Abstract
Purpose
To evaluate whether an educational intervention based on collegial discussions on patient cases could increase interns’ professional confidence in prescribing.
Methods
In a randomized controlled study at Sahlgrenska University Hospital, Gothenburg, Sweden, 69 interns (median age: 29 years, 54% female) were allocated to an intervention or control group. The intervention consisted of two 3-h seminars based on collegial discussions of patient cases focused on performing medication reviews. This included reconciling the drug treatment and ascertaining that it is reasonable given the patient’s current health status, as well as tips on practical handling of the medical records system and integrated decision support. Self-assessed confidence in performing medication reviews was evaluated with questionnaires distributed at baseline and at 6-month follow-up.
Results
Fifty-seven (83%) interns completed the questionnaires. Although the opposite was found at baseline, intervention interns, in comparison with controls, at follow-up, were more confident in performing medication reviews (4.3 ± 0.9 vs. 3.6 ± 1.3, P = 0.034; 1 = completely disagree to 5 = completely agree). At follow-up, the intervention participants had increased their confidence in prescribing to a greater extent compared with the control participants, including performing medication reviews as well as taking responsibility for the medication list at discharge: + 1.5/+ 1 vs ± 0 on the 5-point agreement scale (all P ≤ 0.01). Among other positive outcomes, the intervention increased the interns’ awareness of adverse effects as a potential cause of symptoms and their confidence in withdrawing a medication.
Conclusion
Structured collegial discussions on pharmacotherapy, even of a relatively short duration, can increase junior physicians’ professional confidence in prescribing medicines.
Similar content being viewed by others
Introduction
Prescribing is a core skill for a physician and is a complex task where diagnostic competence needs to be combined with pharmacological knowledge and patient communication. Indeed, physicians’ prescribing skills are the basis for rational and safe use of medicines. Therefore, it is essential that medical education focuses on the art of prescribing [1]. Nevertheless, a recent questionnaire study, administered in 26 medical schools in 17 European countries, reveals that final year students have poor knowledge of pharmacotherapy [2], and most European medical schools do not consider their students to be well prepared for prescribing [3]. Furthermore, prescribing skills have been shown to be insufficient in some junior doctors [4].
In many European countries, the medical degree in itself, often after 6 years of studies, confers the license to prescribe. In Sweden, where medical school is 5.5 years, the graduate needs to complete an additional 1.5 years of internship before getting a license to prescribe. However, in an unpublished survey on interns at Sahlgrenska University Hospital (n = 47; 2013), we found that a considerable proportion (60%) were not confident in performing medication reviews, that is, the basic skill of prescribing for which the physician is responsible according to the Swedish National Board of Health and Welfare [5]. Indeed, guidelines, recommendations, and indicators of prescribing quality may form the basis for decision making [6,7,8], but medical and pharmacological skills are prerequisites for the ability to plan prescribing appropriate to the medical conditions and preferences of each patient. In addition, an overemphasis on algorithmic rules may make the health care less patient-centered, and evidence-based guidelines often map poorly to complex multimorbidity [9].
The challenges related to prescribing are illustrated by the finding that students may be able to define pharmacological concepts but may be less prepared to discuss the meanings in depth and implement them in clinical practice [10]. Although training may be crucial for the professional progress, learning may be better facilitated by combining training with integrated medical education over time. However, to the best of our knowledge, randomized controlled studies evaluating how such educational efforts can strengthen young physicians’ confidence in prescribing are lacking in the scientific literature. Therefore, we performed this study aiming to evaluate whether an educational intervention for interns might facilitate their gain in confidence in prescribing.
Methods
We performed a randomized controlled study to investigate the effects of a short and structured educational intervention, based on collegial discussions of patient cases and targeting important pharmacotherapeutic aspects, on interns’ professional confidence regarding drug prescribing in clinical practice. The study was conducted at Sahlgrenska University Hospital in Region Västra Götaland, Sweden. Although interns in this hospital participate in weekly education within their employment, no seminar specifically focuses on the art of prescribing.
Participants and randomization
We (J.L. and S.M.W.) consecutively recruited participants among interns at Sahlgrenska University Hospital between September 2014 and March 2016. The inclusion criteria were (i) ≥ 6 months remaining of the 1-year, hospital-based internship (preceding the consecutive 6-month internship in primary care), and (ii) signed written informed consent. Eligible interns were individually asked by phone to participate and were sent written information. Where an intern could not be reached by phone, information was sent by post only. Since internship at Sahlgrenska University Hospital starts in clusters of ten, four times a year, we had four recruitment periods over 1 year, and asked approximately ten interns with each intake. During the first period, however, we approached all eligible interns with at least 6 months remaining of their hospital-based internship (n = 49).
Participants were randomly allocated to the intervention or the control group, stratified by sex, whether they had obtained their medical degree in Sweden or not, and whether the internship included time for research or not. Before any participant was assigned a study group, a random allocation sequence was generated for each stratum using the RANDBETWEEN function in Excel. To ensure comparable groups, although the number of participants in some strata was expected to be low, the randomization was performed in blocks of four (1:1). Each of the six possible block sequences was assigned a number between 1 and 6, and a random 15-number sequence was obtained for each stratum, forming the basis for a list of 60 sequential allocation assignments, each corresponding to a code number. Upon the inclusion of each cluster of interns, a list with initials and code numbers was provided, one for each stratum, to a person not involved in the study and without other information about the participants or the intervention. This person performed the allocation by combining initials with available code numbers.
Intervention interns received the intervention after the collection of baseline data and before the collection of follow-up data. Both groups performed their internship without further interactions with the study investigators. We offered all interns in the control group the intervention after follow-up data had been collected.
Intervention
The intervention was a short educational intervention designed to increase interns’ knowledge of the management of patients’ drug treatment in clinical practice. The intervention consisted of two 3-h seminars with time to review the information and practise in-between sessions. The rationale for this setup was that educational efforts on health care professionals have been shown to be most effective if they are mixed interactive and didactic, including at least two occasions over an extended period of time, and focusing on changing simple behaviors and outcomes that are likely to be perceived as serious [11, 12]. The seminars were led by one internist (J.L.) and one clinical pharmacologist (S.M.W. or K.N.). The intervention, including both seminars, was performed eight times, with a median of 3.5 participants per session (range 2–6).
The first seminar was scheduled 1–3 months after inclusion. It was structured to cover the different parts of medication reviews, including reconciliation of the drugs a patient has been prescribed and that they use; assessment of whether the treatment is reasonable or not, given the patient’s condition; and preparing a medication discharge summary for the patient and the next caregiver at discharge. The seminar was based on a total of four fictive or authentic cases, summarized in Appendix A. We included practical tips on how to use decision support tools within the electronic medical record system, for example regarding estimated glomerular filtration rate (eGFR) or how to use the integrated drug-drug interaction alert tool. We also introduced participants to the external drug-drug interaction database [13]. In addition, we highlighted keyboard shortcuts to facilitate the ordering of medicines in an efficient way. Further, the seminar focused on drugs which, in general, are considered inappropriate in older people, for example because of an increased risk of adverse effects [14]. At the end of the seminar, the participants received printed materials: (i) the regional prescribing guidelines booklet, (ii) a quick reference guide to medication reviews, and (iii) a quick reference guide to drug treatment in the elderly based on national indicators of prescribing quality [14].
As “homework” before the second seminar, scheduled 2–3 weeks after the first, the interns were to practise medication reviews, collect cases for the forthcoming seminar discussions, and reflect on physicians’ drug prescribing in clinical practice. During the second seminar, which was largely unspecified beforehand, we focused on a collegial discussion starting with the participants’ cases and experiences from their clinical practice.
The seminars were interactive and the interns were free to ask questions about situations or problems they had encountered. Because of the composition of the seminar tutors, the discussions were clinical and pharmacological at the same time, the aim being to grasp a broader perspective of safe and rational use of medicines and how physicians can contribute to this.
Outcomes
The effects of the intervention were evaluated by a questionnaire (Appendix B) designed for this study and tested for face validity on physicians not involved in the study. The questionnaire was distributed at baseline as well as at 6-month follow-up and included questions about the participant, for example concerning clinical experience and involvement in research, as well as statements to which the participants responded on a Likert scale ranging from 1 = completely disagree to 5 = completely agree.
The outcomes of the study were adjusted to the regulations by the Swedish National Board of Health and Welfare in which medication reviews are subdivided into two levels: basic and expanded. A basic medication review includes, for example, reconciliation of prescribed and actually used medications; assessing whether the medication list is reasonable taking into account the patients prior and current medical condition; considering side effects as a possible cause of the symptoms; reflecting on the importance of kidney function for a specific drug; determining the clinical relevance of potential drug-drug interactions with appropriate treatment adjustments where needed; and providing relevant information to the patient and the next caregiver at discharge. An expanded medication review implies that the physician reconsiders the drug treatment more thoroughly and over time, that is, assesses the benefit-risk balance for all drugs separately and combined and ensures that there is a reason for the treatment and that important drugs that the patient would probably benefit from are not left out. In this study, self-assessed confidence in performing basic medication reviews was the primary outcome, that is, the medication review primarily applicable in the hospital setting. For the sake of completeness, we also investigated the confidence in performing expanded medication reviews, which, in practice, are primarily performed by primary care physicians. In addition, we assessed the interns’ perceived knowledge of the components of basic and expanded medication reviews, as well as of various aspects of importance in drug prescribing, such as attention to kidney function, interactions, adverse effects, and whether a medication dose is reasonable.
After completion of the second seminar, we asked the participants to respond in writing to the questions “What was good about the seminars?” and “What could be improved?”
Statistics
All statistical analyses were performed with SPSS Statistics for Windows, version 22 (IBM SPSS, Armonk, NY, USA). To be able to detect a difference of 0.8 on a Likert scale from 1 to 5 with a standard deviation (SD) of 1.0 and a power of > 80%, we aimed to include 30 participants in each group (intervention and control), resulting in a total of 60 participants. To compensate for drop-outs after inclusion, we included about 10% more participants than indicated by the power calculation. We used the Mann-Whitney and Chi-square tests for comparisons between the randomization groups and Wilcoxon’s signed-rank and McNemar’s tests for within-group analyses. Categorical data are presented as numbers (percentages). To facilitate the interpretation of Likert scale results, mean ± SD is presented in addition to median and interquartile range (IQR), although normal distribution is not assumed in non-parametric statistics. Further, in bivariate statistics, those rating 4 or 5 were regarded as confident, and those rating 1–3 as not confident. Logistic regression was performed to obtain odds ratios (ORs) (and 95% confidence intervals (CIs)) for the intervention to predict perceived confidence in performing basic medication reviews at 6-month follow-up. Covariates included in the adjusted analysis were age, sex, research experience (vs. no research experience), total work experience before completing the follow-up questionnaire (months), baseline confidence (yes vs. no). A two-tailed p value < 0.05 was considered significant.
Results
A total of 57 (83%) interns (median age: 29 (IQR 27–34) years, 54% female, 28% with research included in the internship) completed the study and were included in the analysis: 26 in the intervention group and 31 in the control group (Fig. 1, Table 1). Regarding various aspects of prescribing, 55 (97%) and 45 (79%) interns, respectively, reported at baseline that they usually reconciled the medications ordered for, and actually used by, the patients. A total of 46 (81%) interns usually assessed the reasonableness of the drug treatment, taking the patient’s current situation into account. Furthermore, 26 (46%) interns stated that they considered adverse effects as a potential cause of symptoms; 26 (46%) that they usually reflected on the importance of kidney function for a specific drug; and 21 (37%) that they usually reflected on potential drug-drug interactions.
In all, 28 (49%) interns were confident in performing basic medication reviews at baseline. The corresponding figure for expanded medication reviews was 2 (4%). The randomization groups did not differ regarding age, sex, country of medical education, research internship, and clinical work experience. However, at baseline, the perceived confidence regarding basic medication reviews was lower in the intervention compared with the control group and a trend towards a higher baseline level of confidence in expanded medication reviews as well as more knowledge regarding both basic and expanded medication reviews was found among controls.
By contrast, at follow-up, the intervention interns rated their confidence in performing basic medication reviews higher compared with the controls: 4.3 ± 0.9 vs. 3.6 ± 1.3 (P = 0.034). Furthermore, more intervention than control interns was confident in practising this professional task (23 (88%) vs. 18 (58%), P = 0.011). At follow-up, intervention participants had increased their confidence in prescribing to a greater extent compared with the control participants, including performing medication reviews as well as taking responsibility for the medication list at discharge: + 1.5/+ 1 vs ± 0 on the 5-point Likert scale (all P ≤ 0.01; Table 2).
Without adjustments, the intervention resulted in 5.54 (95% CI: 1.37; 22.4) increased odds for being confident in performing basic medication reviews. After adjustment for age, sex, research experience, work experience before completing the follow-up questionnaire and baseline confidence, intervention interns, compared with controls, were 8.38 (1.37;39.7) times more likely to feel confident in performing such reviews (Table 3).
At follow-up compared with baseline, intervention interns had significantly increased their (i) assessment of the reasonableness of the drug treatment taking the patient’s current situation into account; (ii) consideration of adverse effects as a potential cause of symptoms; and (iii) confidence in withdrawing a medication; also (iv), they consulted more sources for reconciliation of medication (Table 4). No such increase was seen in the control group. Comparing the randomization groups at follow-up, all these aspects but the first, concerning the assessment of whether the drug treatment is reasonable, which was rated high from start, were rated higher by the intervention interns. For control interns, a positive development, from baseline to follow-up, was seen regarding reflection on prevention of double dosing, but no difference was found between the randomization groups at follow-up. Both intervention and control participants increased their awareness regarding potential drug-drug interactions.
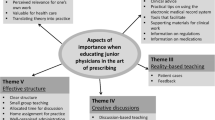
The submitted texts regarding the participants’ experiences of the seminars will be analyzed qualitatively in a separate publication. In brief, 17 (65%) out of 26 respondents spontaneously wrote that they appreciated the opportunity of having an open collegial discussion on the subject; ten (38%) that they liked the use of authentic cases to highlight important aspects of prescribing; and ten (38%) that they welcomed receiving practical tips on how to use decision support tools, the medical records system, and other sources of information. Regarding potential improvements, six (23%) respondents suggested including more patient cases for practising and five (19%) a longer period between the seminars in order to collect their own cases and practise performing medication reviews.
Discussion
In this study, we show that a short and structured educational intervention, consisting of two 3-h seminars based on collegial discussions on pharmacotherapeutic aspects of patient cases, can facilitate young physicians’ gain in professional confidence in prescribing. Indeed, after relevant adjustments, interns receiving the intervention were eight times more likely to be confident in the basics of prescribing, that is, of performing medication reviews in the hospital setting. The intervention also enhanced the self-perceived performance of several other important aspects related to safe and rational use of medicines. Although already from the start most interns routinely assessed whether the drug treatment was reasonable according to the patient’s current situation, an increased awareness of the patient’s health status and potential adverse effects was found in the intervention group at follow-up.
Interestingly, five out of ten interns were confident in performing basic medication reviews already at baseline. The corresponding figure for expanded medication reviews was considerably lower; less than one in 20. These findings may illustrate the complexity of drug treatment in clinical practice; medical school may sufficiently prepare most students concerning the theoretical basics and general prescribing guidelines, but experience and continuous medical education may be prerequisites to gaining confidence in the challenges associated with more advanced treatment considerations. In other words, early learning means gaining knowledge of facts, while advanced learning requires understanding, application, and analysis in order to provide a basis for synthesizing and applying the knowledge under new circumstances [15]. Indeed, a weak correlation between drug knowledge and treatment appropriateness has been reported [16]. Notwithstanding differences internationally in medical schools, it undoubtedly takes considerable time and efforts to become a skilled physician mastering the art of prescribing. This process requires dealing with large numbers of patients concerning diagnosis and treatment.
Our results suggest that general practice, at least in the short term, does not contribute substantially to interns’ confidence in prescribing. Indeed, in the control interns, little development was seen over 6 months. One interpretation of this finding is that allowing collegial discussions on drug treatment early after medical school may be necessary to facilitate the process of acquiring professional confidence in prescribing. During medical school training in performing medication reviews and writing discharge summaries may be sufficient to gain confidence in these core aspects of physicians’ prescribing responsibilities [17], but at the next stage of the learning process in becoming an experienced physician, collegial discussions may be required. Our results suggest that it may not suffice to rely on young physicians to achieve this complex knowledge on the go.
Unquestionably, prescribing-related matters are of major importance for the rational use of medicines. Worldwide, the use of drugs is increasing [18] and it is important that medications are added, withdrawn, and doses adjusted upon changes in a patient’s health status. This is the responsibility of the physician in every patient consultation. In fact, as patients’ conditions change over time, physicians cannot solely rely on the previous physician’s prescribing. Furthermore, as prescribing needs to incorporate medical issues, physicians cannot rely on other professions’ knowledge on drugs. In this context, our results are reassuring as they illustrate that a short educational intervention may make a large difference regarding the interns’ confidence in adding and withdrawing medications. Indeed, reluctance to withdraw medications prescribed by senior colleagues has been discussed as a potential reason for inappropriate treatment [19].
Comparison with previous studies
Our results may contribute to the understanding of why specially organized medication reviews have failed to show effects on the patient-relevant outcome mortality and hospitalizations [20,21,22,23,24]. In our study at baseline, the majority of the interns stated that they usually assessed whether the drug treatment, at the overall level, was reasonable, taking into account the patient’s health status. This finding suggests that the focus on drug-related matters over the last decades, including for example treatment guidelines, computerized support systems and benchmarking of prescribing practices, may have had positive effects on drug treatment practices among physicians. Furthermore, as specially organized medication reviews are costly in terms of personnel costs, the intervention in our study may constitute a simple approach for rational and safe use of medicines. Indeed, a health economics analysis based on a randomized controlled trial (RCT) revealed that specially organized medication reviews are probably not cost-effective [25]. As decision support tools integrated in the medical records system allow the physician to directly determine the clinical relevance of alerts for a specific patient, the need to manually check for interactions and general prescribing guidelines may be smaller compared with a decade ago. These developments also suggest that a few hours earmarked for structured collegial discussion on pharmacotherapy may make a difference even for more senior colleagues, as they may not be aware of the decision support tools available.
In the present study, we used self-perceived confidence as the primary outcome. In medical students, such confidence has been shown to be significantly but weakly correlated with prescribing competence [26]. In junior physicians, to the best of our knowledge, such correlation studies are lacking. One may speculate that the correlation between confidence and prescribing competence would be more prominent for individuals actually shouldering the responsibility for the patient’s treatment. To investigate if prescribing confidence varies according to role, we performed a post hoc analysis, in which we compared the proportion who completely disagreed with being confident in performing medication reviews between seventh-term medical students in Gothenburg (2016–2017; n = 386; response rate 82%) and the interns in the present study. A considerable discrepancy was found; 7% of the students and 23% of the interns were not at all confident (P = 0.0002). These findings may illustrate that self-perceived confidence varies according to role; junior physicians will face their own prescribing competence in their daily work, thereby potentially perceiving confidence accordingly. Indeed, a certain level of knowledge and experience, under one’s own responsibility, may be required to recognize that skills are lacking and that drug treatment in real life is complex.
Strengths and limitations of this study
The most important strength of this study is the randomized design. Few educational interventions have been evaluated with this key methodology to learn about causality. By chance, the randomization groups from the start differed in important aspects. The control group scored better than the intervention group at baseline. Therefore, the main results cannot be explained by beneficial study circumstances. Rather, these results may be considered even more robust because of the disadvantageous distribution at baseline. However, as scoring lower from start may leave greater room for improvements, comparisons of changes between the randomization groups regarding various aspects of importance in drug prescribing, such as attention to adverse reactions and withdrawing/adding medications, may hold limitations and must be interpreted with caution. Another strength is the high participation rate. Only five interns among those who could be reached by phone declined participation, and 57 out of 69 randomized participants completed questionnaires and were evaluable. Therefore, the external validity can be considered acceptable and the beneficial effects trustworthy, thereby providing important insight into the need for collegial pharmacotherapy discussions for young physicians. As medical schools in Sweden do not include an assessment of pharmacological and pharmacotherapeutic skills before graduation, as for example the Prescribing Safety Assessment (PSA) in the United Kingdom [27], our results may be applicable mainly in countries without such structured assessments.
A limitation of the study is that the intervention could not be blinded. Nevertheless, although participants were aware of their participation in the intervention, 6 months had passed between the baseline and follow-up questionnaires, and it is likely that few interns were aware of their first responses upon completing the second ones. Other limitations are the limited number of participants and that all randomized participants were not evaluable; 12 interns did not complete the follow-up questionnaire. Further, as discussed above, the primary outcome was a surrogate measure, that is, did not provide information on potential patient effects. In fact, the choice of outcome is a challenge in studies aiming to improve prescribing practices. To gain knowledge on patient effects, prohibitively large samples would be needed. Some would argue that the quality of prescribing in a random selection of patients could be determined. However, interns often execute drug orders by senior colleagues, and the actual input by the intern in prescribing matters is therefore not distinguishable. Further, there is no gold standard for quality assessments. Although indicators of prescribing quality are often used for such purposes [28, 29], they do not actually reflect quality; general guidelines may not be applicable at the individual level [30, 31]. The limited applicability of general guidelines for a specific patient also speaks against using a competence test to obtain the outcome measure; such tests inherently cover general aspects rather than patient-specific ones. Summarized, confidence in prescribing may constitute an acceptable happy medium between feasibility and clinical relevance. Nevertheless, we acknowledge that the association between prescribing competence and perceived confidence in junior physicians needs to be further elucidated.
Conclusion
In summary, this study shows that a few, brief, structured collegial discussions on drug treatment can increase professional confidence in prescribing among young physicians. As drug treatment is a core element of the professional responsibility of a physician, earmarking time and resources for such discussions may contribute to safe and rational use of medicines.
References
Brinkman DJ, Tichelaar J, Mokkink LB, Christiaens T, Likic R, Maciulaitis R, Costa J, Sanz EJ, Maxwell SR, Richir MC, van Agtmael MA, the Education Working Group of the European Association for Clinical Pharmacology and Therapeutics (EACPT) and its affiliated Network of Teachers in Pharmacotherapy (NOTIP) (2018) Key learning outcomes for clinical pharmacology and therapeutics education in Europe: a modified Delphi study. Clin Pharmacol Ther 104(2):317–325. https://doi.org/10.1002/cpt.962
Brinkman DJ, Tichelaar J, Schutte T, Benemei S, Bottiger Y, Chamontin B et al (2017) Essential competencies in prescribing: a first european cross-sectional study among 895 final-year medical students. Clin Pharmacol Ther 101(2):281–289. https://doi.org/10.1002/cpt.521
Brinkman DJ, Tichelaar J, Okorie M, Bissell L, Christiaens T, Likic R, Mačìulaitis R, Costa J, Sanz EJ, Tamba BI, Maxwell SR, Richir MC, van Agtmael M, for the Education Working Group of the European Association for Clinical Pharmacology and Therapeutics (EACPT) (2017) Pharmacology and therapeutics education in the European Union needs harmonization and modernization: a cross-sectional survey among 185 medical schools in 27 countries. Clin Pharmacol Ther 102(5):815–822. https://doi.org/10.1002/cpt.682
Harding S, Britten N, Bristow D (2010) The performance of junior doctors in applying clinical pharmacology knowledge and prescribing skills to standardized clinical cases. Br J Clin Pharmacol 69(6):598–606. https://doi.org/10.1111/j.1365-2125.2010.03645.x
The Swedish National Board of Health and Welfare (Socialstyrelsen) (2017) Socialstyrelsens föreskrifter och allmänna råd om ordination och hantering av läkemedel i hälso- och sjukvården (HSLF-FS 2017:37) [Internet]. Stockholm: Socialstyrelsen. [cited 2018 Aug 28] Available from: http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/20604/2017-5-2.pdf. Accessed 21 Jan 2019
The Swedish National Board of Health and Welfare (Socialstyrelsen) (2017) Indikatorer för god läkemedelsbehandling hos äldre [Internet]. Stockholm: Socialstyrelsen. [cited 2018 Aug 28]. Available from: http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/20644/2017-6-7.pdf. Accessed 21 Jan 2019
O'Connor MN, O'Sullivan D, Gallagher PF, Eustace J, Byrne S, O'Mahony D (2016) Prevention of hospital-acquired adverse drug reactions in older people using screening tool of older Persons' prescriptions and screening tool to alert to right treatment criteria: a cluster randomized controlled trial. J Am Geriatr Soc 64(8):1558–1566. https://doi.org/10.1111/jgs.14312
Axelsson MA, Spetz M, Mellen A, Wallerstedt SM (2008) Use of and attitudes towards the prescribing guidelines booklet in primary health care doctors. BMC Clin Pharmacol 8:8. https://doi.org/10.1186/1472-6904-8-8
Greenhalgh T, Howick J, Maskrey N (2014) Evidence based medicine: a movement in crisis? BMJ 348:g3725. https://doi.org/10.1136/bmj.g3725
Aronsson P, Booth S, Hagg S, Kjellgren K, Zetterqvist A, Tobin G et al (2015) The understanding of core pharmacological concepts among health care students in their final semester. BMC Med Educ 15:235. https://doi.org/10.1186/s12909-015-0522-z
Satterlee WG, Eggers RG, Grimes DA (2008) Effective medical education: insights from the Cochrane library. Obstet Gynecol Surv 63(5):329–333. https://doi.org/10.1097/OGX.0b013e31816ff661
Forsetlund L, Bjorndal A, Rashidian A, Jamtvedt G, O'Brien MA, Wolf F et al (2009) Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev (2):Cd003030. https://doi.org/10.1002/14651858.CD003030.pub2
Janusinfo (2017) Beslutsstöd/Janusmed interaktioner och riskprofil [Internet]. Stockholm: Janusinfo, Stockholms läns landsting. [cited 2018 Aug 28]. Available from: http://janusinfo.se/beslutsstod/janusmedinteraktionerochriskprofil.4.72866553160e98a7ddf1cdc.html. Accessed 21 Jan 2019
Fastbom J, Johnell K (2015) National indicators for quality of drug therapy in older persons: the Swedish experience from the first 10 years. Drugs Aging 32(3):189–199. https://doi.org/10.1007/s40266-015-0242-4
Bloom BS, Englehart MD, Furst EJ, Hill WH, Krathwohl DR (1956) The taxonomy of educational objectives, handbook I: The Cognitive domain. David McKay Co., Inc, New York
Brinkman DJ, van Rossem AP, Tichelaar J, Richir MC, van Agtmael MA (2017) Does medical students knowing more about drugs Lead to better treatment choices? J Clin Pharmacol 57(8):1071–1072. https://doi.org/10.1002/jcph.943
Eriksson AL, Wallerstedt SM (2018) Developing confidence in basic prescribing skills during medical school: a longitudinal questionnaire study investigating the effects of a modified clinical pharmacology course. Eur J Clin Pharmacol 74(10):1343–1349. https://doi.org/10.1007/s00228-018-2508-3
World Health Organization (2011) The World Medicines Situation Report 2011 [Internet]. Geneva: World Health Organization. [cited 2018 Aug 28]. Available from: http://www.who.int/medicines/areas/policy/world_medicines_situation/en/. Accessed 21 Jan 2019
Hedenrud TM, Svensson SA, Wallerstedt SM (2013) "psychiatry is not a science like others" - a focus group study on psychotropic prescribing in primary care. BMC Fam Pract 14:115. https://doi.org/10.1186/1471-2296-14-115
Christensen M, Lundh A (2013) Medication review in hospitalised patients to reduce morbidity and mortality. Cochrane Database Syst Rev 2:CD008986. https://doi.org/10.1002/14651858.CD008986.pub2
Hohl CM, Wickham ME, Sobolev B, Perry JJ, Sivilotti ML, Garrison S et al (2015) The effect of early in-hospital medication review on health outcomes: a systematic review. Br J Clin Pharmacol 80(1):51–61. https://doi.org/10.1111/bcp.12585
Wallerstedt SM, Kindblom JM, Nylen K, Samuelsson O, Strandell A (2014) Medication reviews for nursing home residents to reduce mortality and hospitalization: systematic review and meta-analysis. Br J Clin Pharmacol 78(3):488–497. https://doi.org/10.1111/bcp.12351
Lehnbom EC, Stewart MJ, Manias E, Westbrook JI (2014) Impact of medication reconciliation and review on clinical outcomes. Ann Pharmacother 48(10):1298–1312. https://doi.org/10.1177/1060028014543485
Huiskes VJ, Burger DM, van den Ende CH, van den Bemt BJ (2017) Effectiveness of medication review: a systematic review and meta-analysis of randomized controlled trials. BMC Fam Pract 18(1):5. https://doi.org/10.1186/s12875-016-0577-x
Wallerstedt SM, Bladh L, Ramsberg J (2012) A cost-effectiveness analysis of an in-hospital clinical pharmacist service. BMJ Open 2:e000329. https://doi.org/10.1136/bmjopen-2011-000329
Brinkman DJ, Tichelaar J, van Agtmael MA, de Vries TP, Richir MC (2015) Self-reported confidence in prescribing skills correlates poorly with assessed competence in fourth-year medical students. J Clin Pharmacol 55(7):825–830. https://doi.org/10.1002/jcph.474
Maxwell SRJ, Coleman JJ, Bollington L, Taylor C, Webb DJ (2017) Prescribing safety assessment 2016: delivery of a national prescribing assessment to 7343 UK final-year medical students. Br J Clin Pharmacol 83(10):2249–2258. https://doi.org/10.1111/bcp.13319
Guaraldo L, Cano FG, Damasceno GS, Rozenfeld S (2011) Inappropriate medication use among the elderly: a systematic review of administrative databases. BMC Geriatr 11:79. https://doi.org/10.1186/1471-2318-11-79
Tommelein E, Mehuys E, Petrovic M, Somers A, Colin P, Boussery K (2015) Potentially inappropriate prescribing in community-dwelling older people across Europe: a systematic literature review. Eur J Clin Pharmacol 71(12):1415–1427. https://doi.org/10.1007/s00228-015-1954-4
Lönnbro J, Wallerstedt SM (2017) Clinical relevance of the STOPP/START criteria in hip fracture patients. Eur J Clin Pharmacol 73(4):499–505. https://doi.org/10.1007/s00228-016-2188-9
Wallerstedt SM, Belfrage B, Fastbom J (2015) Association between drug-specific indicators of prescribing quality and quality of drug treatment: a validation study. Pharmacoepidemiol Drug Saf 24(9):906–914. https://doi.org/10.1002/pds.3827
Acknowledgements
We are grateful to all interns who participated in the study. We also want to thank the former internship heads of Sahlgrenska University Hospital, Caterina Finizia and Paulin Andréll, who contributed with knowledge on the internship structure and allowed us to perform the study within the interns’ working hours. In addition, we would like to thank Ulrika Wall for valuable input in the study design, and Lisa Lundberg for conducting the random allocation of the participants.
Data sharing statement
The datasets generated and analyzed during the current study are not publicly available owing to Swedish data protection laws. The data can be shared with authorized persons after approved application from the Regional Ethical Review Board in Gothenburg (https://www.epn.se/en/start/the-organisation/).
Funding
This study was supported by the Health and Medical Care Committee of Region Västra Götaland (grant numbers VGFOUREG-392071, VGFOUREG-476621). The funding source did not influence the design or conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, and approval of the manuscript.
Author information
Authors and Affiliations
Contributions
S.M.W. conceived the study, and S.M.W., K.N., and J.L. designed it. J.L. designed the seminars, and S.M.W., K.N., and J.L. conducted them. J.L. handled the data acquisition. S.M.W. and J.L. performed the statistical analyses and drafted the manuscript. K.N. revised the manuscript for intellectual content. J.L. and S.M.W. are guarantors of this work.
Corresponding author
Ethics declarations
Ethical approval
The study complies with the Declaration of Helsinki, and ethics approval was obtained from the Regional Ethical Review Board in Gothenburg (ID: 344-14).
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Lönnbro, J., Nylén, K. & Wallerstedt, S.M. Developing professional confidence in the art of prescribing—a randomized controlled study on structured collegial discussions during internship. Eur J Clin Pharmacol 75, 687–696 (2019). https://doi.org/10.1007/s00228-018-02619-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-018-02619-4