Abstract
Purpose
Debridement, systemic antibiotics and implant retention (DAIR) is very successful for early periprosthetic joint infection (PJI), but can fail in late-onset cases. We selected patients with PJI who were unsuitable for two-stage exchange total knee arthroplasty (TKA) and compared the outcomes of DAIR with or without degradable calcium-based antibiotics.
Methods
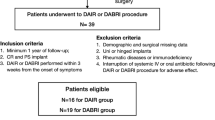
All patients fulfilled the criteria for late-onset PJI of TKA, as defined by an International Consensus Meeting in 2013, but were unsuitable for multistage procedures and TKA exchange due to operative risk. Fifty-six patients (mean age: 70.6 years, SD ± 10.8), in two historical collectives, were treated using a single-stage algorithm consisting of DAIR without antibiotics (control group, n = 33, 2012–2014), or by DAIR following the implantation of degradable antibiotics as indicated by an antibiogram (intervention group, n = 23, 2014–2017). OSTEOSET® (admixed vancomycin/tobramycin), and HERAFILL-gentamicin® were used as carrier systems. The primary endpoint was re-infection or surgical intervention after DAIR.
Results
There were no significant differences between the two groups in terms of mean age, Charlson comorbidity index or the rate of mixed infections. Overall, 65.2% of patients achieved remission in the intervention group compared with only 18.2% in the control group (p < 0.001); 50% of re-infections in the intervention group even occurred after 36 months. Kaplan–Meier analysis showed that, compared with controls, the intervention group experienced significantly longer 3-year infection-free survival.
Conclusion
DAIR shows poor efficacy in difficult-to-treat cases, as demonstrated in our control group, which had a re-infection rate of 81.8%. In contrast, a DAIR group receiving topical calcium-based antibiotics showed significantly higher 3-year infection-free survival. Therefore, the combination of DAIR and degradable antibiogram-based local antibiotics is a reasonable salvage procedure for this body of patients. This is important as the number of severely sick patients who are too old for appropriate PJI treatment is estimated to increase significantly due to demographic change.




Similar content being viewed by others
References
Adams K, Couch L, Cierny G, Calhoun J, Mader JT (1992) In vitro and in vivo evaluation of antibiotic diffusion from antibiotic-impregnated polymethylmethacrylate beads. Clin Orthop Relat Res 278:244–252
Argenson JN, Arndt M, Babis G, Battenberg A, Budhiparama N, Catani F et al (2019) Hip and knee section, treatment, debridement and retention of implant: proceedings of international consensus on orthopedic infections. J Arthroplasty 34:S399–S419
Armstrong DG, Findlow AH, Oyibo SO, Boulton AJ (2001) The use of absorbable antibiotic-impregnated calcium sulphate pellets in the management of diabetic foot infections. Diabet Med 18:942–943
Blaha JD, Calhoun JH, Nelson CL, Henry SL, Seligson D, Esterhai JL Jr et al (1993) Comparison of the clinical efficacy and tolerance of gentamicin PMMA beads on surgical wire versus combined and systemic therapy for osteomyelitis. Clin Orthop Relat Res 295:8–12
Chang W, Colangeli M, Colangeli S, Di Bella C, Gozzi E, Donati D (2007) Adult osteomyelitis: debridement versus debridement plus Osteoset T pellets. Acta Orthop Belg 73:238–243
Chaussade H, Uckay I, Vuagnat A, Druon J, Gras G, Rosset P et al (2017) Antibiotic therapy duration for prosthetic joint infections treated by Debridement and Implant Retention (DAIR): similar long-term remission for 6 weeks as compared to 12 weeks. Int J Infect Dis 63:37–42
de Vries L, van der Weegen W, Neve WC, Das H, Ridwan BU, Steens J (2016) The effectiveness of debridement, antibiotics and irrigation for periprosthetic joint infections after primary hip and knee arthroplasty. A 15 years retrospective study in two community hospitals in The Netherlands. J Bone Jt Infect 1:20–24
Di Benedetto P, Di Benedetto ED, Salviato D, Beltrame A, Gissoni R, Cainero V et al (2017) Acute periprosthetic knee infection: is there still a role for DAIR? Acta Biomed 88:84–91
Faul F, Erdfelder E, Lang A-G, Buchner A (2007) G* Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39:175–191
Fehring KA, Abdel MP, Ollivier M, Mabry TM, Hanssen AD (2017) Repeat two-stage exchange arthroplasty for periprosthetic knee infection is dependent on host grade. J Bone Joint Surg Am 99:19–24
Ferguson JY, Dudareva M, Riley ND, Stubbs D, Atkins BL, McNally MA (2014) The use of a biodegradable antibiotic-loaded calcium sulphate carrier containing tobramycin for the treatment of chronic osteomyelitis: a series of 195 cases. Bone Joint J 96-B:829–836
Fleiter N, Walter G, Bosebeck H, Vogt S, Buchner H, Hirschberger W et al (2014) Clinical use and safety of a novel gentamicin-releasing resorbable bone graft substitute in the treatment of osteomyelitis/osteitis. Bone Joint Res 3:223–229
Gauland C (2011) Managing lower-extremity osteomyelitis locally with surgical debridement and synthetic calcium sulfate antibiotic tablets. Adv Skin Wound Care 24:515–523
Gehrke T, Parvizi J (2014) Proceedings of the international consensus meeting on periprosthetic joint infection. J Arthroplasty 29:4
GmbH Hereaus Medical (2016) Technical Monograph Herafill.In: Hereaus Medical Technical Monograph Herafill; 2016. http://heraeus-medical.com/de/produkte_1/knochenersatz/herafill_1.aspx. Accessed 15 Oct 2016
Gramlich Y, Walter G, Gils J, Hoffmann R (2017) Early results of adjuvant topical treatment of recurrent osteomyelitis with absorbable antibiotic carriers. Z Orthop Unfall 12:0042–112228
Gramlich Y, Walter G, Klug A, Harbering J, Kemmerer M, Hoffmann R (2019) Procedure for single-stage implant retention for chronic periprosthetic infection using topical degradable calcium-based antibiotics. Int Orthop 43(7):1559–1566
Heybeli N, Oktar FN, Ozyazgan S, Akkan G, Ozsoy S (2003) Low-cost antibiotic loaded systems for developing countries. Technol Health Care 11:207–216
Humm G, Noor S, Bridgeman P, David M, Bose D (2014) Adjuvant treatment of chronic osteomyelitis of the tibia following exogenous trauma using OSTEOSET((R))-T: a review of 21 patients in a regional trauma centre. Strat Trauma Limb Reconstr 9(3):157–161
Kallala R, Haddad FS (2015) Hypercalcaemia following the use of antibiotic-eluting absorbable calcium sulphate beads in revision arthroplasty for infection. Bone Joint J 97-B:1237–1241
Kamath AF, Ong KL, Lau E, Chan V, Vail TP, Rubash HE et al (2015) Quantifying the burden of revision total joint arthroplasty for periprosthetic infection. J Arthroplasty 30:1492–1497
Kelm J, Anagnostakos K, Regitz T, Schmitt E, Schneider G, Ahlhelm F (2004) MRSA-infections-treatment with intraoperatively produced gentamycin-vancomycin PMMA beads. Chirurg 75:988–995
Klemm K (1979) Gentamicin-PMMA-beads in treating bone and soft tissue infections (author’s transl). Zentralbl Chir 104:934–942
Klemm K, Borner M (1986) Treatment of chronic osteomyelitis with gentamicin PMMA chains. Unfallchirurgie 12:128–131
Kuiper JW, Willink RT, Moojen DJ, van den Bekerom MP, Colen S (2014) Treatment of acute periprosthetic infections with prosthesis retention: review of current concepts. World J Orthop 5:667–676
Kunutsor SK, Whitehouse MR, Lenguerrand E, Blom AW, Beswick AD (2016) Re-infection outcomes following one- and two-stage surgical revision of infected knee prosthesis: a systematic review and meta-analysis. PLoS ONE 11(3):e0151537
Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J (2012) Economic burden of periprosthetic joint infection in the United States. J Arthroplasty 27:61–65
Leite PS, Figueiredo S, Sousa R (2016) Prosthetic joint infection: report on the one versus two-stage exchange EBJIS survey. J Bone Jt Infect 1:1–6
Lora-Tamayo J, Senneville E, Ribera A, Bernard L, Dupon M, Zeller V et al (2017) The not-so-good prognosis of streptococcal periprosthetic joint infection managed by implant retention: the results of a large multicenter study. Clin Infect Dis 64:1742–1752
Mader JT, Calhoun J, Cobos J (1997) In vitro evaluation of antibiotic diffusion from antibiotic-impregnated biodegradable beads and polymethylmethacrylate beads. Antimicrob Agents Chemother 41:415–418
Maillet M, Pavese P, Bruley D, Seigneurin A, Francois P (2015) Is prosthesis retention effective for chronic infections in hip arthroplasties? A systematic literature review. Eur J Clin Microbiol Infect Dis 34:1495–1502
Marczak D, Synder M, Sibiński M, Okoń T, Kowalczewski J (2016) The use of calcium carbonate beads containing gentamicin in the second stage septic revision of total knee arthroplasty reduces reinfection rate. Knee 23(2):322–326
Mousset B, Benoit MA, Delloye C, Bouillet R, Gillard J (1995) Biodegradable implants for potential use in bone infection. An in vitro study of antibiotic-loaded calcium sulphate. Int Orthop 19:157–161
Nagra NS, Hamilton TW, Ganatra S, Murray DW, Pandit H (2016) One-stage versus two-stage exchange arthroplasty for infected total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 24:3106–3114
Nelson CL, Griffin FM, Harrison BH, Cooper RE (1992) In vitro elution characteristics of commercially and noncommercially prepared antibiotic PMMA beads. Clin Orthop Relat Res 284:303–309
Neut D, van de Belt H, Stokroos I, van Horn JR, van der Mei HC, Busscher HJ (2001) Biomaterial-associated infection of gentamicin-loaded PMMA beads in orthopaedic revision surgery. J Antimicrob Chemother 47:885–891
Osmon D, Berbari E, Berendt A, Lew D, Zimmerli W, Steckelberg J et al (2013) Infectious diseases society of a: diagnosis and management of prosthetic joint infection: clinical practice guidelines by the infectious diseases society of America. Clin Infect Dis 56:e1–e25
Ottesen CS, Troelsen A, Sandholdt H, Jacobsen S, Husted H, Gromov K (2019) Acceptable success rate in patients with periprosthetic knee joint infection treated with debridement, antibiotics, and implant retention. J Arthroplasty 34:365–368
Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ et al (2011) New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res 469(11):2992–2994
Peel TN, Dowsey MM, Buising KL, Liew D, Choong PF (2013) Cost analysis of debridement and retention for management of prosthetic joint infection. Clin Microbiol Infect 19:181–186
Qasim SN, Swann A, Ashford R (2017) The DAIR (debridement, antibiotics and implant retention) procedure for infected total knee replacement—a literature review. SICOT-J 3:2
Roger PM, Tabutin J, Blanc V, Leotard S, Brofferio P, Lecule F et al (2015) Prosthetic joint infection: a pluridisciplinary multi-center audit bridging quality of care and outcome. Med Mal Infect 45:229–236
Schinsky MF, Della Valle CJ, Sporer SM, Paprosky WG (2008) Perioperative testing for joint infection in patients undergoing revision total hip arthroplasty. J Bone Joint Surg Am 90:1869–1875
Sendi P, Lotscher PO, Kessler B, Graber P, Zimmerli W, Clauss M (2017) Debridement and implant retention in the management of hip periprosthetic joint infection: outcomes following guided and rapid treatment at a single centre. Bone Joint J 99(3):330–336
Sporer SM, Paprosky WG (2006) The use of a trabecular metal acetabular component and trabecular metal augment for severe acetabular defects. J Arthroplasty 21:83–86
Strauss A (1999) Lokaler Antibiotikumtraeger aus Kalziumsulfat: Vertraeglichkeit im Gewebe und Pharmakokinetik der angewendeten Antibiotika nach Implantation in Kaninchen. Köhler, Germany
Tice AD, Rehm SJ, Dalovisio JR, Bradley JS, Martinelli LP, Graham DR et al (2004) Practice guidelines for outpatient parenteral antimicrobial therapy. IDSA guidelines. Clin Infect Dis 38(12):1651–1671
Tsang SJ, Ting J, Simpson A, Gaston P (2017) Outcomes following debridement, antibiotics and implant retention in the management of periprosthetic infections of the hip: a review of cohort studies. Bone Joint J 99-B:1458–1466
Tschudin-Sutter S, Frei R, Dangel M, Jakob M, Balmelli C, Schaefer DJ et al (2016) Validation of a treatment algorithm for orthopaedic implant-related infections with device-retention-results from a prospective observational cohort study. Clin Microbiol Infect 22:457.e451–457.e459
Turner TM, Urban RM, Hall DJ, Chye PC, Segreti J, Gitelis S (2005) Local and systemic levels of tobramycin delivered from calcium sulfate bone graft substitute pellets. Clin Orthop Relat Res 437:97–104
Wahl P, Livio F, Jacobi M, Gautier E, Buclin T (2011) Systemic exposure to tobramycin after local antibiotic treatment with calcium sulphate as carrier material. Arch Orthop Trauma Surg 131:657–662
Wang J, Calhoun JH, Mader JT (2002) The application of bioimplants in the management of chronic osteomyelitis. Orthopedics 25:1247–1252
Waterman P, Melissa Barber M, Weintrob AC, Regina VanBrakle M, Howard R, Kozar MP et al (2012) The elution of colistimethate sodium from polymethylmethacrylate and calcium phosphate cement beads. Am J Orthop (Belle Mead NJ) 41(6):256–259
Webb JE, Schleck CD, Larson DR, Lewallen DG, Trousdale RT (2014) Mortality of elderly patients after two-stage reimplantation for total joint infection: a case-control study. J Arthroplasty 29:2206–2210
Wongworawat MD (2013) Clinical faceoff: one-versus two-stage exchange arthroplasty for prosthetic joint infections. Clin Orthop Relat Res 471:1750–1753
Yoon YC, Lakhotia D, Oh JK, Moon JG, Prashant K, Shon WY (2015) Is two-stage reimplantation effective for virulent pathogenic infection in a periprosthetic hip? A retrospective analysis. World J Orthop 6:712–718
Yu R, Hofstaetter JG, Sullivan T, Costi K, Howie DW, Solomon LB (2013) Validity and reliability of the paprosky acetabular defect classification. Clin Orthop Relat Res 471:2259–2265
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Ethical approval
The study was approved by the institutional review board (IRB Approval: LAEKH-FF-14-2018). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
167_2019_5627_MOESM1_ESM.pdf
Supplementary material 1 (PDF 38 kb) Supplementary Table: The Charlson comorbidity index. The table shows a full dataset relating to comorbidities for the intervention and control groups, and overall. There were no statistically significant differences between the two groups in terms of the Charlson comorbidity index.
Rights and permissions
About this article
Cite this article
Gramlich, Y., Johnson, T., Kemmerer, M. et al. Salvage procedure for chronic periprosthetic knee infection: the application of DAIR results in better remission rates and infection-free survivorship when used with topical degradable calcium-based antibiotics. Knee Surg Sports Traumatol Arthrosc 28, 2823–2834 (2020). https://doi.org/10.1007/s00167-019-05627-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05627-8