Abstract
Summary
This study examined the imminent risk of a future fracture within 1 and 2 years following a first fracture in women aged 50 years and older and assessed independent factors associated with risk of subsequent fractures. The study highlights the need to intervene rapidly after a fracture to prevent further fractures.
Introduction
This study aims to determine the imminent risk of subsequent fractures within 1 and 2 years following a first fracture and to assess independent factors associated with subsequent fractures.
Methods
Retrospective, observational cohort study of women aged ≥ 50 years with a fragility fracture was identified from Swedish national registers. Clinical/demographic characteristics at the time of index fracture and cumulative fracture incidences up to 12 and 24 months following index fracture were calculated. Risk factors for subsequent fracture were identified using multivariate regression analysis.
Results
Two hundred forty-two thousand one hundred eight women (mean [SD] age 74 [12.5] years) were included. The cumulative subsequent fracture incidence at 12 months was 7.1% (95% confidence interval [CI], 6.9–7.2) and at 24 months was 12.0% (95% CI, 11.8–12.1). The rate of subsequent fractures was highest in the first month (~ 15 fractures per 1000 patient-years) and remained steady between 4 and 24 months (~ 5 fractures/1000 patient-years). Higher age was an independent risk factor for imminent subsequent fractures (at 24 months, sub-distribution hazard ratio [HR], 3.07; p < 0.001 for women 80–89 years [reference 50–59 years]). Index vertebral fracture was a strong independent risk factor for subsequent fracture (sub-distribution HR, 2.72 versus hip fracture; p < 0.001 over 12 months; HR, 2.23; p < 0.001 over 24 months).
Conclusions
Our findings highlight the need to intervene rapidly after any fragility fracture in postmenopausal women. The occurrence of a fragility fracture provides healthcare systems with a unique opportunity to intervene to reduce the increased risk of subsequent fractures.
Similar content being viewed by others
Introduction
Fragility fractures due to osteoporosis are common. More than nine million fragility fractures have been estimated worldwide based on the year 2000 [1], and in Europe, 3.5 million fragility fractures were reported to occur annually [2]. In a study of patient records in Malmö, Sweden, for women aged 50 years, the lifetime probability of a fragility fracture was 23% for hip fracture and 15% for clinical vertebral fracture [3]. Moreover, the number of fragility fractures is expected to rise as the population ages, and in Europe, a 28% increase in the number of fragility fractures has been estimated by 2025 [4].
Fragility fractures cause substantial individual burden related to the significant reduction in a patient’s mobility, function, and quality of life [5, 6]. The increase in morbidities associated with fragility fractures is greater than can be attributed to aging alone and represents a major clinical problem [7]. Fragility fractures also lead to an increase in mortality [8,9,10,11,12]. Consequently, an understanding of the variables leading to fracture is an important area of research, to enable treatment strategies to focus on those most at risk and effectively reduce the clinical burden of disease.
Multiple factors are known to increase the risk of sustaining a fragility fracture [13]. Among them, prior fragility fracture is a well-documented major risk factor for future fragility fracture [13,14,15,16,17]. On average, the risk of future fracture is doubled in the presence of a prior fracture [18,19,20]. In the Reykjavik study of 30,795 men and women, the risk of a second major osteoporotic fracture (MOF) within the year following the first fracture was 2.7-fold higher than the risk seen in the whole of the study population [21]. In addition, a significant number of patients who sustain a hip or wrist fracture have a history of up to three previous fractures [22].
The risk of a subsequent fracture changes over time, and the time elapsed since sustaining a prior fracture is now recognized as an important factor influencing subsequent fracture risk. The concept of “imminent risk” for fracture, defined as a markedly elevated risk of fracture within the next 12–24 months, has been emphasized [19, 23, 24]. In a study of postmenopausal women in The Netherlands, the risk of subsequent fracture was highest within the first year following the initial fracture [25]. This risk decreased over time, but remained higher compared with the whole of the study population during the follow-up period. Age is also an independent predictor of future fracture [21, 26]. In a study of women in the USA, the incidence of any clinical fracture at 1 and 2 years following the initial fracture was 10% and 18%, respectively [26], but the corresponding figures for women ≥ 75 years of age were higher, with a 2-year fracture risk of 25%. All-cause mortality is also highest in the year following a hip fracture [5, 10, 23, 27, 28].
Tools to assess the risk of fragility fracture are extensively used to make clinical decisions [29,30,31]. FRAX®, University of Sheffield, in particular allows the identification of patients at high risk for fracture more effectively than bone mineral density (BMD) measures alone [32]. Accordingly, FRAX has proved useful in identifying individuals at risk of fracture over 10 years and assisting therapeutic decisions, but at present does not take into account the time since fracture or fracture location and was not primarily designed to identify patients at imminent risk of fracture. However, a recent publication suggests that FRAX could be adapted to predict fracture over a shorter period [33]. The need for research to identify the determinants of imminent fracture risk was recently reported in a consensus meeting for the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) [24].
Currently, many patients do not receive treatment for their osteoporosis after a fragility fracture, despite the recognition that sustaining a fracture increases the risk of a subsequent fracture [2, 13, 21, 34, 35]. Therefore, a more robust approach to the identification of patients at imminent risk of fracture is important and could prove relevant to determine the best treatment strategies for patients at increased fracture risk. This approach should also include other independent factors that may increase the risk of imminent fracture and may provide insights into a select group of patients in whom rapid intervention to decrease fracture risk is essential.
The aim of the current study was to determine the incidence of subsequent fractures within 1 and 2 years following a first fracture in a population-based study of women in Sweden, and to assess independent factors associated with subsequent fracture. This large-scale Swedish study was designed to strengthen the knowledge around the driving factors for imminent fracture risk.
Methods
Study participants
This was a retrospective, observational cohort study of women with a fragility fracture. Study participants were women aged ≥ 50 years with a fragility fracture at any skeletal location, between the dates 1 July 2006 and 31 December 2012. Women were identified from the National Patient Register (Patientregistret; NPR). The NPR contains patient, geographic, administrative, and medical data for all inpatient and outpatient hospital care in Sweden.
The NPR and the Swedish Prescribed Drug Register (Läkemedelsregistret; PDR) were used to collect data on demographic and potential clinical risk factors for fracture. The PDR contains information on all prescriptions filled at pharmacies in Sweden and is updated monthly; it also contains information on gender, age, and residency of the patients. Date of patient death was obtained from the Cause of Death Register. The register includes statistics on causes of deaths for all of Sweden. All three registers are held by the Swedish Board of Health and Welfare. Complete data from all of the registers up until 31 December 2012 were available for analysis for all patients included in the study population.
To exclude other potential pathologic causes of fracture, women with a diagnosis of Paget’s disease, or a malignancy (other than basal cell carcinoma) at any time during the study, were excluded from the analysis.
Study design
In this retrospective, observational cohort study, clinical and demographic characteristics were collected at the time of the first (index) fracture for each woman included in the analysis. As fractures could not be definitively confirmed to be fragility fractures as opposed to non-fragility fractures using the NPR, only fractures typically associated with osteoporosis were included; the fracture types and the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) codes are shown in Supplementary Table S1. Only clinically diagnosed and coded fractures were included in the analysis; therefore, it is likely that asymptomatic radiographic vertebral fractures were not captured. A main diagnosis of fracture was required for inclusion in the analysis and for the identification of new fractures. The following inclusion criteria were used to differentiate new fracture occurrences from existing fractures recorded at follow-up visits and/or from patient history: (a) when a fracture was registered in the outpatient and inpatient setting on the same day, only the inpatient record was counted; (b) for hip fractures, an inpatient hospital admission was required; (c) fractures at the same location in the body were required to have occurred at least 6 months apart and accompanied by a hospitalization; (d) fractures coded as M80 (osteoporosis with pathologic fracture) were counted only if they were a patient’s first fracture. As such, the M80 code for fracture was only used for the index fracture and not for identification of subsequent fractures. Fractures with a code of Z.094 (follow-up examination after fracture) were excluded.
The primary study endpoint was the cumulative incidence of subsequent fracture over 12 months following index fracture. Incidence of subsequent fracture over 24 months was also investigated. The risk of subsequent fracture from the time of the index fracture was estimated by index fracture type, i.e., any fracture, vertebral, hip, non-hip/non-vertebral (NH/NV), and MOF (i.e., vertebral, hip, humerus, or wrist). Independent risk factors for fracture were evaluated.
Data analysis
Cumulative fracture incidences at up to 12 months and 24 months were calculated taking the competing risk of death into account. The cumulative incidence function is preferred over a Kaplan-Meier estimate when competing events are present, as Kaplan-Meier estimates consider failures due to the competing event as censored, despite the competing event precluding failure from the event of interest altogether [36, 37]. A Kaplan-Meier estimate would therefore overestimate the true risk of fracture in the presence of competing risks.
Clinical and demographic factors associated with subsequent fracture risk were identified using multivariate competing risk regression, with fracture as the outcome and death as the competing event [38]. The variables included in the final multivariate model were age, index fracture type, and Charlson comorbidities. Osteoporosis treatment, glucocorticoid use, drugs associated with the risk of falls, and assisted drug dispensing (based on any filled prescription within 12 months before the index date) were also included in the multivariate model. The full list of variables considered for inclusion in the multivariate model is shown in Supplementary Table S2. Osteoporosis treatments included in the multivariate analysis were bisphosphonates, denosumab, strontium ranelate, raloxifene, and teriparatide (full list shown in Supplementary Table S3). Drugs delivered intravenously or subcutaneously may not have been included if they were dispensed through the hospital clinic and not by prescription. Drugs associated with increased risk of falls were defined using the listed medications from the Swedish National Board of Health and Welfare (Supplementary Table S4) [39] Glucocorticoid use was defined in the same way as in the FRAX algorithm, i.e., current exposure to oral glucocorticoids or previous exposure to oral glucocorticoids for > 3 months at a dose of prednisolone 5 mg daily or more (or equivalent doses of other glucocorticoids). Assisted drug dispensing was defined as use of the ApoDos system [40]. This is a system where medication is pre-packaged in small bags for morning, lunch, dinner, and evening. Use of the ApoDos system was implemented as a broad proxy for dependency, frailty, medication burden, and cognitive impairment.
Univariate analyses were performed for each of the potential risk factors individually to assess the influence of the risk factor on the risk of subsequent fracture. Sub-distribution hazard ratios (HR) with p values < 0.05 were considered statistically significant and were included in the multivariate model.
No imputation was required for missing data, as data were available for all risk factors used in the models.
Results
Patient characteristics at index date
Patient characteristics at the time of the index fracture are shown in Table 1. After excluding 31,896 women with either a diagnosis of Paget’s disease or a malignancy (other than basal cell carcinoma), a total of 242,108 women (mean [SD] age 74 [12.5] years) with an index fragility fracture were included in the analysis. The number and proportion of fracture types at index date were hip (51,904 [21.4%]), vertebral (15,065 [6.2%]), NH/NV (175,139 [72.3%]), and MOF (vertebral, hip, pelvis, humerus, forearm, or wrist; 156,253 [64.5%]). The number and proportion of women who had received osteoporosis treatment within the past 12 months was 25,860 (10.7%). The most frequent comorbidities were dementia (15,120 [6.3%]), diabetes without chronic complications (14,639 [6.1%]), and congestive heart failure (13,973 [5.8%]). Most women (173,138 [71.5%]) had received medications associated with increased risk of falls within the 12 months preceding the index fracture.
Incidence of subsequent fracture
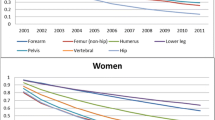
The number of subsequent fracture events within 12 months was 16,145 and within 24 months was 25,545. The overall cumulative subsequent fracture incidence at 12 months following any index fracture was 7.1% (95% confidence interval [CI], 6.9–7.2) and at 24 months was 12.0% (95% CI, 11.8–12.1; Fig. 1a). The rate of subsequent fractures was highest in the first month following fracture (~ 15 fractures per 1000 patient-years) and then remained consistently elevated between 4 and 24 months at ~ 5 fractures/1000 patient-years (Fig. 1b).
a Cumulative incidence of any subsequent fracture (clinically diagnosed and coded fractures only were counted) during the 24 months following any index fracture. b Rate of any subsequent fracture (clinically diagnosed and coded fractures only were counted) during the 24 months following any index fracture
A total of 20,811 deaths occurred within 12 months and 31,390 deaths within 24 months of the follow-up period. The numbers of competing events of death before subsequent fracture were 19,153 within 12 months and 27, 331 within 24 months.
Risk factors for subsequent fracture
Independent risk factors for subsequent fracture within 12 and 24 months, as identified by multivariate analysis, are shown in Table 2. Higher age was an independent risk factor for subsequent fracture within 12 and 24 months, notably with HRs > 2.0 in the 70–79 years age group and HRs > 3.0 in those aged ≥80 years compared with those aged 50–59 years (Table 2). Index vertebral fracture was a strong independent risk factor for imminent fracture risk relative to index hip fracture (HR, 2.72; p < 0.001). Similar results were seen for fractures within 24 months. Following NH/NV fracture, there was an increased risk of subsequent fracture within 12 and 24 months relative to hip fracture (at 12 months: HR, 1.29; p < 0.001, at 24 months: HR, 1.14; p < 0.001). Charlson comorbidity index scores of 1 and ≥ 2 were associated with an increased risk of subsequent fractures compared with an index score of 0 (Table 2). Use of assisted drug dispensing and osteoporosis medications was also associated with an increased risk of subsequent fracture. Despite taking into account the competing risk of death, comorbidities (cerebrovascular disease, congestive heart failure, dementia, diabetes without chronic complications, mild liver disease, renal disease, and rheumatic disease) were also predictors of subsequent fracture at 12 and 24 months (Supplementary Table S5).
Discussion
In this study, we report the incidence of a subsequent fracture within 1 and 2 years following initial fracture in women ≥ 50 years of age in Sweden by index fracture type. The highest risk of subsequent fractures was observed following a clinical vertebral fracture. In addition, we show that even when taking into account the competing risk of death, advancing age and comorbidities remain strong independent risk factors for imminent fracture. We also observed a high frequency of usage of medications known to increase fall risk in the year before the index fracture.
In the current study, the incidence of subsequent fractures within 12 months was 7.1%, increasing to 12.0% at 24 months. This is similar to a previous study of 4140 postmenopausal women performed in The Netherlands, where the absolute risk of any subsequent fracture in the year following first fracture was 6.1% [25]. Unlike the current study, the study undertaken in The Netherlands was a questionnaire study and relied on the proportion of patients who responded to the request to complete the questionnaire; this is likely to introduce bias, as patients who had suffered a new fracture could have been overrepresented in the responding group. In the current study, all women in Sweden ≥ 50 years of age with a fracture during the period of study were included, thus limiting sources of possible bias.
Our data are comparable with a US study of 377,561 women, which also employed a retrospective database design [26] and where the incidence of any subsequent fracture was 10% within 1 year of initial fracture. In our study, at 12 months, the incidence of subsequent fracture was highest following index clinical vertebral fracture (16.2%). This is also consistent with the US database study, where the subsequent fracture rate following index vertebral fracture was approximately 14% at 12 months [26]. In an earlier study of women with an index hip fracture, conducted in Sweden, 15% of women re-fractured within 1 year [42]. The proportion was lower in our study; 7.4% of women with index hip fracture went on to have a fracture within the following year. This difference in finding may be due to differences in sample size, patient demographic, and analysis methods. For example, the earlier Swedish study [42] comprised 766 adult women aged > 20 years compared with the 51,904 women (≥ 50 years) with index hip fracture in the current study. Further, in the study by von Friesendorff et al., a Kaplan-Meier estimate was used to quantify fracture risk, while in our study, a cumulative incidence function was used. As we took the competing risk of death into account, the cumulative incidence function will give a lower estimate than the Kaplan-Meier method if competing events are present.
In addition to the well-known elevated risk of fracture that follows a fragility fracture, we identified several independent risk factors for imminent fracture in this study. Age was an important factor; the HRs of age > 80 years compared with age 50–59 years were greater than 3.0. Age was also identified in other studies of risk factors for imminent fracture [23, 26, 43,44,45,46]. The risk of imminent fracture was doubled for every additional decade after age 50 years in a study of patients with no recent fracture [23]. A further study showed that incidence of subsequent fracture was higher with increasing age, with a HR of 1.2 per decade [44].
The risk factors identified in the current study are generally consistent with the risk factors included in the FRAX algorithm, i.e., age, rheumatic disease, and glucocorticoid use. However, we also identified other significant risk factors not included in FRAX, such as the use of a multi-dose drug dispensing service in the last 12 months, drugs that are associated with an increase in risk of falls, and specific comorbidities. Our data are consistent with the findings of the US Study of Osteoporotic Fractures (SOF), where independent predictors of any non-vertebral fracture within 1 year of follow-up included age, prior fracture, Parkinson’s disease or cerebrovascular disease, total hip T-score, prior falls, walking speed, and smoking [28]. However, in SOF, the 1-year follow-up period was not anchored to an index fragility fracture as in our study. Unlike the SOF study, in the current study, we did not capture data on falls, walking speed, or smoking status. In our study, the use of assisted drug dispensing was used as a broad proxy for dependency, frailty, medication burden, and functional and cognitive impairment, which we hypothesized would be associated with increased risk of fracture. Our findings were consistent with this hypothesis, as use of the ApoDos system was associated with a significantly increased risk of fracture.
We acknowledge that our study has some limitations. Diagnosis of fracture in this study was based on medical records, and we were not able to verify that all sustained fractures were associated with a low-trauma event. Therefore, it was not possible to make an absolute diagnosis of fragility fracture in all cases. Only ICD-10-coded clinical vertebral fractures were identified. Clinical vertebral fractures are a subset of all vertebral fractures; therefore, our numbers likely represent an underestimate of the true incidence and prevalence of vertebral fractures. While we acknowledge the limitations in the accuracy of fracture diagnoses, the diagnosis of hip fracture is expected to be more accurate than for vertebral fractures. Hip fractures were based on the ICD-10 code S72.x. Unlike previous studies [47, 48], we did not base the identification of hip fracture on the surgical procedure code as this would exclude women who (1) died shortly after hip fracture before undergoing surgery, (2) were too frail to undergo such a procedure and/or terminally ill, and (3) patients who were transferred elsewhere for the procedure. Still, our data are likely to underestimate the incidence of subsequent fractures. We observed a higher risk of subsequent fracture in patients using osteoporosis medications, which may be explained by a potential channeling bias; this has also been observed in previous studies [49]. A history of falls is a known strong predictor of imminent future fracture [23, 28]; data on falls were not available in our study. In addition, we examine data from a single country, and findings may not be transferable to other countries or populations. However, our study also has some major strengths. It is a large inclusive sample providing data on every diagnosed fracture in Sweden during the period of investigation. The Swedish social security number, which is unique for each citizen, allows for following patients over time and allows data to be linked to other registers, i.e., the PDR and the Cause of Death Register. In addition, minimal exclusion criteria were applied; therefore, it arguably provides a more representative depiction of events in a real-world clinical setting than that reported in smaller, more selective studies. Our study provides a comprehensive account of the incidence of subsequent fractures in women with a previous fracture and the risk factors associated with subsequent fractures; it does not, however, provide an estimate of the level of fracture risk compared with a control population.
In summary, there has been extensive research estimating fracture risk over a patient’s lifetime, but there is less evidence describing imminent fracture risk (within 12 and 24 months). Imminent risk of fragility fracture has been identified as an important area for further research [19, 24], provides an opportunity for rapid interventions to reduce future fracture events, and is key to the appropriate treatment of those patients at the highest risk of fracture. In such patients, to positively impact osteoporosis management, it is necessary to intervene with therapies proven to rapidly decrease fracture risk. Identifying individuals at imminent risk for fracture can be achieved through the recognition of associated risk factors, such as a recent fragility fracture and older age. In view of the current under treatment of patients at increased risk for fracture and in particular of those who have already suffered a fragility fracture, our findings highlight the need and the opportunity to put in place healthcare systems to intervene rapidly after a fracture, such as Fracture Liaison Services, or other forms of organized care intervention, linking orthopedic and emergency departments with doctors providing the longer term care of patients with fragility fractures. Indeed, the occurrence of a fragility fracture provides physicians and medical systems with a unique opportunity to act to reduce the risk of subsequent fractures.
References
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733. https://doi.org/10.1007/s00198-006-0172-4
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the international Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136. https://doi.org/10.1007/s11657-013-0136-1
Kanis JA, Johnell O, Oden A, Sembo I, Redlund-Johnell I, Dawson A, De Laet C, Jonsson B (2000) Long-term risk of osteoporotic fracture in Malmö. Osteoporosis Int 11:669–674. https://doi.org/10.1007/s001980070064
Svedbom A, Hernlund E, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA, EU Review Panel of IOF (2013) Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos 8:137. https://doi.org/10.1007/s11657-013-0137-0
Bentler SE, Liu L, Obrizan M, Cook EA, Wright KB, Geweke JF, Chrischilles EA, Pavlik CE, Wallace RB, Ohsfeldt RL, Jones MP, Rosenthal GE, Wolinsky FD (2009) The aftermath of hip fracture: discharge placement, functional status change, and mortality. Am J Epidemiol 170:1290–1299. https://doi.org/10.1093/aje/kwp266
Leibsen CL, Tosteson AN, Gabriel SE, Ransom JE, Melton LJ (2002) Mortality, disability, and nursing home use for persons with and without hip fracture: a population-based study. J Am Geriat Soc 50:1644–1650. https://doi.org/10.1046/j.1532-5415.2002.50455.x
International Osteoporosis Foundation (2012) Capture the Fracture Report 2012. https://www.iofbonehealth.org/capture-fracture-report-2012. Accessed 27 July 2018
Bliuc D, Alarkawi D, Nguyen TV, Eisman JA, Center JR (2015) Risk of subsequent fractures and mortality in elderly women and men with fragility fractures with and without osteoporotic bone density: the Dubbo osteoporosis epidemiology study. J Bone Miner Res 30:637–646. https://doi.org/10.1002/jbmr.2393
Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR (1999) Vertebral fractures and mortality in older women: a prospective study. Study of osteoporotic fractures research group. Arch Intern Med 159:1215–1220. https://doi.org/10.1001/archinte.159.11.1215
Katsoulis M, Benetou V, Karapetyan T, Feskanich D, Grodstein F, Pettersson-Kymmer U, Eriksson S, Wilsgaard T, Jørgensen L, Ahmed LA, Schöttker B, Brenner H, Bellavia A, Wolk A, Kubinova R, Stegeman B, Bobak M, Boffetta P, Trichopoulou A (2017) Excess mortality after hip fracture in elderly persons from Europe and the USA: the CHANCES project. J Intern Med 281:300–310. https://doi.org/10.1111/joim.12586
Klop C, van Staa T, Cooper C, Harvey N, de Vries F (2017) The epidemiology of mortality after fracture in England: variation by age, sex, time, geographic location, and ethnicity. Osteoporos Int 28:161–168. https://doi.org/10.1007/s00198-016-3787-0
von Friesendorff M, McGuigan FE, Wizert A, Rogmark C, Holmberg AH, Woolf AD, Akesson K (2016) Hip fracture, mortality risk, and cause of death over two decades. Osteoporos Int 27:2945–2953. https://doi.org/10.1007/s00198-016-3616-5
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R, National Osteoporosis Foundation (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25:2359–2381. https://doi.org/10.1007/s00198-014-2794-2
Black DM, Arden NK, Palermo L, Pearson J, Cummings SR (1999) Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of osteoporotic fractures research group. J Bone Miner Res 14:821–828. https://doi.org/10.1359/jbmr.1999.14.5.821
Eisman JA, Bogoch ER, Dell R, Harrington JT, McKinney RE Jr, McLellan A, Mitchell PJ, Silverman S, Singleton R, Siris E, ASBMR task force on secondary fracture prevention (2012) Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res 27:2039–2046. https://doi.org/10.1002/jbmr.1698
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359:1929–1936. https://doi.org/10.1016/S0140-6736(02)08761-5
Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, Eisman J, Fujiwara S, Garnero P, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35:375–382. https://doi.org/10.1016/j.bone.2004.03.024
Kloetzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739. https://doi.org/10.1359/jbmr.2000.15.4.721
Roux C, Briot K (2017) Imminent fracture risk. Osteoporos Int 28:1765–1769. https://doi.org/10.1007/s00198-017-3976-5
Van Geel TACM, Huntjens KM, van den Bergh JP, Dinant GJ, Geusens PP (2010) Timing of subsequent fractures after an initial fracture. Curr Osteoporos Rep 8:118–122. https://doi.org/10.1007/s11914-010-0023-2
Johansson H, Siggeirsdóttir K, Harvey NC, Odén A, Gudnason V, McCloskey E, Sigurdsson G, Kanis JA (2017) Imminent risk of fracture after fracture. Osteoporos Int 28:775–780. https://doi.org/10.1007/s00198-016-3868-0
McLellan AR, Reid DM, Forbes K, Reid R, Campbell C, Gregori A, Raby N, Simpson A (2004) Effectiveness of strategies for the secondary prevention of osteoporotic fractures in Scotland. http://www.healthcareimprovementscotland.org/previous_resources/audit_report/osteoporotic_fractures_audit.aspx. Accessed 27 July 2018
Bonafede M, Shi N, Barron R, Li X, Crittenden DB, Chandler D (2016) Predicting imminent risk for fracture in patients aged 50 or older with osteoporosis using US claims data. Arch Osteoporos 11:26. https://doi.org/10.1007/s11657-016-0280-5
Kanis JA, Cooper C, Rizzoli R, Abrahamsen B, Al-Daghri NM, Brandi ML, Cannata-Andia J, Cortet B, Dimai HP, Ferrari S, Hadji P, Harvey NC, Kraenzlin M, Kurth A, McCloskey E, Minisola S, Thomas T, Reginster JY, European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) (2017) Identification and management of patients at increased risk of osteoporotic fracture: outcomes of an ESCEO expert consensus meeting. Osteoporos Int 28:2023–2034. https://doi.org/10.1007/s00198-017-4009-0
Van Geel TACM, van Helden S, Geusens PP, Winkens B, Dinant GJ (2009) Clinical subsequent fractures cluster in time after first fractures. Ann Rheum Dis 68:99–102. https://doi.org/10.1136/ard.2008.092775
Balasubramanian A, Zhang J, Chen L, Wenkert D, Daigle SG, Grauer A, Curtis JR (2016) High risk of second fracture within 1, 2, 5 years after prior fracture among women 65 years or older. J Bone Miner Res 31(Suppl 1):S93 Abstract FR02033
Johnell O, Kanis JA, Odén A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jönsson B (2004) Mortality after osteoporotic fractures. Osteoporos Int 15:38–42. https://doi.org/10.1007/s00198-003-1490-4
Weycker D, Edelsberg J, Barron R, Atwood M, Oster G, Crittenden DB, Grauer A (2017) Predictors of near-term fracture in osteoporotic women aged ≥65 years, based on data from the study of osteoporotic fractures. Osteoporos Int 28:2565–2571. https://doi.org/10.1007/s00198-017-4103-3
University of Sheffield. FRAX®: fracture risk assessment tool. https://www.sheffield.ac.uk/FRAX/tool.jsp. Accessed 27 July 2018
GARVAN Institute. Fracture risk calculator. https://www.garvan.org.au/promotions/bone-fracture-risk/calculator/. Accessed 27 July 2018
QFracture. QFracture®-2016 risk calculator. http://www.qfracture.org/. Accessed 27 July 2018
Kanis JA, Harvey NC, Cooper C, Johansson H, Odén A, Mccloskey EV, Advisory Board of the National Osteoporosis Guideline Group (2016) A systematic review of intervention thresholds based on FRAX: a report prepared for the National Osteoporosis Guideline Group and the international Osteoporosis Foundation. Arch Osteoporos 11:25. https://doi.org/10.1007/s11657-016-0278-z
Leslie WD, Majumdar SR, Morin SN, Lix LM, Johansson H, Oden A, McCloskey EV, Kanis JA (2017) FRAX for fracture prediction shorter and longer than 10 years: the Manitoba BMD registry. Osteoporos Int 28:2557–2564. https://doi.org/10.1007/s00198-017-4091-3
Feldstein A, Elmer PJ, Orwoll E, Herson M, Hillier T (2003) Bone mineral density measurement and treatment for osteoporosis in older individuals with fractures: a gap in evidence-based practice guideline implementation. Arch Intern Med 163:2165–2172. https://doi.org/10.1001/archinte.163.18.2165.
Siris ES, Adler R, Bilezikian J, Bolognese M, Dawson-Hughes B, Favus MJ, Harris ST, Jan de Beur SM, Khosla S, Lane NE, Lindsay R, Nana AD, Orwoll ES, Saag K, Silverman S, Watts NB (2014) The clinical diagnosis of osteoporosis: a position statement from the National Bone Health Alliance Working Group. Osteoporos Int 25:1439–1443. https://doi.org/10.1007/s00198-014-2655-z
Klein JP, Rizzo JD, Zhang MJ, Keiding N (2001) Statistical methods for the analysis and presentation of the results of bone marrow transplants. Part I: unadjusted analysis. Bone Marrow Transplant 28:909–915
Andersen PK, Geskus RB, de Witte T, Putter H (2012) Competing risks in epidemiology: possibilities and pitfalls. Int J Epidemiol 41:861–870
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496–509. https://doi.org/10.1080/01621459.1999.10474144
Socialstyrelsen. Indikatorer för god läkemedelsterapi hos äldre. https://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/18085/2010-6-29.pdf. Accessed 21 November 2018
Apoteket. ApoDos—simple and safe. https://www.apoteket.se/vard-foretag/apodos/. Accessed 27 July 2018
Landfeldt E, Ström O, Robbins S, Borgström F (2012) Adherence to treatment of primary osteoporosis and its association to fractures—the Swedish adherence register analysis (SARA). Osteoporos Int 23:433–443
von Friesendorff M, Besjakov J, Akesson K (2008) Long-term survival and fracture risk after hip fracture: a 22-year follow-up in women. J Bone Miner Res 23:1832–1841. https://doi.org/10.1359/jbmr.080606
Ahmed LA, Center JR, Bjørnerem A, Bluic D, Joakimsen RM, Jørgensen L, Meyer HE, Nguyen ND, Nguyen TV, Omsland TK, Størmer J, Tell GS, van Geel TA, Eisman JA, Emaus N (2013) Progressively increasing fracture risk with advancing age after initial incident fragility fracture: the Tromsø study. J Bone Miner Res 28:2214–2221. https://doi.org/10.1002/jbmr.1952
Van Helden S, Cals J, Kessels F, Brink P, Dinant GJ, Geusens P (2006) Risk of new clinical fractures within 2 years following a fracture. Osteoporos Int 17:348–354. https://doi.org/10.1007/s00198-005-2026-x
Yusuf A, Hu Y, Chandler D, Crittenden B, Barron R (2016) Characteristics of patients at high one-year fracture risk. J Bone Miner Res 31(Suppl 1):S363 Abstract MO0223
Yusuf A, Hu Y, Chandler D, Crittenden B, Barron R (2016) Predictors of imminent fracture risk in Medicare-enrolled men and women. J Bone Miner Res 31(Suppl 1):S246 Abstract SU0227
Vu T, Davie G, Barson D, Day L, Finch CF (2013) Accuracy of evidence-based criteria for identifying an incident hip fracture in the absence of the date of injury: a retrospective database study. BMJ Open 3. https://doi.org/10.1136/bmjopen-2013-003222
Rosengren BE, Ahlborg HG, Mellström D, Nilsson JÅ, Björk J, Karlsson MK (2012) Secular trends in Swedish hip fractures 1987–2002: birth cohort and period effects. Epidemiology 23:623–630
Yusuf AA, Hu Y, Chandler D, Crittenden B, Barron R (2016) Characteristics of patients at high one-year fracture risk ASBMR Annual Meeting: SU0227
Acknowledgments
Medical writing support, in the form of development of the draft outline and manuscript first draft in consultation with the authors, editorial suggestions to draft versions of this manuscript, assembling tables and figures, collating author comments, copyediting, referencing, and graphic services was provided by Angela Rogers, PhD, CMPP™, of Gardiner-Caldwell Communications (an Ashfield company, part of UDG Healthcare plc), Macclesfield, UK, and funded by UCB Pharma.
Funding
This study was funded by UCB Pharma. Medical writing and editorial support in the preparation of this manuscript was funded by UCB Pharma.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study has been approved by the Regional Ethical Review Board in Stockholm and performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments. For this type of study, individual formal consent was not required.
Conflicts of interest
JB, LK, OS, and GO are employed by Quantify Research, and Quantify Research was funded by UCB Pharma to conduct this study.
KEA has received lecture fees from Merck, UCB Pharma, Eli Lilly, Amgen, and Novartis.
AS has received lecture fees from Amgen and Eli Lilly.
OL has received lecture fees from Eli Lilly and Amgen.
CL and ET are employed by, and own stocks in, UCB Pharma.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
OpenAccess This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Banefelt, J., Åkesson, K., Spångéus, A. et al. Risk of imminent fracture following a previous fracture in a Swedish database study. Osteoporos Int 30, 601–609 (2019). https://doi.org/10.1007/s00198-019-04852-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-04852-8