongoing monotherapy or increasing polypharmacy and thus conceptualized as a measure of continued need of treatment.
Assessment of agreement between PRE2DUP-modeled medication use and toxicological findings as a measure of biochemically verified pharmacoadherence was made at an individual level for all toxicologically investigated psychotropic medications. Risks of completed suicide conferred by adherent, partially adherent or non-adherent use of each class of psychotropic medication, were estimated using logistic regression by comparing exposure to treatment in cases and controls expressed as odds ratios (ORs) with 95% CIs. ORs for which uncorrected 95% CIs did not span unity were considered statistically significant.
Criteria of judgment
Adherence was defined as congruence between the predicted occurrence of continuous medication use at the time of death and positive postmortem toxicology for the same medication’s active substance or metabolite, without simultaneous incongruence for a medication in the same class. Non-adherence was defined as predicted occurrence of continuous medication use at the time of death in the absence of positive postmortem toxicology for all medications in a particular class, and partial adherence as simultaneous congruence and incongruence for multiple medications in the same class.
Adjustments were made for sex, age, previous inpatient care, and previous psychiatric inpatient care (both defined as at least one instance of inpatient care recorded in the National Patient Registry), as well as the dispensation ratio during the 4 months preceding death. Statistical analyses were performed using R version 3.4 .4 (R Core Team, Vienna, Austria) and SPSS version 22.0 (IBM Corp., Armonk, NY, USA).
Ethics
Our investigation was carried out in accordance with the latest version of the Declaration of Helsinki. The research ethics committee in Stockholm, Sweden, approved the current research (reference number 2013/1411-31/5).
Data availability
The data that support the findings of this study are available from the two Swedish governmental agencies: the Swedish National Board of Forensic Medicine’s department of forensic toxicology (Rättsmedicinalverket - Rättskemi; Toxbase; http://www.rmv.se); and the National Board of Health and Welfare (Socialstyrelsen; Prescription Registry and Cause of Death Registry; http://www.sos.se), but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission from Rättsmedicinalverket and Socialstyrelsen.
Results
Characteristics of sample
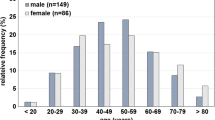
As seen in Table 1, of 5294 completed-suicide cases, 80% were male and 73% under 65 years of age (mean age 52 years, SD 19.9 years), whereas, of 9879 non-suicide controls, 82% were male and 72% under 65 years of age (mean age 53 years, SD 19.1). In comparison, for the study period, the living Swedish population consisted of nearly equal distribution of men and women, with a mean age of 41 years, with 82% under 65 years of age. After exclusion of self-poisoning, the two most common main causes of death among controls were death due to external causes (ICD-10 codes V01-Y98, with the exception of Y10-Y19), at 39%, and death resulting from diseases of the circulatory system (ICD-10 codes I00-I99), at 37%. In the Swedish population, for the study period, main causes of death were death resulting from diseases of the circulatory system, at 40%, and neoplasms (ICD-10 codes C00-D48), at 25%, whereas the average annual proportion of individuals dying from external causes was 5%. The contribution of each of the 8 years of the study period to the total number of cases and controls was relatively constant.
Rates of positivity for ethanol and GABAergic hypnotics upon toxicological analysis were, after rounding, equal in completed-suicide cases and non-suicide controls, at 26% and 18%, respectively, whereas opioids and other addictive medications were less commonly detected in cases than in controls (3% vs. 8%, and 3% vs. 6%, respectively). Alcohol-related disorders and ischemic heart disease were the two most common comorbid conditions adjudged to have contributed to the cause of death in both cases (at 7% and 2%, respectively) and controls (at 20% and 31%, respectively). Comorbid conditions contributing to the main causes of death were not available for the general population. Among completed-suicide cases, depression (10.6%), alcohol-related disorders (10.6%), and psychosis (4.8%) were the most common main diagnoses from previous inpatient care, whereas in non-suicide controls, alcohol-related disorders (23.8%), drug-related disorders (7.6%), and diabetes mellitus (3.1%) were the leading main diagnoses. For all main diagnoses other than pulmonary or cardiovascular conditions, the general population showed a lower prevalence of previous inpatient care compared with the study group (Table 1).
Dispensation ratios
The number of changes in dispensed prescriptions per person, the dispensation ratio per month, and DDD per person were modeled for the year preceding death in cases and controls for all medications, all psychotropic medications, and all toxicologically verifiable psychotropic medications. Among cases, the monthly number of changes per person increased over the year preceding death (all medications 0.56–1.10; all psychotropic medications 0.18–0.48; and verifiable psychotropic medications 0.05–0.15), while non-suicide controls showed similar trends (all medications 1.03–1.49; all psychotropic medications, 0.27–0.39; and verifiable psychotropic medications 0.05–0.08). Increases were more dependent on initiated prescriptions in cases than in controls, as shown by differences between groups regarding dispensation ratios. Calculated linear fitting for the 6 months preceding death showed statistically significant slopes of similar magnitude for changes in dispensation ratios, but in opposite directions, between completed-suicide cases (positive slope) and non-suicide controls (negative slope), for all psychotropic medications and toxicologically verifiable psychotropic medications. By the last month prior to death, cases had surpassed controls with regard to dispensed DDDs per person per month for all psychotropic medications and verifiable psychotropic medications (Supplementary table 4).
In completed-suicide cases, the dispensation ratio decreased for all medications (1.15–0.96) yet increased for all psychotropic medications (1.17–1.42) and verifiable psychotropic medications (1.30–1.76), in the year preceding death, whereas ratios in non-suicide controls decreased for all types of prescriptions (all medications, 1.15–0.66; all psychotropic medications, 1.11–0.67; and verifiable psychotropic medications, 1.29–0.59). By 2 months prior to death, 95% CIs for dispensation ratios of cases and controls no longer overlapped for any prescription type (Supplementary table 4, Fig. 2).
Differences in dispensation ratios for verifiable psychotropic substances were further modeled with a focus on antidepressants and antipsychotics. The ratio in completed-suicide cases prescribed antidepressants increased in the months prior to death, diverging, at 2 months prior to death, from ratios in other groups; by the last month prior to death, the 95% CI for the ratio in cases no longer overlapped with intervals for ratios in other groups (Supplementary figure 1, Supplementary table 5).
Adherence and suicide risk
In models comparing risk estimates for completed suicide conferred by degrees of adherence to antipsychotics and antidepressants, adherence was set as reference (OR 1; Table 2). Unadjusted risk estimates for non-adherence and partial adherence to antipsychotics were OR 9.51 (95% CI 2.70–60.30) and OR 4.59 (95% CI 1.30–29.16), respectively. Following adjustments for psychiatric and somatic inpatient care, non-adherence and partial adherence conferred, respectively, the highest and next highest risk estimates (adjusted OR [aOR] 9.92, 95% CI 2.80–63.14 and aOR 4.72, 95% CI 1.33–30.10). After further adjustment for dispensation ratio, risk estimates increased further for both non-adherence (aOR 12.43, 95% CI 2.06–238.66) and partial adherence (aOR 6.66, 95% CI 1.20–128.04). For antidepressants, unadjusted risk estimates for non-adherence and partial adherence were OR 1.61 (95% CI 1.05–2.50) and OR 1.57 (95% CI 1.04–2.40), respectively. Adjustments for previous psychiatric and somatic inpatient care yielded attenuated risk estimates for suicide, with the risked conferred non-adherence being statistically significant (partial adherence, aOR 1.43, 95% CI 0.94–2.20; non-adherence, aOR 1.59, 95% CI 1.03–2.49); however, after a final adjustment for dispensation ratio, the latter risk estimate was no longer significant (aOR 1.52, 95% CI 0.67–3.44). Analyses of possible interactions between sex and adherence status revealed no significant effects for any combination (data not shown).
Discussion
This nationwide postmortem study included information regarding nearly all incidents of suspected unnatural death in Sweden 2006–2013. Using a matched case-control design, we investigated whether biochemically verified incomplete adherence to commonly prescribed psychotropic medications influences the risk of completed suicide. To our knowledge, this is the first time that the combined methods of pharmacoepidemiology and toxicology have been complemented with data concerning non-suicide deaths to address, by means of a case-control design, the influence of pharmacoadherence on suicide risk. Moreover, this is the first population-based study in which the ratio of initiated and discontinued prescriptions for psychotropic medications has been operationalized as a proxy for continued need of treatment.
Pharmacoadherence and completed suicide
The main result of the present study was that, in comparison with adherent use, both partial adherence and non-adherence to treatment with antidepressant and antipsychotic medications confer increased risks of completed suicide. However, after adjustments for variables reflecting the degree of somatic and psychiatric illness and continued need of psychotropic treatment, risk estimates for antidepressants were no longer significant. For antipsychotics, the latter adjustment resulted in risk-estimate increases for both partial adherence (from 4.72 to 6.66) and non-adherence (from 9.92 to 12.43), suggesting that a higher degree of continued treatment need was associated with a greater level of adherence (perhaps reflecting the use of long-acting injectables in severe psychosis).
An immediately evident explanation for the finding that partial adherence and non-adherence to psychotropic medication confer increased suicide risks is that discontinuation of a prescribed medication results in cessation of its pharmacodynamic antidepressive or antipsychotic effects, since states of depression and psychosis are well-known risk factors for suicide [39, 40]. Given the design of the study, however, it is difficult to draw convincing conclusions regarding causality. Indeed, another possibility is that the degree of mental illness is inversely related to adherence—that individuals with a greater burden of illness are less capable of sustaining continuous medication treatment, affecting the course of their illness [41]. A third possibility is that switching or discontinuation of psychotropic medications may give rise to withdrawal or rebound phenomena, whereby symptoms for which medications were originally prescribed, including suicidality, reoccur [42, 43].
Dispensations ratio
A subsidiary result of the study was that the average dispensation ratios in completed-suicide cases and non-suicide controls diverged markedly in the last month prior to death. In a further comparison of prescriptions for toxicologically verifiable psychotropic medications, the ratio for dispensed antidepressants in cases (2.1) exceeded the ratio for dispensed antidepressants in controls (0.6), as well as the ratios for dispensed antipsychotics in both cases (0.9) and controls (0.7). Since ratios exceeding 1.0 represent an increase in prescribed medications (newly initiated use of a single medication, or initiation of additional medications in the case of concomitant use), they are assumed to indicate the need of augmented treatment, for reasons that may include insufficient treatment response and increased severity of symptoms and signs, including suicidality. As the number of changes increased at a greater rate than the simultaneous increase in the dispensation ratio, in addition to the initiation of medications and restarting of previous non-continuous drug use, switching must also have occurred.
Although switching medications drives the dispensation ratio towards 1.0, it may nonetheless indicate a need for augmented treatment. In fact, recent findings suggest that switching of antidepressants confers a more than the two-fold elevated risk of suicidality in late life [44], yet, in the present study, adjustments for dispensation ratio had little effect on risk estimates for incomplete adherence to antidepressants. By contrast, the same adjustment increased risk estimates for incomplete adherence to antipsychotics, reflecting a difference between cases and controls regarding patterns of use of psychotropic medications in the months prior to death. Thus, it may be the case that non-suicidal individuals are less often treated with psychotropic medications, or that changes of psychotropic treatment entail the combined disadvantages of initiation side effects, discontinuation syndromes, and treatment gaps.
Strengths and limitations
The present dataset comprises reliable forensic-toxicological findings from a virtually complete national record of incidents of suspected unnatural death linked to individual-level information on all dispensed prescriptions. Further, by excluding substances with short half-lives, we compensated for lack of information regarding exact times of death and last administrated doses. One limitation is related to the possibility of intermittent use of prescribed medications. The calculated rates of adherence may therefore be overestimations of “long-term adherence,” but, at the same time accurate measures of “short-term adherence”—a phenomenon which, nonetheless, in itself, might influence suicide risk. Exclusion of deaths by intoxication should, in this study, be seen as both a strength and a limitation. Upon forensic investigation, an overdose of prescribed medications confounds judgments regarding pharmacoadherence, and level of suicidal intentionality is more difficult to determine in medication intoxications [45]. Yet, exclusion of intoxications meant that nearly a third of all instances of completed suicide in the study period were unaccounted for—and younger individuals and women underrepresented—limiting the generalizability of the results. Owing to the phenomena of postmortem redistribution—whereby concentrations of substances in the blood generally get elevated—it is conceivable that we have misclassified non-adherence subjects as adherent. Finally, although all investigated categories of pharmacoadherence presuppose a medical indication for treatment, lack of reliable clinical outpatient data precluded more precise adjustment for possible residual confounding by indication.
Clinical implications
Controls in our dataset showed a greater burden of somatic and psychiatric illness—recognized risk factors for both incomplete adherence and suicide—than in the general population. Thus, reported risk estimates for completed suicide are likely conservative underestimations, implying even superior real-world effectiveness regarding suicide risk for wholly adherent use of psychotropic medications. The most common first line of pharmacological treatment for (suicidal) depressive states is antidepressants. Although prior research has demonstrated antidepressive effects of augmentation with antipsychotics in isolated major depressive disorder, antipsychotics are rarely prescribed in the absence of co-occurring signs of psychosis or mania [46, 47]. Based on our results, we suspect that individuals prone to violent suicidality might benefit from adherent use of antipsychotics. However, owing to the lack of information regarding specific indications for investigated psychotropic medications, we cannot with certainty conclude that antipsychotics exert a general antisuicidal effect. Still, we recommend that antipsychotics be considered for the treatment of suicidality when other forms of treatment have failed—all the more since poor adherence to antipsychotics can be countered by the use of long-acting injectables. Finally, our results support the notion that in suicidal individuals treated with psychotropic medications, especially antidepressants, warning signs for adverse outcomes may be low adherence, switching of medications, and markedly increased polypharmacy. Upon the emergence of such signs, the threshold for inpatient care should be lowered to prevent suicidal behavior.
References
Haukka J, Tiihonen J, Harkanen T, Lönnqvist J (2008) Association between medication and risk of suicide, attempted suicide and death in nationwide cohort of suicidal patients with schizophrenia. Pharmacoepidemiol Drug Saf 17:686–696
Meltzer HY, Larry A, Green AI et al (2003) Clozapine treatment for suicidality in schizophrenia. Arch Gen Psychiatry 60:82–91
Lewitzka U, Severus E, Bauer R, Ritter P, Bauer M (2015) The suicide prevention effect of lithium : more than 20 years of evidence — a narrative review. Int J Bipolar Disord 3:32
Patchan KM, Program R, Richardson C et al (2015) The risk of suicide after clozapine discontinuation: cause for concern. Ann Clin Psychiatry 27:253–256
Sharma T, Guski LS, Freund N, Gøtzsche PC (2016) Suicidality and aggression during antidepressant treatment: systematic review and meta-analyses based on clinical study reports. BMJ 352. doi:https://doi.org/10.1136/bmj.i65
Thomas KH, Martin RM, Potokar J, Pirmohamed M, Gunnell D (2014) Reporting of drug induced depression and fatal and non-fatal suicidal behaviour in the UK from 1998 to 2011. BMC Pharmacol Toxicol 15:54
Stone M, Laughren T, Jones ML, Levenson M, Holland PC, Hughes A, Hammad TA, Temple R, Rochester G (2009) Risk of suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug Administration. BMJ 339:b2880
Högberg G, Antonuccio DO, Healy D (2015) Suicidal risk from TADS study was higher than it first appeared. Int J Risk Saf Med 27:85–91
Björkenstam C, Möller J, Ringbäck G, Salmi P, Hallqvist J, Ljung R (2013) An association between initiation of selective serotonin reuptake inhibitors and suicide - a nationwide register-based case-crossover study. PLoS One 8:1–6
Pompili M, Serafini G, Innamorati M, Ambrosi E, Giordano G, Girardi P, Tatarelli R, Lester D (2010) Antidepressants and suicide risk: a comprehensive overview. Pharmaceuticals 3:2861–2883
Ernst CL, Goldberg JF (2004) Antisuicide properties of psychotropic drugs: a critical review. Harv Rev Psychiatry 12:14–41
Corrado B, Eleonora E, Cipriani A (2009) Selective serotonin reuptake inhibitors and risk of suicide: a systematic review of observational studies. CMAJ 180:291–297
Schneeweiss S, Patrick AR, Solomon DH, Mehta J, Dormuth C, Miller M, Lee JC, Wang PS (2010) Variation in the risk of suicide attempts and completed suicides by antidepressant agent in adults. Arch Gen Psychiatry 67:497–506
Haukka J, Arffman M, Partonen T, Sihvo S, Elovainio M, Tiihonen J, Lönnqvist J, Keskimäki I (2009) Antidepressant use and mortality in Finland: a register-linkage study from a nationwide cohort. Eur J Clin Pharmacol 65:715–720
Tiihonen J, Lonnqvist J, Wahlbeck K, Klaukka T, Tanskanen A, Haukka J (2006) Antidepressants and the risk of suicide, attempted suicide, and overall mortality in a nationwide cohort. Arch Gen Psychiatry 63:1358–1367
Sondergard L, Kvist K, Andersen PK, Kessing L (2006) Do antidepressants prevent suicide? Int Clin Psychopharmacol 21:211–218
Baldessarini RJ, Tondo L, David P, Pompili M, Goodwin FK, Hennen J (2006) Decreased risk of suicides and attempts during long-term lithium treatment : a meta-analytic review. Bipolar Disord 8:625–639
Cassidy RM, Yang F, Kapczinski F, Passos IC (2018) Risk factors for suicidality in patients with schizophrenia : a systematic review, meta-analysis, and meta-regression of 96 studies. Schizophr Bull 44:787–797
Serafini G, Del CA, Rigucci S, Innamorati M, Girardi P, Tatarelli R (2009) Improving adherence in mood disorders: the struggle against relapse , recurrence and suicide risk. Expert Rev Neurother 9:985–1004
Erlangsen A, Agerbo E, Hawton K, Conwell Y (2009) Early discontinuation of antidepressant treatment and suicide risk among persons aged 50 and over: a population-based register study. J Affect Disord 119:194–199
Juurlink DN, Mamdani MM, Pharm D, Kopp A, Redelmeier DA, Sc M (2006) The risk of suicide with selective serotonin reuptake inhibitors in the elderly. Am J Psychiatry 163:813–821
Forsman J, Masterman T, Ahlner J, Isacsson G, Hedström AK (2019) Selective serotonin re-uptake inhibitors and the risk of violent suicide: a nationwide postmortem study. Eur J Clin Pharmacol 75:393–400
Benson T, Corry C, O’Neill S, Murphy S, Bunting B (2018) Use of prescription medication by individuals who died by suicide in Northern Ireland. Arch Suicide Res 1:139–152
Henriksson S, Boethius G, Isacsson G (2001) Suicides are seldom prescribed antidepressants: findings from a prospective prescription database in Jamtland county, Sweden, 1985-95. Acta Psychiatr Scand 103:301–306
Isacsson G, Bergman U, Rich CL (1994) Antidepressants, depression and suicide: an analysis of the San Diego study. J Affect Disord 32:277–286
Tanskanen A, Taipale H, Koponen M et al (2015) From prescriptions to drug use periods - a second generation method (PRE2DUP). BMC Res Notes 15:1–13
Nielsen LH, Lokkegaard E, Andreasen AH, Keiding N (2008) Using prescription registries to define continuous drug use: how to fill gaps between prescriptions. Pharmacoepidemiol Drug Saf 17:384–388
Forsman J, Taipale H, Masterman T, Tiihonen J, Tanskanen A (2018) Comparison of dispensed medications and forensic-toxicological findings to assess pharmacotherapy in the Swedish population 2006 to 2013. Pharmacoepidemiol Drug Saf 27(10):1112–1122
Hedlund J, Forsman J, Sturup J, Masterman T (2017) Psychotropic medications in Swedish homicide victims and offenders: a forensic-toxicological case-control study of adherence and recreational use. J Clin Psychiatry 78:797–802
Isacsson G, Ahlner J (2014) Antidepressants and the risk of suicide in young persons – prescription trends and toxicological analyses. Acta Psychiatr Scand 129:296–302
Reis M, Aamo T, Ahlner J, Druid H (2007) Reference concentrations of antidepressants. A compilation of postmortem and therapeutic levels. J Anal Toxicol 31:254–264
Roman M, Strom L, Tell H, Josefsson M (2013) Liquid chromatography/time-of-flight mass spectrometry analysis of postmortem blood samples for targeted toxicological screening. Anal Bioanal Chem 405:4107–4125
Schulz M, Iwersen-Bergmann S, Andresen H, Schmoldt A (2012) Therapeutic and toxic blood concentrations of nearly 1,000 drugs and other xenobiotics. Crit Care 16:1–4
McIntyre IM (2014) Liver and peripheral blood concentration ratio (L/P) as a marker of postmortem drug redistribution: a literature review. Forensic Sci Med Pathol 10:91–96
Leikin JB, Watson WA (2003) Post-mortem toxicology: what the dead can and cannot Tell us. J Toxicol Clin Toxicol 41:47–56
Zilg B, Thelander G, Giebe B, Druid H (2017) Postmortem blood sampling—comparison of drug concentrations at different sample sites. Forensic Sci Int 278:296–303
Cook DS, Braithwaite RA, Hale KA (2000) Estimating antemortem drug concentrations from postmortem blood samples: the influence of postmortem redistribution. J Clin Pathol 53:282–285
Tanskanen A, Taipale H, Koponen M, Tolppanen AM, Hartikainen S, Ahonen R, Tiihonen J (2014) From prescriptions to drug use periods - things to notice. BMC Res Notes 7:796
Chesney E, Goodwin GM, Fazel S (2014) Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry 13:153–160
Zalpuri I, Rothschild AJ (2016) Does psychosis increase the risk of suicide in patients with major depression? A systematic review. J Affect Disord 198:23–31
Higashi K, Medic G, Littlewood KJ, Diez T, Granström O, de Hert M (2013) Medication adherence in schizophrenia: factors influencing adherence and consequences of nonadherence, a systematic literature review. Ther Adv Psychopharmacol 3:200–218
Zabegalov KN, Kolesnikova TO, Khatsko SL et al (2018) Understanding antidepressant discontinuation syndrome (ADS) through preclinical experimental models. Eur J Pharmacol 829:129–140
Cerovecki A, Musil R, Klimke A, Seemüller F, Haen E, Schennach R, Kühn KU, Volz HP, Riedel M (2013) Withdrawal symptoms and rebound syndromes associated with switching and discontinuing atypical antipsychotics: theoretical background and practical recommendations. CNS Drugs 27:545–572
Hedna K, Andersson Sundell K, Hamidi A, Skoog I, Gustavsson S, Waern M (2018) Antidepressants and suicidal behaviour in late life: a prospective populationbased study of use patterns in new users aged 75 and above. Eur J Clin Pharmacol 74(2):201–208
Rockett IRH, Caine ED, Connery HS et al (2018) Discerning suicide in drug intoxication deaths: paucity and primacy of suicide notes and psychiatric history. PLoS One 13:1–13
Spielmans GI, Berman MI, Linardatos E, Rosenlicht NZ, Perry A, Tsai AC (2013) Adjunctive atypical antipsychotic treatment for major depressive disorder: a meta-analysis of depression, quality of life, and safety outcomes. PLoS Med 10:e1001403. https://doi.org/10.1371/journal.pmed.1001403
Papakostas GI, Shelton RC, Smith J, Fava M (2007) Augmentation of antidepressants with atypical antipsychotic medications for treatment-resistant major depressive disorder: a meta-analysis. J Clin Psychiatry 68:826–831
Contributors
All authors have contributed to the conception of the work, acquisition, analysis, and interpretation of the data. Further, all authors have taken part in the final drafts of the manuscript and revised it for important intellectual content. Before finally approving the manuscript to be published, questions related to the accuracy or integrity of the work were investigated and resolved by all authors.
Funding
Psykiatrifonden (Stockholm, Sweden) has in part funded the study by their 2015 grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
HT, JT, and AT have participated in research projects funded by Janssen-Cilag and Eli Lilly, with grants paid to the institution where they were employed. AT is a member of the Janssen-Cilag advisory board. JT has served as a consultant to the European Medical Agency and the Finnish Medicines Agency and has received lecture fees from Eli Lilly, Janssen-Cilag, Lundbeck, and Otsuka, and grants from the Stanley Foundation and the Sigrid Jusélius Foundation. JF and TM have received a grant from Psykiatrifonden (Stockholm, Sweden). All studied pharmacological products in this paper were generic substances without exclusive ownership by any company.
Role of the sponsor
The funding source had no role in the design or execution of the study; in the collection, management, analysis, or interpretation of the data; in the preparation, review or approval of the manuscript; or in the decision to submit the manuscript for publication.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. In this registry-based postmortem study, all personal information was anonymized, rendering unnecessary the need for formal consent or ethical approval. The study was nonetheless reviewed and approved by the Regional Ethical Review Board in Stockholm (2013/1411-31/5).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Forsman, J., Taipale, H., Masterman, T. et al. Adherence to psychotropic medication in completed suicide in Sweden 2006–2013: a forensic-toxicological matched case-control study. Eur J Clin Pharmacol 75, 1421–1430 (2019). https://doi.org/10.1007/s00228-019-02707-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-019-02707-z