Abstract
Summary
In the first year, after an osteoporotic fracture of a hip, forearm, upper arm, or spine, the dispensing rates of antidepressants and benzodiazepines increased significantly. After those fractures, recent and past use of antidepressants and benzodiazepines was associated with increased all-cause mortality; current use was not associated with mortality risk.
Introduction
It remains unclear to what extent use of antidepressants and benzodiazepines is associated with mortality risk after a major osteoporotic fracture (MOF). We aimed to study the cumulative use of antidepressants and benzodiazepines during the year after MOF or hip fracture (HF) and whether the use was associated with mortality.
Methods
A cohort study was performed within the Dutch PHARMO Database Network including all patients aged 65+ with a first record of MOF (hip, humerus, forearm, and clinical vertebral fracture) between 2002 and 2011. Data were analyzed using Cox regression models, adjusted for comorbidities, and concomitant medication use and broken down to index fracture type.
Results
A total of 4854 patients sustained a first MOF, of whom 1766 patients sustained a HF. Mean follow-up was 4.6 years, divided in 30-day periods. The cumulative antidepressant and benzodiazepine use during the first year after MOF increased from 10.6 to 14.7% and from 24.0 to 31.4%, respectively. Recent (31–92 days before each follow-up period) and past use (> 92 days before) of antidepressants and benzodiazepines after MOF or HF was associated with an increased all-cause mortality risk but current use (< 30 days before) was not.
Conclusion
There is a considerable increase in dispensing rate of antidepressants and benzodiazepines in the first year after a MOF. Recent and past use of these medications was associated with all-cause mortality. The finding that current use was not associated with mortality should be further explored and may probably be explained by the healthy survivor’s bias.
Similar content being viewed by others
Introduction
In 2000, it was estimated that worldwide 9 million new fragility fractures occurred of which 5.4 million were major osteoporotic fractures (MOF: hip, forearm, spine, and humerus) [1]. It has been estimated that due to aging of the population, the fracture incidence of osteoporotic fractures in the period of 2010 to 2030 will increase with 40% in the Netherlands [2]. Besides resulting co-morbidities, patients with osteoporotic fractures have an increased risk of subsequent fracture and an increased mortality [3, 4].
The reasons for increased mortality in fracture patients are diverse, and the use of antidepressants and benzodiazepines is possibly one of the reasons. Psychotropic drugs such as antidepressants and benzodiazepines are frequently prescribed in elderly [5, 6], in patients with a recent clinical fracture presenting at a fracture liaison service (FLS) [7], and in patients with a hip fracture (HF) [8,9,10]. Both antidepressants and benzodiazepines have been associated with mortality [11,12,13,14,15,16]. The risk of mortality with antidepressant use may be the result of an increased risk of cardiac arrhythmias [17], while in benzodiazepine users, upper airway collapse and negative effects on respiration are described as possible mechanisms of the increased mortality risk [18, 19]. However, epidemiological studies showed inconsistent results when studying the association between use of antidepressants or benzodiazepines and all-cause mortality [11,12,13,14,15,16, 20,21,22,23,24,25].
Many studies have assessed the association of fracture risk with use of benzodiazepines and antidepressants in the general population [26,27,28]. Only few studies assessed the mortality risk with use of antidepressants and benzodiazepines after a HF but not after other osteoporotic fracture types [9, 29]. Kragh et al. reported a significantly higher first year mortality in older hip fracture in patients exposed before the fracture to psychotropic drugs [29].
It remains unclear to which extent use of antidepressants and benzodiazepines is associated with mortality risk in the, already high-risk, post-fracture period in patients with a MOF. Therefore, the aims of this study were (1) to describe the frequency of dispensing of antidepressants and benzodiazepines in the first year after HF or MOF, and (2) to describe the association between use of these drugs and risk of all-cause mortality.
Methods
Data source
The design and methods of our study were comparable to the recently published study of van de Ven et al. [30]. Between 2002 and 2011, a cohort study was performed within the Dutch PHARMO Database Network (Institute for Drug Outcome Research, www.pharmo.nl). This population-based network of probabilistically linked electronic healthcare databases contains data from multiple primary and secondary healthcare settings. For the current study, primary care data linked to outpatient pharmacy dispensing data, hospitalizations from the Dutch Hospital Data Foundation (DHD, www.dutchhospitaldata.nl), and death registration data for approximately 660,000 community-dwelling individuals in the Netherlands was used. Primary care diagnoses are coded according to International Classification of Primary Care (ICPC) codes. Drug-dispensing records contain information concerning the dispensed drug according to the Anatomical Therapeutic Chemical (ATC) Classification system codes including amount, dose, dosage regimen, and date of dispensing [31]. Hospital records include dates of inpatient admissions and discharge, diagnoses, and procedures recorded according to the International Classification of Disease, 9th or 10th revision codes (ICD-9-CM or ICD-10). A high validity of hip fracture recording has been shown previously in the PHARMO Database Network with a true positive rate > 90% [32].
Study population
All patients aged 65 years or older with a first record of a fracture of either the hip, forearm, humerus, or spine that came to clinical attention since start of data collection were included. Fractures were classified into the following categories using ICPC, ICD-9-CM, and ICD-10 codes: hip (ICPC: L75.01, ICD-9-CM: 820, ICD-10: S72.0, S72.1, S72.2), forearm (ICPC: L72, ICD-9-CM: 813, 814, ICD-10: S52), clinical spine (ICPC: L76.06, ICD-9-CM: 805, 806, ICD-10: S12.0-S12.2, S12.7, S22.0, S22.1, S32.0-S32.2), and humerus (ICPC: L74.04, ICD-9-CM: 812, ICD-10: S42.2-S42.4, S42.7). Fractures were identified from primary care records and hospitalization data between 1 January 2002 and 31 December 2011. The date of the first fracture defined the index date. All patients were required to have at least 1 year of valid data collection before their index date.
Definition of exposure
Oral use of antidepressants and benzodiazepines was determined using pharmacy dispensing data. The following ATC codes were included: antidepressants: N06A. These included tricyclic antidepressants [TCAs] N06AA, SSRIs, N06AB and others: N06AF, N06AG, and N06AX. We also included benzodiazepines (ATC codes N05BA, N05CD, or N05CF). Use of these drugs was defined in a time-dependent manner. Follow-up was divided in 30-day periods. Presence of a dispensing for an antidepressant and/or benzodiazepine was determined before each interval. Current users were patients who had a record in the 30-day period before each interval. Recent users were those with a record between 31 days and 92 days before each interval. Past users were those who had a record > 92 days before the interval. Patients could move between current, recent, and past exposure throughout follow-up. Patients who were not dispensed an antidepressant or benzodiazepine were classified as non-users. At each current use interval, the cumulative dose was calculated by adding the amount of dispensed defined daily dosages (DDDs) [31] of all dispensings before that interval. The cumulative dose of benzodiazepines was expressed in milligram temazepam equivalents and the cumulative dose of antidepressants in milligram paroxetine equivalents.
All patients were followed from the index date until the occurrence of all-cause mortality, migration out of the data source, or the end of the study period (31 December 2011 the latest), whichever came first. The date of death was the earliest date that was recorded wither in general practice, hospital, or national death certificates.
Potential confounders
Potential confounders for this study were determinants that have been associated with mortality risk. With the exception of sex, they were assessed in a time-dependent manner and included age, and a history of chronic diseases (ischemic heart disease, cerebrovascular disease, congestive heart failure, chronic kidney disease, chronic obstructive pulmonary disease (COPD), dementia), malignant neoplasms, or depression. Other potential confounders included a dispensing for anticonvulsants, antipsychotics, lithium, glucocorticoids, anti-arrhythmic drugs, NSAIDs, β-blockers, thiazide diuretics, loop diuretics, renin-angiotensin-aldosterone system (RAAS) inhibitors, statins, anti-diabetic drugs, and anti-rheumatic drugs in the 6 months before the start of an interval.
Statistical analysis
Kaplan–Meier analyses (1, Kaplan–Meier estimate) were used to estimate cumulative incidence rates of all-cause mortality after MOF or specifically hip fracture, broken down by current use of antidepressants, benzodiazepines, or concomitant use of both classes of drugs. Cox proportional hazards regression was used to estimate the risk of all-cause mortality with use of antidepressants and/or benzodiazepines versus non-use (PHREG procedure, SAS 9.4; SAS Institute). Current use of benzodiazepines and antidepressants was further stratified by cumulative dose categories. Potential confounders were included into the final model if they independently changed the β-coefficient for the exposure (antidepressants, benzodiazepines) by at least 5% (change-in-estimate method [33]). Risk of mortality was assessed by the time since the most recent dispensing of either an antidepressant or benzodiazepine.
Results
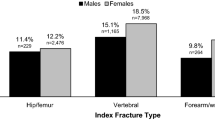
Between 2002 and 2011, a total number of 4854 patients sustained a MOF after the age of 65 years, of whom 1766 patients sustained a HF. In the group of patients with a MOF, 78.1% were women and their mean age was 78 years (standard deviation (SD) = 7.5 years). In the subgroup of patients with a HF, 72.6% were women and they had a mean age of 81 years (SD = 7.4 years). The mean duration of follow-up in the group of patients with a MOF was 4.6 years (SD = 2.2 years) and in the group of patients with a HF 4.6 years (SD 2.3 = years).
As presented in Table 1, patients in both groups had a history of several of the selected comorbidities; peptic ulcer and dyspepsia, ischemic heart disease, and cerebrovascular diseases were the most common selected comorbidities before the index date. A history of depression was less frequent in patients with a MOF (4.3%) versus the patients in the subgroup with a HF (4.8%), whereas the proportions of previous antidepressant use in the past 6 months prior to fracture were considerably higher: 12.7% among those who had sustained a MOF and 14.5% for the subgroup with a HF. More than 25% of all patients with a MOF or HF had used benzodiazepines in the past 6 months prior to fracture.
In Table 2, the cumulative incidence of antidepressant, benzodiazepine, or combined use in the first year following fracture is presented. The cumulative incidence after a MOF increased from 10.6% (95% CI 9.8–11.6) to 14.7% (95% CI 13.7–15.7) for antidepressant use, from 24.0% (95% CI 22.8–25.3) to 31.4% (95% CI 30.1–32.8) for benzodiazepine use, and from 5.4% (95% CI 4.8–6.0) to 8.2% (95% CI: 7.5–9.1) for concomitant use of antidepressants and benzodiazepines. During the first year after a HF, the cumulative incidence of antidepressant use increased from 10.9% (95% CI 9.5–12.5) to 16.0% (95% CI 14.3–17.9) and the cumulative incidence of benzodiazepine use increased from 27.8% (95% CI 25.7–30.0) to 35.7% (95% CI 33.4–38.1).
During the total follow-up period, current use of antidepressants, benzodiazepines, or both after a MOF or HF was not associated with risk of all-cause mortality (Table 3). However, recent use of antidepressants, benzodiazepines, or both was associated with an increased all-cause mortality risk after MOF (adjusted HR of 1.38 (95% CI 1.01–1.90) for antidepressants, adjusted HR of 1.47 (95% CI 1.14–1.89) for benzodiazepines, and adjusted HR of 2.37 (95% CI 1.39–4.06) for combined use. Past use of antidepressants, benzodiazepines, or both was also associated with all-cause mortality risk; adjusted HR of 1.39 (95% CI 1.15–1.66) for antidepressants, adjusted HR of 1.20 (95% CI 1.02–1.42) for benzodiazepines, and adjusted HR of 1.58 (95% CI 1.25–2.00) for combined use.
Stratification of current use by cumulative dose did not demonstrate a significant difference in mortality risk in the different cumulative dosage groups in antidepressants. In benzodiazepines, only the lowest cumulative dose had an elevated all-cause mortality after MOF, adjusted HR of 1.40 (95% CI 1.06–1.85). Higher cumulative dosages of benzodiazepines were not associated with all-cause mortality.
As shown in Table 3, compared to the all-cause mortality after a MOF, recent and past use of antidepressants, benzodiazepines, or combined use after a HF resulted in a comparable risk of all-cause mortality.
Discussion
This study demonstrates that the proportion of patients who had received at least one dispensing of antidepressants or benzodiazepines increased during the first year following a MOF; this was also shown for the subgroup of patients with a HF. Furthermore, this study showed no association between the current use of antidepressants or benzodiazepines and risk of all-cause mortality during a 4.6-year follow-up period after a MOF or a HF. However, risk of all-cause mortality was higher for recent and past use of any of both classes of medication.
The use of antidepressants and benzodiazepines in the period before and after a HF in our cohort is different compared to other studies. In our study, 14.5% and 28.1% of the patients used antidepressants and benzodiazepines, respectively, in the 6 months before the HF. The cumulative incidence of antidepressant or benzodiazepine use 3 months after a HF was 10.9% and 27.8%, respectively. This increased to 16.0% and 35.7% 1 year after the HF, respectively. After a MOF, the proportions of benzodiazepine and antidepressant users were slightly lower compared to the subgroup of patients who sustained a HF. Our results are not in line with those by Iaboni et al., who showed an initiation rate of 8.8% of antidepressants in the first 90 days after a hip fracture in the cohort of community-dwelling elderly who had not been exposed to an antidepressant in the year prior to the fracture [8]. The dispensing rate increased over a period of time, with 10.4% as highest initiation rate [8]. These initiation rates are higher compared to our study. Kragh et al. [10] reported that 21.5% and 20.1% of the patients used antidepressants and benzodiazepines in the 6 months before a hip fracture, respectively. After a hip fracture, these proportions increased to 31.8% and 28.1%, respectively. The study of Kragh et al. [10] showed a substantial use of antidepressants and benzodiazepines but a higher rate of antidepressant use and a lower rate of benzodiazepine use compared to our study. There are several differences which may explain the different outcomes. In our cohort, the cumulative incidence was studied, in the Swedish cohort of Kragh et al. the incidence, and in the study of Iaboni et al. the initiation rate was studied and there were different time windows [8, 10]. Besides that, in our cohort and in the cohort of Kragh et al. [10], patients had received dispensings of antidepressants in the year before the fracture. Further, the habits of prescribing certain drugs in a country may also contribute to the differences. A potential explanation for the high incidence rate of antidepressants and benzodiazepines after a HF may be that depression was reported to be associated with adverse effects on rehabilitation participation and recovery from hip fractures [34].
In the cohort of patients with a MOF or HF we found an association between recent and past use of antidepressant or benzodiazepines and all-cause mortality but not for current use of antidepressants and benzodiazepines. Several previous studies reported that the use of antidepressants and benzodiazepines was associated with an increased risk of mortality [11,12,13,14,15,16], but other observational studies did not find increased mortality risk with the use of antidepressants and benzodiazepines [20,21,22,23,24,25]. Panula et al. studied in a Finnish hip fracture cohort the use of potent anticholinergics, sedatives and antipsychotics at the time of the hip fracture and the association with postoperative mortality [9]. Only in men the age-adjusted mortality after 30 days, 3 months, 6 months, and 3 years was increased with the use of potent anticholinergics. Furthermore, the mortality after 3 years in men using sedatives and antipsychotics at the time of the hip fracture was higher compared to men not taking sedatives and antipsychotics. In the Finnish hip cohort medication at the time of the HF was checked. It is unclear how many patients continued to use the medications the years after the HF [9]. Therefore, it is difficult to conclude whether the association is due to medication use or comorbidity.
Since we found an increased mortality risk with recent and past antidepressant and benzodiazepine use, i.e., opposite of a causal hypothesis, these effects are unlikely to be explained by direct pharmacological action but rather by unknown distortion. The absence of a dose–response effect in the analysis with the cumulative doses in current use confirms this. An excess mortality risk is demonstrated in the first year after a HF [35]. One of the possible explanations for the excess mortality risk after a HF is cardiac disease [36]. Cameron et al. demonstrated that the number of deaths due to arrhythmias was elevated in the first 3 months after a hip fracture [36]. The use of antidepressants and benzodiazepines may increase mortality risk via cardiac arrhythmias [17] or upper airway collapse [18, 19], respectively. Those effects of antidepressants and benzodiazepines are more likely to occur in the first period after starting the drugs and given the relatively short half-life of most agents, these effects should only last a few days after discontinuation. We found no increased mortality risk with current use of antidepressants and benzodiazepines, only with recent and past use. Therefore, we cannot explain the effects by direct pharmacological action. In previous research, it was reported that good adherence is associated with a decreased mortality [37, 38], while other studies report that poor adherence is associated with an increased mortality risk ([39]. However, in our study, data regarding persistence and reasons or causes of stopping the antidepressants or benzodiazepines were not available. Therefore, we were unable to analyze the effect of adherence on mortality.
We postulate that there might be an effect of the healthy survival [40, 41]. In 2008, a first version of the STOPP/START criteria for potentially inappropriate prescribing in older people were developed [41]. Further, the updated Beers criteria of 2012 stated that the use of benzodiazepines in elderly should be avoided and that antidepressants (SSRIs, TCAs) should be used with caution [42]. There are several guidelines developed to help reviewing medication and to stop medication in elderly [43, 44]. These reviews are especially developed for the frail elderly. According to the Dutch general practitioners’ guideline for medication review: patients aged > 65 year, using 5 or more medications, and with at least 1 risk factor (eGFR < 50 ml/min/1.73 m2, impaired cognitive function, increased risk of falling, signs of reduced compliance, living in a nursing home, unplanned hospitalization) have an indication for an extensive medication review [44]. Hence, stopping or diminishing use of antidepressants or benzodiazepines among other medications might be especially applied in elderly patients of this Dutch PHARMO cohort with polypharmacy indicating at a worse prognosis of these patients. This may have resulted in the finding of increased risk of all-cause mortality with recent and past but not current use of these medications in the present study.
This study has several strengths and limitations. First, dispensing and not prescription data was used to evaluate the use of antidepressants and benzodiazepines. As compared to prescription data, dispensing data is more reliable and will result in less misclassification of exposure as compared to prescription data. However, it remains unknown if patients have been compliant with their dispensings and this may have resulted in a dilution of the effect. Second, we used real-life data and we had longitudinal information on drug dispensings. Third, we were able to adjust our analyses for several confounders, including comorbidities and concomitant drug use. However, a limitation is that we did not have information on lifestyle factors, such as smoking and body mass index (BMI). It is known that patients with a psychiatric disease smoke more often than people without a psychiatric disease [45], and smoking has been associated with an increased risk of mortality [46]. Therefore, not adjusting for smoking may result in an artificial association between use of benzodiazepines or antidepressants and mortality risk. However, we did not find such an association. Use of benzodiazepines and antidepressants has been association with weight gain [47, 48]. A higher BMI has been associated with an increased risk of mortality [49]. Not adjusting for BMI would have resulted in an artificial association when users of antidepressants or benzodiazepines had a higher BMI as compared to never users. However, we did not find such an association. Fifth, the date of death but not the cause of death was available from the linkage of the Central Bureau of Genealogy we used in this study.
In conclusion, this study demonstrates a considerable increase in dispensing rate of antidepressants and benzodiazepines in the first year after a MOF. Furthermore, this study showed that recent and past use of antidepressants or benzodiazepines was significantly associated with all-cause mortality. We found no association between current use of antidepressants or benzodiazepines and mortality after MOF, but we postulate that this may probably be explained by the healthy survivor’s bias. We would like to emphasize that it is important to focus on the drug use of the frail patients after a recent MOF and to follow the current guidelines concerning stopping and starting drugs especially with regard to use of antidepressants or benzodiazepines.
References
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733. https://doi.org/10.1007/s00198-006-0172-4
Lötters FJB, van den Bergh JP, de Vries F, Rutten-van Mölken MPMH (2016) Current and future incidence and costs of osteoporosis-related fractures in the Netherlands: combining claims data with BMD measurements. Calcif Tissue Int 98:235–243. https://doi.org/10.1007/s00223-015-0089-z
Bliuc D, Alarkawi D, Nguyen TV, Eisman JA, Center JR (2015) Risk of subsequent fractures and mortality in elderly women and men with fragility fractures with and without osteoporotic bone density: the Dubbo osteoporosis epidemiology study. J Bone Miner Res 30:637–646. https://doi.org/10.1002/jbmr.2393
Tran T, Bliuc D, van Geel T, Adachi JD, Berger C, van den Bergh J, Eisman JA, Geusens P, Goltzman D, Hanley DA, Josse RG, Kaiser SM, Kovacs CS, Langsetmo L, Prior JC, Nguyen TV, Center JR (2017) Population-wide impact of non-hip non-vertebral fractures on mortality. J Bone Miner Res 32:1802–1810. https://doi.org/10.1002/jbmr.3118
Egan M, Moride Y, Wolfson C, Monette J (2000) Long-term continuous use of benzodiazepines by older adults in Quebec: prevalence, incidence and risk factors. J Am Geriatr Soc 48:811–816
Karkare SU, Bhattacharjee S, Kamble P, Aparasu R (2011) Prevalence and predictors of antidepressant prescribing in nursing home residents in the United States. Am J Geriatr Pharmacother 9:109–119. https://doi.org/10.1016/j.amjopharm.2011.03.001
Vranken L, Wyers CE, van der Velde RY, Janzing HM, Kaarsemaker S, Geusens PP, van den Bergh JP (2018) Comorbidities and medication use in patients with a recent clinical fracture at the fracture liaison service. Osteoporos Int 29:397–407. https://doi.org/10.1007/s00198-017-4290-y
Iaboni A, Seitz DP, Fischer HD, Diong CC, Rochon PA, Flint AJ (2015) Initiation of antidepressant medication after hip fracture in community-dwelling older adults. Am J Geriatr Psychiatry 23:1007–1015. https://doi.org/10.1016/j.jagp.2014.10.002
Panula J, Puustinen J, Jaatinen P, Vahlberg T, Aarnio P, Kivela SL (2009) Effects of potent anticholinergics, sedatives and antipsychotics on postoperative mortality in elderly patients with hip fracture: a retrospective, population-based study. Drugs Aging 26:963–971. https://doi.org/10.2165/11317660-000000000-00000
Kragh A, Elmståhl S, Atroshi I (2011) Older adults' medication use 6 months before and after hip fracture: a population-based cohort study. J Am Geriatr Soc 59:863–868. https://doi.org/10.1111/j.1532-5415.2011.03372.x
Coupland C, Dhiman P, Morriss R, Arthur A, Barton G, Hippisley-Cox J (2011) Antidepressant use and risk of adverse outcomes in older people: population based cohort study. BMJ 343:d4551–d4551. https://doi.org/10.1136/bmj.d4551
Hansen RA, Khodneva Y, Glasser SP, Qian J, Redmond N, Safford MM (2016) Antidepressant medication use and its association with cardiovascular disease and all-cause mortality in the reasons for geographic and racial differences in stroke (REGARDS) study. Ann Pharmacother 50:253–261. https://doi.org/10.1177/1060028015625284
Smoller JW, Allison M, Cochrane BB et al (2009) Antidepressant use and risk of incident cardiovascular morbidity and mortality among postmenopausal women in the Women's Health Initiative study. Arch Intern Med 169:2128–2139. https://doi.org/10.1001/archinternmed.2009.436
Jennum P, Baandrup L, Ibsen R, Kjellberg J (2015) Increased all-cause mortality with use of psychotropic medication in dementia patients and controls: a population-based register study. Eur Neuropsychopharmacol 25:1906–1913. https://doi.org/10.1016/j.euroneuro.2015.08.014
Mallon L, Broman J-E, Hetta J (2009) Is usage of hypnotics associated with mortality? Sleep Med 10:279–286. https://doi.org/10.1016/j.sleep.2008.12.004
Palmaro A, Dupouy J, Lapeyre-Mestre M (2015) Benzodiazepines and risk of death: results from two large cohort studies in France and UK. Eur Neuropsychopharmacol 25:1566–1577. https://doi.org/10.1016/j.euroneuro.2015.07.006
Waring WS (2012) Clinical use of antidepressant therapy and associated cardiovascular risk. Drug Healthc Patient Saf 4:93–101. https://doi.org/10.2147/DHPS.S28804
Vroegop AV, Vanderveken OM, Boudewyns AN, Scholman J, Saldien V, Wouters K, Braem MJ, van de Heyning PH, Hamans E (2014) Drug-induced sleep endoscopy in sleep-disordered breathing: report on 1,249 cases. Laryngoscope 124:797–802. https://doi.org/10.1002/lary.24479
Gonzalez Castro LN, Mehta JH, Brayanov JB, Mullen GJ (2017) Quantification of respiratory depression during pre-operative administration of midazolam using a non-invasive respiratory volume monitor. PLoS One 12:e0172750. https://doi.org/10.1371/journal.pone.0172750
Zivin K, Kim HM, Yosef M, Maust DT, Valenstein M, Smith EG, Davydow DS (2016) Antidepressant medication treatment and risk of death. J Clin Psychopharmacol 36:445–452. https://doi.org/10.1097/JCP.0000000000000545
Vinkers DJ, Gussekloo J, van der Mast RC et al (2003) Benzodiazepine use and risk of mortality in individuals aged 85 years or older. JAMA 290:2942–2943. https://doi.org/10.1001/jama.290.22.2942
Hogan DB, Maxwell CJ, Fung TS et al (2003) Prevalence and potential consequences of benzodiazepine use in senior citizens: results from the Canadian Study of Health and Aging. Can J Clin Pharmacol 10:72–77
Rumble R, Morgan K (1992) Hypnotics, sleep, and mortality in elderly people. J Am Geriatr Soc 40:787–791
Gisev N, Hartikainen S, Chen TF, Korhonen M, Bell JS (2011) Mortality associated with benzodiazepines and benzodiazepine-related drugs among community-dwelling older people in Finland: a population-based retrospective cohort study. Can J Psychiatr 56:377–381. https://doi.org/10.1177/070674371105600609
Jaussent I, Ancelin M-L, Berr C, Pérès K, Scali J, Besset A, Ritchie K, Dauvilliers Y (2013) Hypnotics and mortality in an elderly general population: a 12-year prospective study. BMC Med 11:212. https://doi.org/10.1186/1741-7015-11-212
Oderda LH, Young JR, Asche CV, Pepper GA (2012) Psychotropic-related hip fractures: meta-analysis of first-generation and second-generation antidepressant and antipsychotic drugs. Ann Pharmacother 46:917–928. https://doi.org/10.1345/aph.1Q589
Pouwels S, van Staa TP, Egberts ACG, Leufkens HGM, Cooper C, de Vries F (2009) Antipsychotic use and the risk of hip/femur fracture: a population-based case–control study. Osteoporos Int 20:1499–1506. https://doi.org/10.1007/s00198-008-0826-5
Rabenda V, Nicolet D, Beaudart C, Bruyère O, Reginster JY (2013) Relationship between use of antidepressants and risk of fractures: a meta-analysis. Osteoporos Int 24:121–137. https://doi.org/10.1007/s00198-012-2015-9
Kragh Ekstam A, Elmståhl S (2016) Do fall-risk-increasing drugs have an impact on mortality in older hip fracture patients? A population-based cohort study. Clin Interv Aging 11:489–496. https://doi.org/10.2147/CIA.S101832
van de Ven LI, Klop C, Overbeek JA, de Vries F, Burden AM, Janssen PK (2018) Association between use of antidepressants or benzodiazepines and the risk of subsequent fracture among those aged 65+ in the Netherlands. Osteoporos Int 29:2477–2485. https://doi.org/10.1007/s00198-018-4632-4
Norwegian Institute of Public Health WHO Collaborating Center for drug Statistics Methodology ATC/DDD Index. In: https://www.whocc.no/atc_ddd_index. Accessed 19 Dec 2018
Herings RM, Stricker BH, de Boer A et al (1996) Current use of thiazide diuretics and prevention of femur fractures. J Clin Epidemiol 49:115–119
Greenland S (1989) Modeling and variable selection in epidemiologic analysis. Am J Public Health 79:340–349. https://doi.org/10.2105/AJPH.79.3.340
Lenze EJ, Munin MC, Dew MA, Rogers JC, Seligman K, Mulsant BH, Reynolds CF (2004) Adverse effects of depression and cognitive impairment on rehabilitation participation and recovery from hip fracture. Int J Geriatr Psychiatry 19:472–478. https://doi.org/10.1002/gps.1116
Bliuc D, Nguyen ND, Milch VE et al (2009) Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 301:513–521. https://doi.org/10.1001/jama.2009.50
Cameron ID, Chen JS, March LM, Simpson JM, Cumming RG, Seibel MJ, Sambrook PN (2010) Hip fracture causes excess mortality owing to cardiovascular and infectious disease in institutionalized older people: a prospective 5-year study. J Bone Miner Res 25:866–872. https://doi.org/10.1359/jbmr.091029
Biffi A, Scotti L, Rea F et al (2018) Adherence to antidepressants and mortality in elderly patients with cardiovascular disease. Clin Drug Investig 38:593–602. https://doi.org/10.1007/s40261-018-0642-4
Krivoy A, Balicer RD, Feldman B, Hoshen M, Zalsman G, Weizman A, Shoval G (2016) Adherence to antidepressants is associated with lower mortality: a 4-year population-based cohort study. J Clin Psychiatry 77:e566–e572. https://doi.org/10.4088/JCP.14m09531
Shoval G, Stubbs B, Balicer RD, Feldman B, Hoshen M, Zalsman G, Sagy R, Hochman E, Weizman A, Krivoy A (2017) Low adherence to antidepressants is associated with increased mortality in Parkinson disease patients. Parkinsonism Relat Disord 43:92–96. https://doi.org/10.1016/j.parkreldis.2017.07.032
Gordon SF, Dainty C, Smith T (2012) Why and when to withdraw drugs in the elderly and frail. Prescriber 23:47–51. https://doi.org/10.1002/psb.924
Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D (2008) STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther 46:72–83
American Geriatrics Society 2012 Beers Criteria Update Expert Panel (2012) American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 60:616–631. https://doi.org/10.1111/j.1532-5415.2012.03923.x
Scottish Government Polypharmacy Model of Care Group (2018) Polypharmacy guidance, realistic prescribing
Nederlands Huisartsen Genootschap (NHG) (2012) De Nederlandse Vereniging voor Klinische Geriatrie NVKG, Orde van Medisch Specialisten (OMS) Multidisciplinaire richtlijn polyfarmacie bij ouderen, https://www.nhg.org/themas/publicaties/multidisciplinaire-richtlijn-polyfarmacie-bij-ouderen. Accessed 13 June 2018
Kalman D, Morissette SB, George TP (2005) Co-morbidity of smoking in patients with psychiatric and substance use disorders. Am J Addict 14:106–123. https://doi.org/10.1080/10550490590924728
Thun MJ, Carter BD, Feskanich D, Freedman ND, Prentice R, Lopez AD, Hartge P, Gapstur SM (2013) 50-year trends in smoking-related mortality in the United States. N Engl J Med 368:351–364. https://doi.org/10.1056/NEJMsa1211127
Serretti A, Mandelli L (2010) Antidepressants and body weight: a comprehensive review and meta-analysis. J Clin Psychiatry 71:1259–1272. https://doi.org/10.4088/JCP.09r05346blu
Blumenthal SR, Castro VM, Clements CC, Rosenfield HR, Murphy SN, Fava M, Weilburg JB, Erb JL, Churchill SE, Kohane IS, Smoller JW, Perlis RH (2014) An electronic health records study of long-term weight gain following antidepressant use. JAMA Psychiatry 71:889–896. https://doi.org/10.1001/jamapsychiatry.2014.414
Global BMI Mortality Collaboration, Di Angelantonio E, Bhupathiraju S et al (2016) Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 388:776–786. https://doi.org/10.1016/S0140-6736(16)30175-1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. de Bruin reports personal fees from Pfizer, personal fees from Novartis, personal fees from Sanofi, outside the submitted work;
Dr. Klop has nothing to disclose;
Dr. Wyers has nothing to disclose;
Dr. Overbeek reports other from Universiteit Utrecht / Universitair Medisch Centrum Maastricht, during the conduct of the study; Comment: Employee of the PHARMO Institute for Drug Outcomes Research. This independent research institute performs financially supported studies for government and related healthcare authorities and several pharmaceutical companies. The PHARMO Institute received funding from Universiteit Utrecht / Universitair Medisch Centrum Maastricht for this study.
Dr. Geusens reports grants and personal fees from Amgen, grants from Pfizer, grants from MSD, grants from UCB, grants from Abbott, grants and personal fees from Lilly, grants from BMS, grants from Novartis, grants from Roche, grants from Will Pharma, outside the submitted work.
Dr. van den Bergh reports grants and personal fees from Amgen, grants and personal fees from Eli Lilly, personal fees from UCB, outside the submitted work; .
Dr. Driessen has nothing to disclose;
Dr. de Vries reports that he supervises a PhD student who is also employed with F. Hoffmann la Roche ltd., Basel, Switzerland. The topic of this PhD is not related to the current manuscript. I have not received any reimbursments or fees for this.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
de Bruin, I.J.A., Klop, C., Wyers, C.E. et al. All-cause mortality with current and past use of antidepressants or benzodiazepines after major osteoporotic and hip fracture. Osteoporos Int 30, 573–581 (2019). https://doi.org/10.1007/s00198-019-04851-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-04851-9