Abstract
Summary
There is a need of studies exploring the link between socioeconomic status and DXA scans and osteoporotic fracture, which was the aim of the present study. No differences in socioeconomic status and risk of osteoporotic fractures were found. However, women with further/higher education and higher income are more often DXA-scanned.
Introduction
Lower socioeconomic status is known to be associated with a range of chronic conditions and with access to health care services. The link between socioeconomic status and the use of DXA scans and osteoporotic fracture, however, needs to be explored more closely. Therefore, the aim of this study was to examine the relationship between socioeconomic status and both DXA scan utilization and major osteoporotic fractures (MOF) using a population-based cohort of Danish women and national registers.
Methods
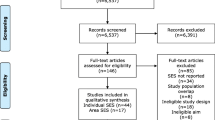
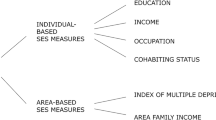
The study included 17,155 women (65–81 years) sampled from the Risk-stratified Osteoporosis Strategy Evaluation study (ROSE). Information on socioeconomic background, DXA scans, and MOFs was retrieved from national registers. Competing-risk regression analyses were performed. Mean follow-up was 4.8 years.
Results
A total of 4245 women had a DXA scan (24.7%) and 1719 (10.0%) had an incident MOF during follow-up. Analyses showed that women with basic education had a lower probability of undergoing DXA scans than women with further or higher education (greater than upper secondary education and vocational training education) (subhazard ratio (SHR) = 0.82; 95% CI 0.75–0.89, adjusted for age and comorbidity). Moreover, women with disposable income in the low and medium tertiles had a lower probability of undergoing DXA scans than women in the high-income tertile (SHR = 0.90; 95% CI 0.84–0.97 and SHR = 0.88, 95% CI 0.82–0.95, respectively, adjusted for age and comorbidity). No association between socioeconomic background and probability of DXA was found in adjusted analyses.
Conclusion
The study found no differences in risk of osteoporotic fractures depending on socioeconomic status. However, women with further or higher education as well as higher income are more often DXA-scanned.

Similar content being viewed by others
References
Mackenbach PJ, Stirbu I, Roskam AJR, Schaap MM, Menvielle G, Leinsalu M, Kunst AEK, for the European Union Working Group on Socioeconomic Inequalities in Health (2008) Socioeconomic inequalities in health in 22 European countries. N Engl J Med 358:2468–2481
Diderichsen F, Andersen I, Manual C and the Working group of the Danish review on social determinants of health (2011) Health Inequality - determinants and policies. Report, Department of Public Health, University of Copenhagen, Copenhagen.
Adler NE, Newman K (2002) Socioeconomic disparities in health: pathways and policies. Health Aff 21(2):60–76
Pickett KE, Wilkinson RG (2015) Income inequality and health: a causal review. Soc Sci Med 128:316–326
Marmot MG (2003) Understanding social inequalities in health. Perspect Biol Med 46(3):s9–S23
Fiscella K, Franks P, Gold MR, Clancy CM (2000) Inequality in quality. Addressing socioeconomic, racial, and ethnic disparities in health care. JAMA 283(19):2579–2574
World Health Organisation (2007) Assessment of osteoporosis at the primary health care level. Technical Report, World health Oranisation Scientific Group.
Crandall CJ, Han W, Greendale GA, Seeman T, Tepper P, Thurston R, Karvonen-Gutierrez C, Karlamangla AS (2014) Socioeconomic status in relation to incident fracture risk in the study of Women’s health across the nation. Osteoporos Int 25(4):1379–1388. https://doi.org/10.1007/s00198-013.2616-y.
Brennan SL, Holloway KL, Williams LJ, Kotowicz MA, Bucki-Smith G, Moloney DJ, Dobbins AG, Timney EN, Pasco JA (2015) The social gradient of fractures at any skeletal site in men and women: data from the Geelong osteoporosis study fracture grid. Osteoporos Int 26:1351–1359
Moradzadeh R, Nadrian H, Golboni F, Kazemi-Galougahi MH, Moghimi N (2016) Economic inequalities amongst women with osteoporosis-related fractures: an application of concentration index decomposition. Health Promot Perspect 6(4):190–195
Navarro MC, Sosa M, Saavedra P, Lainez P, Marrero M, Torres M, Medina CD (2009) Poverty is a risk factor for osteoporotic fractures. Osteoporos Int 20:393–398
Syddall HE, Evandrou M, Dennison EM, Cooper C, Sayer AA (2012) Social inequalities in osteoporosis and fracture among community dwelling older men and women: findings from the Herfordshire Cohort Study. Arch Osteoporos 7(0):37–48
Ong T, Tan W, Marshall L, Sahota O (2015) The relationship between socioeconomic status and fracture in a fracture clinic setting: data from the Nottingham fracture liaison service. Injury, Int J Care Injured 46:366–370
Brennan SL, Pasco JA, Urquhart DM, Oldenburg B, Hanna F, Wluka AE (2009) The association between socioeconomic status and osteoporotic fracture in population-based adults: a systematic review. Osteoporos Int 20:1487–1497
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312(7041):1254–1259
Rubin KH, Abrahamsen B, Hermann AP, Bech M, Gram J, Brixen K (2011) Prevalence of risk factors for fractures and use of DXA scanning in Danish women. A regional population-based study. Osteoporos Int 22(5):1401–1409. https://doi.org/10.1007/s00198-010-1348-5
Born R, Zwahlen M (2013) Disparities in bone density measurement history and osteoporosis medication utilization in Swiss women: results from the Swiss Health Survey 2007. BMC Musculoskelet Disord 14:10. https://doi.org/10.1186/1471-2474-14-10
Brennan SL, Wluka AE, Gould H, Nicholson GC, Leslie WD, Ebling PR, Oldenburg B, Kotowicz MA, Pasco JA (2013) Social Determinants of bone densitometry uptake for osteoporosis risk in patients aged 50 Yr and older: a systematic review. J Clin Densitom 15(2):165–175
Rubin KH, Holmberg T, Rothmann MJ, Høiberg M, Barkmann R, Gram J, Hermann AP, Bech M, Rasmussen O, Glüer CC, Brixen K (2015) The risk-stratified osteoporosis strategy evaluation study (ROSE): a randomized prospective population-based study. Design and baseline characteristics. Calcif Tissue Int 2015 96(2):167–179. https://doi.org/10.1007/s00223-014-9950-8
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987 40(5):373–383
Hoiberg MP, Rubin KH, Gram J, Hermann AP, Brixen K, Haugeberg G (2015) Risk factors for osteoporosis and factors related to the use of DXA in Norway. Arch Osteoporos 10:16
Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, Ott SM, Torner JC, Quandt SA, Reiss TF, Ensrud KE (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fract Interv Trial Res Group Lancet 348(9041):1535–1541
Black DM, Reid IR, Cauley JA, Cosman F, Leung PC, Lakatos P, Lippuner K, Cummings SR, Hue TF, Mukhopadhyay A, Tan M, Aftring RP, Eastell R (2015) The effect of 6 versus 9 years of zoledronic acid treatment in osteoporosis: a randomized second extension to the HORIZON-Pivotal Fracture Trial (PFT). J Bone Miner Res 30(5):934–944. https://doi.org/10.1002/jbmr.2442
Rothmann MJ, Jakobsen PR, Jensen CM, Hermann AP, Smith AC, Clemensen J (2018) Experiences of being diagnosed with osteoporosis: a meta-synthesis. Arch Osteoporos 13:21. https://doi.org/10.1007/s11657-018-0436-6
McCloskey EV, Johansson H, Oden A, Austin M, Siris E, Wang A, Lewiecki EM, Lorenc R, Libanati C, Kanis JA (2012) Denosumab reduces the risk of osteoporotic fractures in postmenopausal women, particularly in those with moderate to high fracture risk as assessed with FRAX. J Bone Miner Res 27(7):1480–1486. https://doi.org/10.1002/jbmr.1606
Kanis JA, Johansson H, Oden A, McCloskey EV (2009) Bazedoxifene reduces vertebral and clinical fractures in postmenopausal women at high risk assessed with FRAX. Bone 44(6):1049–1054. https://doi.org/10.1016/j.bone.2009.02.014
McCloskey EV, Johansson H, Oden A, Vasireddy S, Kayan K, Pande K, Jalava T, Kanis JA (2009) Ten-year fracture probability identifies women who will benefit from clodronate therapy--additional results from a double-blind, placebo-controlled randomised study. Osteoporos Int 20(5):811–817. https://doi.org/10.1007/s00198-008-0786-9
Turner DA, Khioe RFS, Shepstone L, Lenaghan E, Cooper C, Gittoes N, Harvey NC, Holland R, Howe A, McCloskey E, O'Neill TW, Torgerson D, Fordham R, Study Team SCOOP (2018) The cost-effectiveness of screening in the community to reduce osteoporotic fractures in older women in the UK: economic evaluation of the SCOOP study. J Bone Miner Res 33(5):845–851. https://doi.org/10.1002/jbmr.3381
Reyes C, García_gil M, Elorza JM, Fina-Avilés F, Mendez-Boo L, Hermosilla E, Coma E, Carbonell C, Medina-Peralta M, Ramos R, Bolibar B, Díez-Pérez A, Prieto-Alhambra D (2015) Socioeconomic status and its association with the risk of developing hip fractures: a region-wide ecological study. Bone 73:127–131
Quah C, Boulton C, Moran C (2011) The influence of socioeconomic status on the incidence, outcome and mortality of fractures of the hip. J Bone Joint Surg 93-B:801–805
Leu Agelii M, Lehtinen-Jacks S, Zetterberg H, Sundh V, Björkelund C, Lissner L (2017) Low vitamin D status in relation to cardiovascular disease and mortality in Swedish women effect of extended follow-up. Nutr, Metab Cardiovasc Dis 27:1143–1151
Kristensen PK, Thillemann TM, Pedersen AB, Søballe K, Johnsen SP (2017) Socioeconomic inequality in clinical outcome among hip fracture patients: a nationwide cohort study. Osteoporos Int 28:1233–1243. https://doi.org/10.1007/s00198-016-3853-7
Wastensson JW, Weitoft GR, Parker MG, Johnell K (2013) Educational level and use of osteoporosis drugs in elderly men and women: a Swedish nationwide register-based study. Osteoporos Int 24:433–442
Mosbech J, Jorgensen J, Madsen M, Rostgaard K, Thornberg K, Poulsen TD (1995) The national patient registry. Evaluation of data quality. UgeskrLaeger 157(26):3741–3745
Vestergaard P, Mosekilde L (2002) Fracture risk in patients with celiac disease, Crohn’s disease, and ulcerative colitis: a nationwide follow-up study of 16,416 patients in Denmark. Am J Epidemiol 156(1):1–10. https://doi.org/10.1093/aje/kwf007.
Christensen U, Krølner R, Nilsson CJ, Lyngbye PW, Hougaard CØ, Nygaard E, Thielen K, Holstein BE, Avlund K, Lund R (2014) Addressing social inequality in aging by the Danish occupational social class measurement. J Aging Health 26(1):106–127
Avlund K, Holstein BE, Osler M, Damsgaard MT, Holm-Pedersen P, Rasmussen NK (2003) Social position and health in old age: the relevance of different indicators of social position. Scand J Public Health 31:126–136
Galobardes B, Shaw M, Lawlor DA, Lynch JW, Smith GD (2006) Indicators of socioeconomic position (part 1). J Epidemiol Community Health 60:7–12
Rothmann MJ, Moller S, Holmberg T, Hojberg M, Gram J, Bech M et al (2017) Non-participation in systematic screening for osteoporosis—the ROSE trial. Osteoporos Int 28(12):3389–3399
Acknowledgments
We thank the participants in the Rose study and the technical staff in the four hospitals involved: Odense University Hospital, Odense and Nyborg; Hospital of Southwest Denmark, Esbjerg; and Lillebælt Hospital, Kolding, Denmark.
Funding
The ROSE study was supported by INTERREG (4A JNR 08/4177), the Region of Southern Denmark (JNR 08/8133), and Odense University Hospital (JNR 11/5761). The proofreading and submission of the manuscript was funded by the Danish Arthritis Foundation. The funding agencies had no direct role in the conduct of the study, data collection, analysis, and interpretation of the data, or in the preparation, review, and final approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
S Möller, T Holmberg M Bech, J Gram, JS Tolstrup, KH Rubin have no conflicts of interest. MJ Rothmann has received a speaking fee from Eli Lilly. M Hoiberg is a full-time employee of Boehringer-Ingelheim Norway KS (currently). AP Hermann serves on advisory Boards for Eli Lilly, Amgen, and she has received research funding from Eli Lilly, a speaking fee from Eli Lilly, GSK, Genzyme, Amgen; K Brixen reports other from Merck, Sharpe, Dohme, other from Amgen, other from Novartis, other from NPS, all outside the submitted work.
Rights and permissions
About this article
Cite this article
Holmberg, T., Möller, S., Rothmann, M. et al. Socioeconomic status and risk of osteoporotic fractures and the use of DXA scans: data from the Danish population-based ROSE study. Osteoporos Int 30, 343–353 (2019). https://doi.org/10.1007/s00198-018-4768-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-018-4768-2