Abstract
Summary
Osteoporosis affects many aspects of daily life. The aim of this systematic review was to assess the effects of exercise interventions on functional outcomes in persons with osteoporosis, in comparison with controls.
Methods
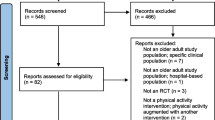
Four databases were searched and yielded 1587 citations. Two reviewers independently determined study eligibility, rated risk of bias, appraised methodological quality of studies, and resolved discordance by consensus.
Results
A total of 28 studies examining 2113 participants met inclusion criteria; 25 studies were suitable for meta-analyses. Four categories of exercise were identified using the ProFaNE taxonomy. After removing studies with high risk of bias and sorting them into intervention sub-types, we were able to sufficiently reduce the heterogeneity. The standardized mean difference (SMD) favored multicomponent exercise for mobility (− 0.56, 95% CI [− 0.81, − 0.32], p = 0.06, I2 = 51%); balance (0.50, 95% CI [0.27, 0.74], p = 0.28, I2 = 21%); and self-reported measures of functioning (− 0.69, 95% CI [− 1.04, − 0.34], p = 0.02, I2 = 61%). Trials were judged at low or unclear risk of selection bias, indicating inadequate reporting and at high risk of performance bias due to lack of participant blinding. The mean methodological quality rating of the studies was 63.5% indicating moderate quality.
Conclusions
A multicomponent exercise program of high-speed training combined with simulated functional tasks is promising to enhance functional outcomes. Due to substantial clinical heterogeneity of the target groups and specific demands of exercise modes, it is unclear which exercise program is optimal.







Similar content being viewed by others
References
Osteoporosis Canada (2011) Managing osteoporosis in primary care: highlights from osteoporosis Canada guidelines. Canadian Pharmacists J 144(sp1):S5–S9.e1
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24(1):23–57. https://doi.org/10.1007/s00198-012-2074-y
World Health Organization (2007) WHO scientific group on the assessment of osteoporosis at primary health care level. World Health Organ (5–7)
Tarride JE, Hopkins RB, Leslie WD, Morin S, Adachi JD, Papaioannou A, Goeree R (2012) The burden of illness of osteoporosis in Canada. Osteoporos Int 23(11):2591–2600. https://doi.org/10.1007/s00198-012-1931-z
Giangregorio LM, MacIntyre NJ, Heinonen A, Cheung AM, Wark JD, Shipp K, Papaioannou A (2014) Too fit to fracture: a consensus on future research priorities in osteoporosis and exercise. Osteoporo Int 25(5):1465–1472. https://doi.org/10.1007/s00198-014-2652-2
Barry BK, Carson RG (2004) The consequences of resistance training for movement control in older adults. J Gerontol Series A, Biolog Sci Med Sci 59(7):730–754
Brady AO, Straight CR, Evans EM (2014) Body composition, muscle capacity, and physical function in older adults: an integrated conceptual model. J Aging Phys Act 22:441–452
Singh MAF (2002) Exercise comes of age: rationale and recommendations for a geriatric exercise prescription. J Gerontol. Series A, Bio Sciences Med Sci 57(5):M262–M282
Ekström H, Dahlin-Ivanoff S, Elmståhl S (2011) Effects of walking speed and results of timed get-up-and-go tests on quality of life and social participation in elderly individuals with a history of osteoporosis-related fractures. J Aging Health 23(8):1379–1399. https://doi.org/10.1177/0898264311418504
Giangregorio LM, Papaioannou A, MacIntyre NJ, Ashe MC, Heinonen A, Shipp K, Cheung AM (2014) Too fit to fracture: exercise recommendations for individuals with osteoporosis or osteoporotic vertebral fracture. Osteoporos Int 25(3):821–835. https://doi.org/10.1007/s00198-013-2523-2
Papaioannou A, Morin S, Cheung AM, Atkinson S, Brown JP, Feldman S, Leslie WD (2010) Clinical practice guidelines for the diagnosis and management of osteoporosis in Canada. CMAJ 182(17):1864–1873. https://doi.org/10.1503/cmaj.100771
Howe TE, Shea B, Dawson LJ, Downie F, Murray A, Ross C (2011) Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev. (7) DOI: https://doi.org/10.1002/14651858.CD000333.pub2
Kerr D, Morton A, Dick I, Prince R (1996) Exercise effects on bone mass in postmenopausal women are site-specific and load-dependent. J Bone Minl Res: Off J Amer Soc Bone Minl Res 11(2):218–225
Liu-Ambrose TY, Khan KM, Eng JJ, Heinonen A, McKay HA (2004) Both resistance and agility training increase cortical bone density in 75- to 85-year-old women with low bone mass: a 6-month randomized controlled trial. J Clin Densitom: Off J Int Soc Clin Densitom 7(4):390–398. https://doi.org/10.1385/JCD:7:4:390
Wilhelm M, Roskovensky G, Emery K, Manno C, Valek K, Cook C (2012) Effect of resistance exercises on function in older adults with osteoporosis or osteopenia: a systematic review. Physiother Can 64(4):386–394. https://doi.org/10.3138/ptc.2011-31BH
World Health Organization (2002) Towards a common language for functioning. Disabil Health ICF Int Classif 1149:1–22
Higgins JPT, Green S, eds (2011) Cochrane Handbook Syst Rev Interv Vers. 5.1.0
Law M, MacDermid JC (2014) Evaluating the evidence. In: JC MD, Law M (eds) Evidence-based rehabilitations: a guide to practice. Slack Incorporation, New Jersey, pp 129–156
Alp A, Yurtjuran, Merih TT (2009) Effects of Tai Chi exercise on functional and life quality assessments in senile osteoporosis. Turkiye Klinikleri J Med Sci 29(3):687–695
Angin E, Zafer E, Filiz C (2015) The effects of clinical Pilates exercises on bone mineral density, physical performance, and quality of life of women with postmenopausal osteoporosis. J Back Musculoskeletal Rehab 28(4):849–858. https://doi.org/10.3233/BMR-150604
Arnold CM, Busch AJ, Schachter CL, Harrison EL, Olszynski WP (2008) A randomized clinical trial of aquatic versus land exercise to improve balance, function, and quality of life in older women with osteoporosis. Phys Can 60(4):296–306
Basat H, Esmaeilzadeh S, Eskiyurt N (2013) The effects of strengthening and high-impact exercises on bone metabolism and quality of life in postmenopausal women: a randomized controlled trial. J Back Musculoskeletal Rehab 26(4):427–435. https://doi.org/10.3233/BMR-130402
Bennell KL, Matthews B, Greig A, Briggs A, Kelly A, Sherburn M, Wark J (2010) Effects of an exercise and manual therapy program on physical impairments, function and quality-of-life in people with osteoporotic vertebral fracture: a randomised, single-blind controlled pilot trial. BMC Musculoskelet Disord 11(1):36. https://doi.org/10.1186/1471-2474-11-36
Bergland A, Thorsen H, Kåresen R (2011) Effect of exercise on mobility, balance, and health-related quality of life in osteoporotic women with a history of vertebral fracture: a randomized, controlled trial. Osteoporos Int 22(6):1863–1871. https://doi.org/10.1007/s00198-010-1435-7
Borba-Pinheiro CJ, Dantas EHM, Vale RG, Drigo AJ, Carvalho MC, Tonini T, Figueiredo NM (2016) Resistance training programs on bone related variables and functional independence of postmenopausal women in pharmacological treatment: a randomized controlled trial. Arch Gerontol Geriatrics 65(40):36–44. https://doi.org/10.1016/j.archger.2016.02.010
Bravo G, Gauthier P, Roy PM, Payette H, Gaulin P, Harvey M, Dubois MF (1996) Impact of a 12-month exercise program on the physical and psychological health of osteopenic women. J American Geriatrics Society 44(7):756–762
Chien MY, Yang RS, Tsauo JY (2005) Home-based trunk-strengthening exercise for osteoporotic and osteopenic postmenopausal women without fracture-a pilot study. Clin Rehab 19(1):28–36. https://doi.org/10.1191/0269215505cr844oa
Chyu MC, James CR, Sawyer SF, Brismée JM, Xu KT, Poklikuha G, Shen CL (2010) Effects of Tai Chi exercise on posturography, gait, physical function and quality of life in postmenopausal women with osteopenia: a randomized clinical study. Clin Rehab 24(12):1080–1090. https://doi.org/10.1177/0269215510375902
Devereux K, Robertson D, Briffa NK (2005) Effects of a water-based program on women 65 years and over: a randomised controlled trial. Australian J Phys 51(2):102–108
Evstigneeva L, Lesnyak O, Bultink IEM, Lems WF, Kozhemyakina E, Negodaeva E, Belkin A (2016) Effect of twelve-month physical exercise program on patients with osteoporotic vertebral fractures: a randomized, controlled trial. Osteoporos Int 27(8):2515–2524. https://doi.org/10.1007/s00198-016-3560-4
Fleisher L, Trudelle-Jackson E, Thompson M, Smith S (2011) Effects of weight-bearing and resistance exercises on lower extremity strength, postural stability, and quality of life in postmenopausal women with low bone mass. J Womenʼs Health Phy Ther 35(3):114–127. https://doi.org/10.1097/JWH.0b013e31823b072c
Gianoudis J, Ca B, Ebeling PR, Ca N, Sanders KM, Hill K, Daly RM (2014) Effects of a targeted multimodal exercise program incorporating high-speed power training on falls and fracture risk factors in older adults: a community-based randomized controlled trial. J Bone Min Res 29(1):182–191. https://doi.org/10.1002/jbmr.2014
Gold DT, Shipp KM, Pieper CF, Duncan PW, Martinez S, Lyles KW (2004) Group treatment improves trunk strength and psychological status in older women with vertebral fractures: results of a randomized, clinical trial. J Amer Geriatrics Society 52(9):1471–1478
Halvarsson A, Franzen E, Stahle A (2014) Balance training with multi-task exercises improves fall-related self-efficacy, gait, balance performance and physical function in older adults with osteoporosis: a randomized controlled trial. Clin Rehab 29(4):365–375
Hongo M, Itoi E, Sinaki M, Miyakoshi N, Shimada Y, Maekawa S, Mizutani Y (2007) Effect of low-intensity back exercise on quality of life and back extensor strength in patients with osteoporosis: a randomized controlled trial. Osteoporos Int 18(10):1389–1395. https://doi.org/10.1007/s00198-007-0398-9
Kanemaru A, Arahata K, Ohta T, Katoh T, Tobimatsu H, Horiuchi T (2010) The efficacy of home-based muscle training for the elderly osteoporotic women: the effects of daily muscle training on quality of life (QoL). Arch Geron Geriatrics 51(2):169–172. https://doi.org/10.1016/j.archger.2009.10.003
Kronhed AG, Hallberg I, Ödkvist L, Möller M (2009) Effect of training on health-related quality of life, pain and falls in osteoporotic women. Adv Phys 11(3):154–165
Maciaszek J, Osinski W (2012) Effect of Tai Chi on body balance: randomized controlled trial in elderly men with dizziness. Am J Chin Med 40(2):245–253. https://doi.org/10.1142/S0192415X1250019X
Madureira MM, Bonfá E, Takayama L, Pereira RMR (2010) A 12-month randomized controlled trial of balance training in elderly women with osteoporosis: improvement of quality of life. Maturitas 66(2):206–211. https://doi.org/10.1016/j.maturitas.2010.03.009
Marchese DI, Andreal MD, Ventura V, Montalcinp T, Fotf D, Pujia A, July A (2012) Effects of a weight-bearing exercise training on bone mineral density and neuromuscular function of osteopenic women. Europ J. Inflammation 10(3):427–435
Nelson ME, Fiatarone MA, Morganti CM, Trice I, Greenberg RA, Evans WJ (1994) High-intensity strength training on multiple risk factors for osteoporotic fractures. JAMA 272(24):1909–1914. https://doi.org/10.1001/jama.1994.03520240037038
Papaioannou A, Adachi JD, Winegard K, Ferko N, Parkinson W, Cook RJ, McCartney N (2003) Efficacy of home-based exercise for improving quality of life among elderly women with symptomatic osteoporosis-related vertebral fractures. Osteoporos Int 14(8):677–682. https://doi.org/10.1007/s00198-003-1423-2
Smulders E, Weerdesteyn V, Groen BE, Duysens J, Eijsbouts A, Laan R, Van Lankveld W (2010) Efficacy of a short multidisciplinary falls prevention program for elderly persons with osteoporosis and a fall history: a randomized controlled trial. Arch Phys Med Rehab 91(11):1705–1711. https://doi.org/10.1016/j.apmr.2010.08.004
Teixeira LEPP, Silva KNG, Imoto AM, Teixeira TJP, Kayo AH, Montenegro-Rodrigues R, Trevisani VFM (2010) Progressive load training for the quadriceps muscle associated with proprioception exercises for the prevention of falls in postmenopausal women with osteoporosis: a randomized controlled trial. Osteoporos Int 21(4):589–596. https://doi.org/10.1007/s00198-009-1002-2
Tolomio S, Ermolao A, Lalli A, Zaccaria M (2010) The effect of a multicomponent dual-modality exercise program targeting osteoporosis on bone health status and physical function capacity of postmenopausal women. J Women Aging 22(4):241–254. https://doi.org/10.1080/08952841.2010.518866
Wayne PM, Kiel DP, Buring JE, Connors EM, Bonato P, Yeh GY, Davis RB (2012) Impact of Tai Chi exercise on multiple fracture-related risk factors in post-menopausal osteopenic women: a pilot pragmatic randomized trial. BMC Complement Altern Med 12(1):1–12
ProFaNE 2011 Taxonomy manual. http://profane.co/2011/03/24/profane-taxonomy-manual/2011
Zehnacker CH, Bemis-Dougherty A (2007) Effect of weighted exercises on bone mineral density in post-menopausal women. A systematic review. J Geriatr Phys Therapy 30(2):79–88. https://doi.org/10.1519/00139143-200708000-00007
Kemmler W, Bebenek M, Kohl M, von Stengel S (2015) Exercise and fractures in postmenopausal women. Final results of the controlled Erlangen Fitness and Osteoporosis Prevention Study (EFOPS). Osteoporos Int 26(10):2491–2499. https://doi.org/10.1007/s00198-015-3165-3
Wallace BA, Cumming RG (2000) Systematic review of randomized trials of the effect of exercise on bone mass in pre-and postmenopausal women. Calcif Tissue Int 67(1):10–18. https://doi.org/10.1007/s00223001089
Moreira LDF, de Oliveira ML, Lirani-Galvão AP, Marin-Mio RV, dos Santos RN, Lazaretti-Castro M (2014) Physical exercise and osteoporosis: effects of different types of exercises on bone and physical function of postmenopausal women. Arq Bras Endocrinol Metabol 58(5):514–522. https://doi.org/10.1590/0004-2730000003374
Cieza A, Schwarzkopf SR, Sigl T, Stucki G, Melvin J, Stoll T, Walsh N (2004) ICF Core sets for osteoporosis. J Rehab Med 36(Suppl 44):81–86. https://doi.org/10.1080/16501960410016028
Faraone SV (2008) Interpreting estimates of treatment effects: implications for managed care. P T: Peer-Rev J Formul Manag 33(12):700–711
Jansen JP, Fleurence R, Devine B, Itzler R, Barrett A, Hawkins N, Cappelleri JC (2011) Interpreting indirect treatment comparisons and network meta-analysis for health-care decision making: report of the ISPOR task force on indirect treatment comparisons good research practices: part 1. Value Health 14(4):417–428. https://doi.org/10.1016/j.jval.2011.04.002
Lamb SE, Becker C, Gillespie LD, Smith JL, Finnegan S, Potter R, Pfeiffer K (2011) Reporting of complex interventions in clinical trials: development of a taxonomy to classify and describe fall-prevention interventions. Trials 12(1):125. https://doi.org/10.1186/1745-6215-12-125
Miszko T, Cress ME, Slade JM, Covey CJ, Agrawal SK, Doerr CE (2003) Effect of strength and power training on physical function in community-dwelling older adults. J Geront Ser A Biol Sci Med 58(2):171–175
Hazell T, Kenno K, Jakobi J (2007) Functional benefit of power training for older adults. J Aging Phys Act 15(3):349–359. https://doi.org/10.1123/japa.15.3.349
Stengel SV, Kemmler W, Pintag R, Beeskow C, Weineck J, Lauber D, Engelke K (2005) Power training is more effective than strength training for maintaining bone mineral density in postmenopausal women. J Appl Phys 99(1):181–188
Clemson L, Fiatarone Singh MA, Bundy A, Cumming RG, Manollaras K, O’Loughlin P, Black D (2012) Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): randomised parallel trial. BMJ 345:e4547–e4547
Chin A, Paw MJM, van Poppel MNM, Twisk JWR, van Mechelen W (2006) Once a week not enough, twice a week not feasible? A randomised controlled exercise trial in long-term care facilities. Patient Educ Couns 63(1–2):205–214. https://doi.org/10.1016/j.pec.2005.10.008
Pinto RS, Correa CS, Radaelli R, Cadore EL, Brown LE, Bottaro M (2014) Short-term strength training improves muscle quality and functional capacity of elderly women. Age 36(1):365–372. https://doi.org/10.1007/s11357-013-9567-2
Reid KF, Fielding R (2013) Skeletal muscle power: a critical determinant of physical functioning in older adults. Exerc Sport Sci Rev 40(1):4–12
Liu C, Shiroy D, Jones L, Clark D (2014) Systematic review of functional training on muscle strength, physical functioning, and activities of daily living in older adults. Eur Rev Aging Phys Act 11(2):95–106. https://doi.org/10.1007/s11556-014-0144-1
Li F, Harmer P, Fishe KJ, McAuley E, Chaumeton N, Eckstrom E, Wilson NL (2005) Tai Chi and fall reductions in older adults: a randomized controlled trial. J Gerontol A, Bio Sci Med Sci 60(2):187–194
Wayne PM, Berkowitz DL, Litrownik DE, Buring JE, Yeh GY (2014) What do we really know about the safety of Tai Chi?: a systematic review of adverse event reports in randomized trials. Arch Phys Med Rehab 95(12):2470–2483. https://doi.org/10.1016/j.apmr.2014.05.005
Liu CJ, Latham N (2010) Adverse events reported in progressive resistance strength training trials in older adults: 2 sides of a coin. Arch Phys Med Rehab 91(9):1471–1473. https://doi.org/10.1016/j.apmr.2010.06.001
Giangregorio LM, McGill S, Wark JD, Laprade J, Heinonen A, Ashe MC, Papaioannou A (2015) Too fit to fracture: outcomes of a Delphi consensus process on physical activity and exercise recommendations for adults with osteoporosis with or without vertebral fractures. Osteoporos Int 26(3):891–910. https://doi.org/10.1007/s00198-014-2881-4
Takeshima N, Islam MM, Rogers ME, Rogers NL, Sengoku N, Koizumi D, Naruse A (2013) Effects of Nordic walking compared to conventional walking and band-based resistance exercise on fitness in older adults. J Sports Scien Med 12(3):422–430
Thorup CB, Grønkjær M, Spindler H, Andreasen JJ, Hansen J, Dinesen BI, Sørensen EE (2016) Pedometer use and self-determined motivation for walking in a cardiac tele-rehabilitation program: a qualitative study. BMC Sports Science, Med & Rehab 8(1):24
Rodrigues IB, Armstrong JJ, Adachi JD, MacDermid JC (2017) Facilitators and barriers to exercise adherence in patients with osteopenia and osteoporosis: a systematic review. Osteoporos Int 28(3):735–745. https://doi.org/10.1007/s00198-016-3793-2
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
I, first author, Azar Varahrami Vigeh confirm that there are no conflicts of interest for my article.
Electronic supplementary material
ESM 1
(DOCX 36 kb)
Rights and permissions
About this article
Cite this article
Varahra, A., Rodrigues, I.B., MacDermid, J.C. et al. Exercise to improve functional outcomes in persons with osteoporosis: a systematic review and meta-analysis. Osteoporos Int 29, 265–286 (2018). https://doi.org/10.1007/s00198-017-4339-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-4339-y