Abstract
Purpose
The present study was conducted to describe antipsychotic (AP) prevalent and incident use, characteristics of AP users, and their trends in the French population.
Methods
A cross-sectional study was repeated yearly from January 1, 2007 to December 31, 2013 (for prevalence analysis) or to December 31, 2012 (for incidence analysis) using the French Health Insurance reimbursement database (Echantillon Généraliste de Bénéficiaires, EGB). For each year studied, prevalent and incident AP users were described in terms of age and gender overall, and according to the type of AP (FGAPs or SGAPs) used at index date. In addition, concurrent medications and comorbidities that a priori contraindicate the use of drugs having atropinic properties were researched.
Results
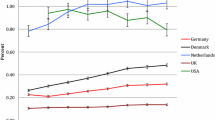
Prevalence and incidence remained relatively stable along the 2007–2013 period. Trends slightly decreased, from 2.07% (n = 10,252) to 2.05% (n = 11,015) for prevalence, and from 0.73% (n = 3461) to 0.66% (n = 3363) for incidence, especially in elderly, in contrast of children and adolescents (+ 39% for prevalence, from 184 to 271). The number of coprescribed drugs was found high (median = 5) and remained constant over time. In 2013, about 7% of prevalent AP users presented with a comorbidity increasing the risk of atropinic ADRs, and 36% used at least one concurrent atropinic drug. In incident AP users, these numbers were of 8 and 29%, respectively.
Conclusions
The present study highlighted a marked shift from FGAPs toward SGAPs, as well as an increase in AP use in children and adolescents in France.


Similar content being viewed by others
References
Rang HP, Dale MM, Ritter JM et al (2011) Rang & Dale’s Pharmacology, 7th edn. Churchill Livingstone, London
Cáceres MC, Peñas-Lledó EM, de la Rubia A et al (2008) Increased use of second generation antipsychotic drugs in primary care: potential relevance for hospitalizations in schizophrenia patients. Eur J Clin Pharmacol 64(1):73–76. https://doi.org/10.1007/s00228-007-0386-1
Verdoux H, Tournier M, Bégaud B (2010) Antipsychotic prescribing trends: a review of pharmaco-epidemiological studies. Acta Psychiatr Scand 121(1):4–10. https://doi.org/10.1111/j.1600-0447.2009.01425.x
Moncrieff J (2013) Magic bullets for mental disorders: the emergence of the concept of an ‘antipsychotic’ drug. J Hist Neurosci 22(1):30–46. https://doi.org/10.1080/0964704X.2012.664847
Carton L, Cottencin O, Lapeyre-Mestre M, Geoffroy P, Favre J, Simon N, Bordet R, Rolland B (2015) Off-label prescribing of antipsychotics in adults, children and elderly individuals: a systematic review of recent prescription trends. Curr Pharm Des 21(23):3280–3297. https://doi.org/10.2174/1381612821666150619092903
Moulis G, Lapeyre-Mestre M, Palmaro A, Pugnet G, Montastruc JL, Sailler L (2015) French health insurance databases: what interest for medical research? Rev Med Interne 36(6):411–417. https://doi.org/10.1016/j.revmed.2014.11.009
Tuppin P, de Roquefeuil L, Weill A, Ricordeau P, Merlière Y (2010) French national health insurance information system and the permanent beneficiaries sample. Rev Epidemiol Sante Publique 58(4):286–290. https://doi.org/10.1016/j.respe.2010.04.005
Aging Brain Care. Anticholinergic Cognitive Burden Scale—2012 Update. Available: www.agingbraincare.org/uploads/products/ACB_scale_-_legal_size.pdf
Laroche ML, Charmes JP, Bouthier F, Merle L (2009) Inappropriate medications in the elderly. Clin Pharmacol Ther 85(1):94–97. https://doi.org/10.1038/clpt.2008.214
Ilyas S, Moncrieff J (2012) Trends in prescriptions and costs of drugs for mental disorders in England, 1998-2010. Br J Psychiatry 200(5):393–398. https://doi.org/10.1192/bjp.bp.111.104257
Nguyen TTH, Pariente A, Montastruc J-L, et al. An original pharmacoepidemiologic - pharmacodynamic method: application to antipsychotic-induced movement disorders. Br J Clin Pharmacol Published Online First: 30 September 2016. https://doi.org/10.1111/bcp.13145
Montastruc F, Palmaro A, Bagheri H, Schmitt L, Montastruc JL, Lapeyre-Mestre M (2015) Role of serotonin 5-HT2C and histamine H1 receptors in antipsychotic-induced diabetes: a pharmacoepidemiological-pharmacodynamic study in VigiBase. Eur Neuropsychopharmacol 25(10):1556–1565. https://doi.org/10.1016/j.euroneuro.2015.07.010
Moncrieff J (2014) The medicalisation of ‘ups and downs’: the marketing of the new bipolar disorder. Transcult Psychiatry 51(4):581–598. https://doi.org/10.1177/1363461514530024
Healy D (2006) The latest mania: selling bipolar disorder. PLoS Med 3(4):e185. https://doi.org/10.1371/journal.pmed.0030185
Jones DR, Macias C, Barreira PJ, Fisher WH, Hargreaves WA, Harding CM (2004) Prevalence, severity, and co-occurrence of chronic physical health problems of persons with serious mental illness. Psychiatr Serv 55(11):1250–1257. https://doi.org/10.1176/appi.ps.55.11.1250
Leucht S, Burkard T, Henderson J, Maj M, Sartorius N (2007) Physical illness and schizophrenia: a review of the literature. Acta Psychiatr Scand 116(5):317–333. https://doi.org/10.1111/j.1600-0447.2007.01095.x
Ganguly R, Kotzan JA, Miller LS, Kennedy K, Martin BC (2004) Prevalence, trends, and factors associated with antipsychotic polypharmacy among Medicaid-eligible schizophrenia patients, 1998-2000. J Clin Psychiatry 65(10):1377–1388. https://doi.org/10.4088/JCP.v65n1013
Geddes J, Freemantle N, Harrison P, Bebbington P (2000) Atypical antipsychotics in the treatment of schizophrenia: systematic overview and meta-regression analysis. BMJ 321(7273):1371–1376. https://doi.org/10.1136/bmj.321.7273.1371
Peluso MJ, Lewis SW, Barnes TRE, Jones PB (2012) Extrapyramidal motor side-effects of first- and second-generation antipsychotic drugs. Br J Psychiatry 200(5):387–392. https://doi.org/10.1192/bjp.bp.111.101485
Hugenholtz GWK, Heerdink ER, Stolker JJ, Meijer WE, Egberts ACG, Nolen WA (2006) Haloperidol dose when used as active comparator in randomized controlled trials with atypical antipsychotics in schizophrenia: comparison with officially recommended doses. J Clin Psychiatry 67(06):897–903. https://doi.org/10.4088/JCP.v67n0606
Tsai AC, Rosenlicht NZ, Jureidini JN, Parry PI, Spielmans GI, Healy D (2011) Aripiprazole in the maintenance treatment of bipolar disorder: a critical review of the evidence and its dissemination into the scientific literature. PLoS Med 8(5):e1000434. https://doi.org/10.1371/journal.pmed.1000434
Verdoux H, Pambrun E, Cortaredona S, Tournier M, Verger P (2015) Antipsychotic prescribing in youths: a French community-based study from 2006 to 2013. Eur Child Adolesc Psychiatry 24(10):1181–1191. https://doi.org/10.1007/s00787-014-0668-y
Gallini A, Andrieu S, Donohue JM, Oumouhou N, Lapeyre-Mestre M, Gardette V (2014) Trends in use of antipsychotics in elderly patients with dementia: impact of national safety warnings. Eur Neuropsychopharmacol 24(1):95–104. https://doi.org/10.1016/j.euroneuro.2013.09.003
Vinogradov S, Fisher M, Warm H et al (2009) The cognitive cost of anticholinergic burden: decreased response to cognitive training in schizophrenia. Am J Psychiatry 166(9):1055–1062. https://doi.org/10.1176/appi.ajp.2009.09010017
Brébion G, Bressan RA, Amador X et al (2004) Medications and verbal memory impairment in schizophrenia: the role of anticholinergic drugs. Psychol Med 34(2):369–374. https://doi.org/10.1017/S0033291703008900
Rehse M, Bartolovic M, Baum K, Richter D, Weisbrod M, Roesch-Ely D (2016) Influence of antipsychotic and anticholinergic loads on cognitive functions in patients with schizophrenia. Schizophr Res Treatment 2016:8213165. https://doi.org/10.1155/2016/8213165
Palmaro A, Moulis G, Despas F, Dupouy J, Lapeyre-Mestre M (2016) Overview of drug data within French health insurance databases and implications for pharmacoepidemiological studies. Fundam Clin Pharmacol 30(6):616–624. https://doi.org/10.1111/fcp.12214
Funding
The present study is part of the Drugs Systematized Assessment in real-liFe Environment (DRUGS-SAFE) research programme. This programme aims at providing an integrated system allowing the concomitant monitoring of drug use and drug safety in France. It is funded by the French Agence Nationale de Sécurité du Médicament et des produits de santé (ANSM). This publication represents the views of the authors and does not necessarily that of the ANSM.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Montastruc, F., Bénard-Laribière, A., Noize, P. et al. Antipsychotics use: 2006–2013 trends in prevalence and incidence and characterization of users. Eur J Clin Pharmacol 74, 619–626 (2018). https://doi.org/10.1007/s00228-017-2406-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-017-2406-0