Abstract
Summary
We performed a study to identify potential causes and risk factors of vertebral fracture cascade. Vertebral fracture cascade is a severe clinical event in patients with bone fragility. Only half of patients have an identified cause of secondary osteoporosis.
Introduction
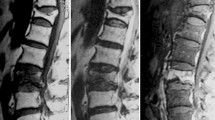
Vertebral fracture (VF) is the most common osteoporotic fracture, and a strong risk factor of subsequent VFs leading to VF cascade (VFC). We prompted a study to identify potential causes and risk factors of VFC.
Methods
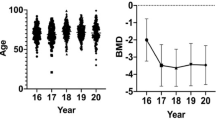
VFC observations were collected retrospectively between January 2016 and April 2017. VFC was defined as an occurrence of at least three VFs within 1 year.
Results
We included in 10 centers a total of 113 patients with VFC (79.6% of women, median age 73, median number of VFs in the cascade, 5). We observed 40.5% and 30.9% of patients with previous major fractures and a previous VF, respectively, and 68.6% with densitometric osteoporosis; 18.9% of patients were currently receiving oral glucocorticoids and 37.1% in the past.
VFC was attributed by the physician to postmenopausal osteoporosis in 54% of patients. A secondary osteoporosis associated with the VFC was diagnosed in 52 patients: glucocorticoid-induced osteoporosis (25.7%), non-malignant hemopathies (6.2%), alcoholism (4.4%), use of aromatase inhibitors (3.6%), primary hyperparathyroidism (2.7%), hypercorticism (2.7%), anorexia nervosa (2.7%), and pregnancy and lactation-associated osteoporosis (1.8%). A total of 11.8% of cases were reported following a vertebroplasty procedure. A total of 31.5% patients previously received an anti-osteoporotic treatment. In six patients, VFC occurred early after discontinuation of an anti-osteoporotic treatment, in the year after the last dose effect was depleted: five after denosumab and one after odanacatib.
Conclusion
The results of this retrospective study showed that only half of VFC occurred in patients with a secondary cause of osteoporosis. Prospective studies are needed to further explore the determinants of this severe complication of osteoporosis.

Similar content being viewed by others
References
Warriner AH, Patkar NM, Curtis JR, Delzell E, Gary L, Kilgore M, Saag K (2011) Which fractures are most attributable to osteoporosis? J Clin Epidemiol 64:46–53. https://doi.org/10.1016/j.jclinepi.2010.07.007
Kado DM, Browner WS, Palermo L et al (1999) Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med 159:1215–1220
Ensrud KE, Thompson DE, Cauley JA et al (2000) Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. Fracture Intervention Trial Research Group. J Am Geriatr Soc 48:241–249
Briggs AM, Greig AM, Wark JD (2007) The vertebral fracture cascade in osteoporosis: a review of aetiopathogenesis. Osteoporos Int 18:575–584. https://doi.org/10.1007/s00198-006-0304-x
Lindsay R, Silverman SL, Cooper C et al (2001) Risk of new vertebral fracture in the year following a fracture. JAMA 285:320–323
Amiche MA, Albaum JM, Tadrous M, Pechlivanoglou P, Lévesque LE, Adachi JD, Cadarette SM (2016) Fracture risk in oral glucocorticoid users: a Bayesian meta-regression leveraging control arms of osteoporosis clinical trials. Osteoporos Int 27:1709–1718. https://doi.org/10.1007/s00198-015-3455-9
Brochot P, Eschard JP, Paternotte L et al (1991) Vertebral compressions revealing Cushing’s syndrome 3 cases. Rev Rhum Mal Osteoartic 58:799–801
van der Veer E, van der Goot W, de Monchy JGR et al (2012) High prevalence of fractures and osteoporosis in patients with indolent systemic mastocytosis. Allergy 67:431–438. https://doi.org/10.1111/j.1398-9995.2011.02780.x
Ozdemir D, Tam AA, Dirikoc A, Ersoy R, Cakir B (2015) Postpartum osteoporosis and vertebral fractures in two patients treated with enoxaparin during pregnancy. Osteoporos Int 26:415–418. https://doi.org/10.1007/s00198-014-2852-9
Xie W, Jin D, Wan C, Ding J, Zhang S, Jiang X, Xu J (2015) The incidence of new vertebral fractures following vertebral augmentation: a meta-analysis of randomized controlled trials. Medicine (Baltimore) 94:e1532. https://doi.org/10.1097/MD.0000000000001532
Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, Graves S, Staples MP, Murphy B (2009) A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med 361:557–568. https://doi.org/10.1056/NEJMoa0900429
Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, Edwards R, Gray LA, Stout L, Owen S, Hollingworth W, Ghdoke B, Annesley-Williams DJ, Ralston SH, Jarvik JG (2009) A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 361:569–579. https://doi.org/10.1056/NEJMoa0900563
Blasco J, Martinez-Ferrer A, Macho J, San Roman L, Pomés J, Carrasco J, Monegal A, Guañabens N, Peris P (2012) Effect of vertebroplasty on pain relief, quality of life, and the incidence of new vertebral fractures: a 12-month randomized follow-up, controlled trial. J Bone Miner Res Off J Am Soc Bone Miner Res 27:1159–1166. https://doi.org/10.1002/jbmr.1564
Abbad N, Lemeunier L, Cotten A, Chastanet P, Cortet B (1983) (2016) [Efficacy and tolerance of vertebroplasty and kyphoplasty for vertebral osteoporotic fractures at Lille University Hospital]. Presse Medicale Paris Fr 45:552–555. https://doi.org/10.1016/j.lpm.2016.01.031
Lamy O, Gonzalez-Rodriguez E, Stoll D, Hans D, Aubry-Rozier B (2017) Severe rebound-associated vertebral fractures after Denosumab discontinuation: 9 clinical cases report. J Clin Endocrinol Metab 102:354–358. https://doi.org/10.1210/jc.2016-3170
Aubry-Rozier B, Gonzalez-Rodriguez E, Stoll D, Lamy O (2016) Severe spontaneous vertebral fractures after denosumab discontinuation: three case reports. Osteoporos Int 27:1923–1925. https://doi.org/10.1007/s00198-015-3380-y
Anastasilakis AD, Polyzos SA, Makras P, Aubry-Rozier B, Kaouri S, Lamy O (2017) Clinical features of 24 patients with rebound-associated vertebral fractures after denosumab discontinuation: systematic review and additional cases. J Bone Miner Res Off J Am Soc Bone Miner Res 32:1291–1296. https://doi.org/10.1002/jbmr.3110
Anastasilakis AD, Tournis S, Yavropoulou MP, Polyzos SA, Makras P (2018) Multiple vertebral fractures following denosumab discontinuation: are we exaggerating? Calcif Tissue Int 103:107–108. https://doi.org/10.1007/s00223-018-0409-1
Cummings SR, Ferrari S, Eastell R, Gilchrist N, Jensen JEB, McClung M, Roux C, Törring O, Valter I, Wang AT, Brown JP (2018) Vertebral fractures after discontinuation of denosumab: a post hoc analysis of the randomized placebo-controlled FREEDOM trial and its extension. J Bone Miner Res Off J Am Soc Bone Miner Res 33:190–198. https://doi.org/10.1002/jbmr.3337
Lamy O, Gonzalez-Rodriguez E (2018) Underestimation of vertebral fractures after denosumab discontinuation. J Bone Miner Res Off J Am Soc Bone Miner Res 33. https://doi.org/10.1002/jbmr.3370
Tripto-Shkolnik L, Rouach V, Marcus Y, Rotman-Pikielny P, Benbassat C, Vered I (2018) Vertebral fractures following denosumab discontinuation in patients with prolonged exposure to bisphosphonates. Calcif Tissue Int 103:44–49. https://doi.org/10.1007/s00223-018-0389-1
Tsourdi E, Langdahl B, Cohen-Solal M, Aubry-Rozier B, Eriksen EF, Guañabens N, Obermayer-Pietsch B, Ralston SH, Eastell R, Zillikens MC (2017) Discontinuation of denosumab therapy for osteoporosis: a systematic review and position statement by ECTS. Bone 105:11–17. https://doi.org/10.1016/j.bone.2017.08.003
Niimi R, Kono T, Nishihara A, Hasegawa M, Kono T, Sudo A (2018) Rebound-associated vertebral fractures after discontinuation of denosumab for the treatment of maxillitis. Osteoporos Int 29:769–772. https://doi.org/10.1007/s00198-017-4334-3
Popp AW, Zysset PK, Lippuner K (2016) Rebound-associated vertebral fractures after discontinuation of denosumab-from clinic and biomechanics. Osteoporos Int 27:1917–1921. https://doi.org/10.1007/s00198-015-3458-6
Eastell R, Cedel SL, Wahner HW, Riggs BL, Melton LJ III (1991) Classification of vertebral fractures. J Bone Miner Res Off J Am Soc Bone Miner Res 6:207–215. https://doi.org/10.1002/jbmr.5650060302
Van Staa TP, Leufkens HG, Abenhaim L et al (2000) Use of oral corticosteroids and risk of fractures. J Bone Miner Res Off J Am Soc Bone Miner Res 15:993–1000. https://doi.org/10.1359/jbmr.2000.15.6.993
Pedersini R, Monteverdi S, Mazziotti G, Amoroso V, Roca E, Maffezzoni F, Vassalli L, Rodella F, Formenti AM, Frara S, Maroldi R, Berruti A, Simoncini E, Giustina A (2017) Morphometric vertebral fractures in breast cancer patients treated with adjuvant aromatase inhibitor therapy: a cross-sectional study. Bone 97:147–152. https://doi.org/10.1016/j.bone.2017.01.013
Veronese N, Luchini C, Solmi M, Sergi G, Manzato E, Stubbs B (2018) Monoclonal gammopathy of undetermined significance and bone health outcomes: a systematic review and exploratory meta-analysis. J Bone Miner Metab 36:128–132. https://doi.org/10.1007/s00774-017-0817-8
Piot JM, Royer M, Schmidt-Tanguy A, Hoppé E, Gardembas M, Bourrée T, Hunault M, François S, Boyer F, Ifrah N, Renier G, Chevailler A, Audran M, Chappard D, Libouban H, Mabilleau G, Legrand E, Bouvard B (2015) Factors associated with an increased risk of vertebral fracture in monoclonal gammopathies of undetermined significance. Blood Cancer J 5:e345. https://doi.org/10.1038/bcj.2015.71
Andrew SM, Freemont AJ (1993) Skeletal mastocytosis. J Clin Pathol 46:1033–1035
Rossini M, Zanotti R, Orsolini G, Tripi G, Viapiana O, Idolazzi L, Zamò A, Bonadonna P, Kunnathully V, Adami S, Gatti D (2016) Prevalence, pathogenesis, and treatment options for mastocytosis-related osteoporosis. Osteoporos Int 27:2411–2421. https://doi.org/10.1007/s00198-016-3539-1
Barete S, Assous N, de Gennes C, Grandpeix C, Feger F, Palmerini F, Dubreuil P, Arock M, Roux C, Launay JM, Fraitag S, Canioni D, Billemont B, Suarez F, Lanternier F, Lortholary O, Hermine O, Frances C (2010) Systemic mastocytosis and bone involvement in a cohort of 75 patients. Ann Rheum Dis 69:1838–1841. https://doi.org/10.1136/ard.2009.124511
Abramowitz JD, Weinerman SA (2012) Osteoporosis as the sole manifestation of systemic mastocytosis in a young man. Endocr Pract 18:e158–e161. https://doi.org/10.4158/EP12062.CR
Yoshihara A, Okubo Y, Tanabe A, Sata A, Nishimaki M, Kawamata T, Kubo O, Hori T, Takano K (2007) A juvenile case of Cushing’s disease incidentally discovered with multiple bone fractures. Intern Med Tokyo Jpn 46:583–587
Notsu M, Kanazawa I, Tanaka S, Yamaguchi T, Sugimoto T (2016) Serum dipeptidyl peptidase-4 is associated with multiple vertebral fractures in type 2 diabetes mellitus. Clin Endocrinol 84:332–337. https://doi.org/10.1111/cen.12971
Choi MK, Kim SM (2017) Nontraumatic multiple vertebral compression fractures induced by primary hyperparathyroidism: a case report and literature review. World Neurosurg 108:992.e5–992.e9. https://doi.org/10.1016/j.wneu.2017.08.157
Ren H, Jiang J, Chen J, Wang J (2015) Risk factors of new symptomatic vertebral compression fractures in osteoporotic patients undergone percutaneous vertebroplasty. Eur Spine J 24:750–758. https://doi.org/10.1007/s00586-015-3786-4
Martinez-Ferrer A, Blasco J, Carrasco JL et al (2013) Risk factors for the development of vertebral fractures after percutaneous vertebroplasty. J Bone Miner Res Off J Am Soc Bone Miner Res 28:1821–1829. https://doi.org/10.1002/jbmr.1899
Lu K, Liang C-L, Hsieh C-H, Tsai YD, Chen HJ, Liliang PC (2012) Risk factors of subsequent vertebral compression fractures after vertebroplasty. Pain Med 13:376–382. https://doi.org/10.1111/j.1526-4637.2011.01297.x
Black DM, Arden NK, Palermo L, Pearson J, Cummings SR (1999) Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of Osteoporotic Fractures Research Group. J Bone Miner Res Off J Am Soc Bone Miner Res 14:821–828. https://doi.org/10.1359/jbmr.1999.14.5.821
Roux C, Fechtenbaum J, Kolta S, Briot K, Girard M (2007) Mild prevalent and incident vertebral fractures are risk factors for new fractures. Osteoporos Int 18:1617–1624. https://doi.org/10.1007/s00198-007-0413-1
Ross PD, Genant HK, Davis JW, Miller PD, Wasnich RD (1993) Predicting vertebral fracture incidence from prevalent fractures and bone density among non-black, osteoporotic women. Osteoporos Int 3:120–126
Binkley N, Krueger D, de Papp AE (2018) Multiple vertebral fractures following osteoporosis treatment discontinuation: a case-report after long-term Odanacatib. Osteoporos Int. https://doi.org/10.1007/s00198-018-4385-0
Anastasilakis AD, Yavropoulou MP, Makras P, Sakellariou GT, Papadopoulou F, Gerou S, Papapoulos SE (2017) Increased osteoclastogenesis in patients with vertebral fractures following discontinuation of denosumab treatment. Eur J Endocrinol 176:677–683. https://doi.org/10.1530/EJE-16-1027
Broy SB (2016) The vertebral fracture cascade: etiology and clinical implications. J Clin Densitom 19:29–34. https://doi.org/10.1016/j.jocd.2015.08.007
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Breuil received grant support and lecture fees from Amgen, Novartis, Chugai, and Lilly. Dr. Briot has received research grants or honoraria from Amgen, Lilly, Medtronic, and MSD. Dr. Cortet has received research grants or honoraria from Amgen, Expanscience, Ferring, Lilly, Medtronic, MSD, Mylan, Novartis, Roche diagnostics, Théramex, and UCB. Dr. Thomas received grant support, lecture fees, and consulting fees from Amgen, Merck Sharp & Dohme, and UCB Pharma; grant support and lecture fees from Chugai and Pfizer; consulting fees from Expanscience, Gilead Sciences, LCA, Thuasne, and Medac; grant support and consulting fees from HAC Pharma; grant support from Novartis; lecture fees from AbbVie, Biogen, and Bristol-Myers Squibb; and lecture fees and consulting fees from Eli Lilly and Teva Pharmaceutical Industries. Dr. Roux has received grants and/or honoraria from Alexion, Amgen, MSD, UCB. Dr. Che, Dr. Paccou, Dr. Chapuis, Dr. Debiais, Dr. Mehsen-Cetre, Dr. Javier, and Dr. Loiseau Peres have no disclosure to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Che, H., Breuil, V., Cortet, B. et al. Vertebral fractures cascade: potential causes and risk factors. Osteoporos Int 30, 555–563 (2019). https://doi.org/10.1007/s00198-018-4793-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-018-4793-1