Abstract
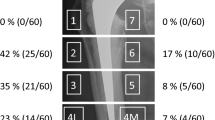
Implant failure and periprosthetic fractures because of periprosthetic bone loss are a major concern in total hip arthroplasty (THA). Hardly any clinical data exist on the long-term evolution of bone mineral density (BMD) around uncemented femoral implants. The question to address is whether relevant bone loss continues into third decade around well-fixed uncemented femoral implants. BMD around stable uncemented straight titanium femoral implants was assessed in a longitudinal cohort study. We included 142 hips of 128 patients and measured the development of the periprosthetic BMD using dual-energy X-ray absorptiometry. The baseline measurement was 12 years (t1) after the implantation of an uncemented femoral stem. Follow-up-measurements were performed at 17 (t2) and at 21 years (t3) after primary THA. The regions of interest (ROI) were selected conforming to Gruen et al. We acquired complete data including three consecutive measurements (t1, t2, t3) for 42 patients (49 hips). Performing radiographic evaluation at t1, t2 and t3, we found a regular bone-implant interface present in all cases. Significant decrease in BMD could be shown in ROI 1 (p = 0.0001; − 7.8%), 4 (p = 0.024; − 2.4%), 6 (p = 0.001; − 5.5%) and 7 (p < 0.0001; − 11.7%) between t1 and t3 and in ROI 1 (p = 0.002; − 3.7%), 2 (p = 0.046; − 3.6%), 4 (p = 0.002; − 2.7%) and 7 (p < 0.0001; − 8.0%) between t2 and t3. There were significant differences in overall bone density (netavg) between t1 and t3 (p = 0.001; − 3.6%) and between t2 and t3 (p = 0.020; − 2.1%). The data indicate clinically relevant changes of BMD especially in the proximal Gruen zones in the long-term after uncemented THA. Loss of periprosthetic BMD might be a risk factor for periprosthetic fractures.



Similar content being viewed by others
References
Streit MR, Innmann MM, Merle C, Bruckner T, Aldinger PR, Gotterbarm T (2013) Long-term (20- to 25-year) results of an uncemented tapered titanium femoral component and factors affecting survivorship. Clin Orthop Relat Res 471(10):3262–3269. https://doi.org/10.1007/s11999-013-3033-4
Aldinger PR, Jung AW, Breusch SJ, Ewerbeck V, Parsch D (2009) Survival of the cementless Spotorno stem in the second decade. Clin Orthop Relat Res 467(9):2297–2304. https://doi.org/10.1007/s11999-009-0906-7
de Witte PB, Brand R, Vermeer HG, van der Heide HJ, Barnaart AF (2011) Mid-term results of total hip arthroplasty with the CementLess Spotorno (CLS) system. J Bone Joint Surg Am 93(13):1249–1255. https://doi.org/10.2106/JBJS.I.01792
Grappiolo G, Burastero G, Moraca G, Camera A, Santoro G, Gruen T, Spotorno L (2009) The CLS stem in primary THA. Long-term results and survivorship analysis of a tapered, grit-blasted, press-fit femoral prosthesis. J Bone Joint Surg 91-B(SUPP I):51
Engh CA Jr, Young AM, Engh CA Sr, Hopper RH Jr (2003) Clinical consequences of stress shielding after porous-coated total hip arthroplasty. Clin Orthop Relat Res 417:157–163. https://doi.org/10.1097/01.blo.0000096825.67494.e3
Lindahl H (2007) Epidemiology of periprosthetic femur fracture around a total hip arthroplasty. Injury 38(6):651–654. https://doi.org/10.1016/j.injury.2007.02.048
Dan D, Germann D, Burki H, Hausner P, Kappeler U, Meyer RP, Klaghofer R, Stoll T (2006) Bone loss after total hip arthroplasty. Rheumatol Int 26(9):792–798. https://doi.org/10.1007/s00296-005-0077-0
Rahmy AI, Gosens T, Blake GM, Tonino A, Fogelman I (2004) Periprosthetic bone remodelling of two types of uncemented femoral implant with proximal hydroxyapatite coating: a 3-year follow-up study addressing the influence of prosthesis design and preoperative bone density on periprosthetic bone loss. Osteoporos Int 15(4):281–289. https://doi.org/10.1007/s00198-003-1546-5
Grochola LF, Habermann B, Mastrodomenico N, Kurth A (2008) Comparison of periprosthetic bone remodelling after implantation of anatomic and straight stem prostheses in total hip arthroplasty. Arch Orthop Trauma Surg 128(4):383–392. https://doi.org/10.1007/s00402-007-0507-4
Braun A, Papp J, Reiter A (2003) The periprosthetic bone remodelling process–signs of vital bone reaction. Int Orthop 27(Suppl 1):S7-10
Merle C, Streit MR, Volz C, Pritsch M, Gotterbarm T, Aldinger PR (2011) Bone remodeling around stable uncemented titanium stems during the second decade after total hip arthroplasty: a DXA study at 12 and 17 years. Osteoporos Int 22(11):2879–2886. https://doi.org/10.1007/s00198-010-1483-z
Boden HS, Skoldenberg OG, Salemyr MO, Lundberg HJ, Adolphson PY (2006) Continuous bone loss around a tapered uncemented femoral stem: a long-term evaluation with DEXA. Acta Orthop 77(6):877–885. https://doi.org/10.1080/17453670610013169
Panisello JJ, Herrero L, Canales V, Herrera A, Martinez AA, Mateo J (2009) Long-term remodeling in proximal femur around a hydroxyapatite-coated anatomic stem: ten years densitometric follow-up. J Arthroplast 24(1):56–64. https://doi.org/10.1016/j.arth.2007.12.017
Stiehl JB (2009) Long-term periprosthetic remodeling in THA shows structural preservation. Clin Orthop Relat Res 467(9):2356–2361. https://doi.org/10.1007/s11999-009-0722-0
Gruen TA, McNeice GM, Amstutz HC (1979) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 141:17–27
Willert HG, Bertram H, Buchhorn GH (1990) Osteolysis in alloarthroplasty of the hip. The role of ultra-high molecular weight polyethylene wear particles. Clin Orthop Relat Res 258:95–107
Engh CA, Bobyn JD, Glassman AH (1987) Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg 69(1):45–55
Gibbons CE, Davies AJ, Amis AA, Olearnik H, Parker BC, Scott JE (2001) Periprosthetic bone mineral density changes with femoral components of differing design philosophy. Int Orthop 25(2):89–92
Sychterz CJ, Engh CA (1996) The influence of clinical factors on periprosthetic bone remodeling. Clin Orthop Relat Res 322:285–292
Kroger H, Venesmaa P, Jurvelin J, Miettinen H, Suomalainen O, Alhava E (1998) Bone density at the proximal femur after total hip arthroplasty. Clin Orthop Relat Res 352:66–74
Nishii T, Sugano N, Masuhara K, Shibuya T, Ochi T, Tamura S (1997) Longitudinal evaluation of time related bone remodeling after cementless total hip arthroplasty. Clin Orthop Relat Res 339:121–131
Wolff J (1986) The law of bone remodelling. Springer, Berlin
Venesmaa PK, Kröger HP, Miettinen HJ, Jurvelin JS, Suomalainen OT, Alhava EM (2001) Monitoring of periprosthetic BMD after uncemented total hip arthroplasty with dual-energy X-ray absorptiometry—a 3-year follow-up study. J Bone Miner Res 16(6):1056–1061
Kröger H, Miettinen H, Arnala I, Koski E, Rushton N, Suomalainen O (1996) Evaluation of periprosthetic bone using dual-energy X-ray absorptiometry: precision of the method and effect of operation on bone mineral density. J Bone Miner Res 11(10):1526–1530
Karachalios T, Tsatsaronis C, Efraimis G, Papadelis P, Lyritis G, Diakoumopoulos G (2004) The long-term clinical relevance of calcar atrophy caused by stress shielding in total hip arthroplasty: a 10-year, prospective, randomized study1 1No benefits or funds were received in support of this study. J Arthroplast 19(4):469–475
Wilkinson JM, Hamer AJ, Rogers A, Stockley I, Eastell R (2003) Bone mineral density and biochemical markers of bone turnover in aseptic loosening after total hip arthroplasty. J Orthop Res 21(4):691–696. https://doi.org/10.1016/s0736-0266(02)00237-1
Tapaninen T, Kroger H, Venesmaa P (2015) Periprosthetic BMD after cemented and uncemented total hip arthroplasty: a 10-year follow-up study. J Orthop Sci 20(4):657–662. https://doi.org/10.1007/s00776-015-0722-8
Hannan MT, Felson DT, Dawson-Hughes B, Tucker KL, Cupples LA, Wilson PW, Kiel DP (2000) Risk factors for longitudinal bone loss in elderly men and women: the Framingham Osteoporosis Study. J Bone Miner Res 15(4):710–720. https://doi.org/10.1359/jbmr.2000.15.4.710
World-Health-Organization (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Org Tech Rep Ser 843:1-129
Leslie WD, Brennan-Olsen SL, Morin SN, Lix LM (2016) Fracture prediction from repeat BMD measurements in clinical practice. Osteoporos Int 27(1):203–210. https://doi.org/10.1007/s00198-015-3259-y
Innmann MM, Streit MR, Bruckner T, Merle C, Gotterbarm T (2017) Comparable cumulative incidence of late periprosthetic femoral fracture and aseptic stem loosening in uncemented total hip arthroplasty-a concise follow-up report at a minimum of 20 years. J Arthroplast. https://doi.org/10.1016/j.arth.2017.11.022
Synder M, Krajewski K, Sibinski M, Drobniewski M (2015) Periprosthetic bone remodeling around short stem. Orthopedics 38(3 Suppl):S40–S45. https://doi.org/10.3928/01477447-20150215-55
Tran P, Zhang BX, Lade JA, Pianta RM, Unni RP, Haw CS (2016) Periprosthetic bone remodeling after novel short-stem neck-sparing total hip arthroplasty. J Arthroplast 31(11):2530–2535. https://doi.org/10.1016/j.arth.2016.04.023
Huo SC, Wang F, Dong LJ, Wei W, Zeng JQ, Huang HX, Han QM, Duan RQ (2016) Short-stem prostheses in primary total hip arthroplasty: a meta-analysis of randomized controlled trials. Medicine 95(43):e5215. https://doi.org/10.1097/md.0000000000005215
Freitag T, Hein MA, Wernerus D, Reichel H, Bieger R (2016) Bone remodelling after femoral short stem implantation in total hip arthroplasty: 1-year results from a randomized DEXA study. Arch Orthop Trauma Surg 136(1):125–130. https://doi.org/10.1007/s00402-015-2370-z
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
David S. Peitgen, Moritz Innmann and Babak Moradi declare that they have no conflict of interest. Christian Merle has received a speaker honorarium from Company ZimmerBiomet. Tobias Gotterbarm has received a speaker and consultancy honorarium and travel expenses from Company Depuy Synthes. Marcus R Streit has received an honorarium for development of educational presentations from Company Depuy Synthes. The institution of one or more of the authors (DSP, MI, CM, TG, BM, MRS) has received funding from the noncommercial research fund of Deutsche Arthrose-Hilfe e.V. and Zimmer Europe (Winterthur, Switzerland).
Human and Animal Rights and Informed Consent
All patients gave informed consent and the institutional review board of the University of Heidelberg approved all procedures. The study was conducted in accordance with the Helsinki Declaration of 1975 as revised in 2013.
Rights and permissions
About this article
Cite this article
Peitgen, D.S., Innmann, M.M., Merle, C. et al. Periprosthetic Bone Mineral Density Around Uncemented Titanium Stems in the Second and Third Decade After Total Hip Arthroplasty: A DXA Study After 12, 17 and 21 Years. Calcif Tissue Int 103, 372–379 (2018). https://doi.org/10.1007/s00223-018-0438-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-018-0438-9