Abstract
Purpose
Limited evidence suggests that cross-education affords clinical benefits in the initial 8 weeks after anterior cruciate ligament (ACL) reconstruction, but it is unknown if such cross-education effects are reproducible and still present in later phases of rehabilitation. We examined whether cross-education, as an adjuvant to standard therapy, would accelerate the rehabilitation up to 26 weeks after ACL reconstruction by attenuating quadriceps weakness.
Methods
ACL-reconstructed patients were randomized into experimental (n = 22) and control groups (n = 21). Both groups received standard care after ACL reconstruction. In addition, the experimental group strength trained the quadriceps of the non-operated leg during weeks 1–12 after surgery (i.e., cross-education). Self-reported knee function was assessed with the Hughston Clinic Knee score as the primary outcome. Secondary outcomes were maximal quadriceps and hamstring strength and single leg hop distance. All outcomes were measured 29 ± 23 days prior to surgery, as a reference, and at 5-week, 12-week, and 26-week post-surgery.
Results
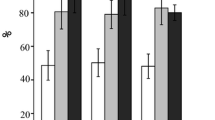
Both groups scored 12% worse on self-reported knee function 5-week post-surgery (95% CI 7–17) and showed 15% improvement 26-week post-surgery (95% CI − 20 to − 10). No cross-education effect was found. Interestingly, males scored 8–10% worse than females at each time point post-surgery. None of 33 secondary outcomes showed a cross-education effect. At 26-week post-surgery, both legs improved maximal quadriceps (5–14%) and hamstring strength (7–18%), and the non-injured leg improved 2% in hop distance. The ACL recovery was not affected by limb dominance and age.
Conclusion
26 weeks of standard care improved self-reported knee function and maximal leg strength relative to pre-surgery and adding cross-education did not further accelerate ACL recovery.
Level of evidence
I.
Clinical Trial Registry name and registration
This randomized controlled clinical trial is registered at the Dutch trial register (http://www.trialregister.nl) under NTR4395.

Similar content being viewed by others
References
Ageberg E, Zatterstrom R, Moritz U (1998) Stabilometry and one-leg hop test have high test–retest reliability. Scand J Med Sci Sports 8:198–202
American College of Sports Medicine (2009) American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc 41:687–708
Andrushko JW, Lanovaz JL, Bjorkman KM, Kontulainen SA, Farthing JP (2018) Unilateral strength training leads to muscle-specific sparing effects during opposite homologous limb immobilization. J Appl Physiol (1985) 124:866–876
Bennell K, Bartam S, Crossley K, Green S (2000) Outcome measures in patellofemoral pain syndrome: test retest reliability and inter-relationships. Phys Therapy Sport 1:32–41
Carroll TJ, Herbert RD, Munn J, Lee M, Gandevia SC (2006) Contralateral effects of unilateral strength training: evidence and possible mechanisms. J Appl Physiol 101:1514–1522
Chung KS, Ha JK, Yeom CH, Ra HJ, Lim JW, Kwon MS, Kim JG (2015) Are muscle strength and function of the uninjured lower limb weakened after anterior cruciate ligament injury? two-year follow-up after reconstruction. Am J Sports Med 43:3013–3021
de Valk EJ, Moen MH, Winters M, Bakker EW, Tamminga R, van der Hoeven H (2013) Preoperative patient and injury factors of successful rehabilitation after anterior cruciate ligament reconstruction with single-bundle techniques. Arthroscopy 29:1879–1895
Di Stasi S, Myer GD, Hewett TE (2013) Neuromuscular training to target deficits associated with second anterior cruciate ligament injury. J Orthop Sports Phys Ther 43:777–792 (A1–11)
Elias LJ, Bryden MP, Bulman-Fleming MB (1998) Footedness is a better predictor than is handedness of emotional lateralization. Neuropsychologia 36:37–43
Flandry F, Hunt JP, Terry GC, Hughston JC (1991) Analysis of subjective knee complaints using visual analog scales. Am J Sports Med 19:112–118
Gokeler A, Welling W, Benjaminse A, Lemmink K, Seil R, Zaffagnini S (2017) A critical analysis of limb symmetry indices of hop tests in athletes after anterior cruciate ligament reconstruction: a case control study. Orthop Traumatol Surg Res 103:947–951
Gokeler A, Welling W, Zaffagnini S, Seil R, Padua D (2017) Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 25:192–199
Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA (2016) Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med 50:804–808
Harput G, Kilinc HE, Ozer H, Baltaci G, Mattacola CG (2015) Quadriceps and hamstring strength recovery during early neuromuscular rehabilitation after ACL hamstring-tendon autograft reconstruction. J Sport Rehabil 24:398–404
Hoher J, Munster A, Klein J, Eypasch E, Tiling T (1995) Validation and application of a subjective knee questionnaire. Knee Surg Sports Traumatol Arthrosc 3:26–33
Hortobagyi T, Lambert NJ, Hill JP (1997) Greater cross education following training with muscle lengthening than shortening. Med Sci Sports Exerc 29:107–112
Lee DH, Lee JH, Jeong HJ, Lee SJ (2015) Serial changes in knee muscle strength after anterior cruciate ligament reconstruction using hamstring tendon autografts. Arthroscopy 31:890–895
Lepley AS, Gribble PA, Thomas AC, Tevald MA, Sohn DH, Pietrosimone BG (2015) Quadriceps neural alterations in anterior cruciate ligament reconstructed patients: a 6-month longitudinal investigation. Scand J Med Sci Sports 25:828–839
Magnus CR, Arnold CM, Johnston G, Dal-Bello Haas V, Basran J, Krentz JR, Farthing JP (2013) Cross-education for improving strength and mobility after distal radius fractures: a randomized controlled trial. Arch Phys Med Rehabil 94:1247–1255
Manca A, Dragone D, Dvir Z, Deriu F (2017) Cross-education of muscular strength following unilateral resistance training: a meta-analysis. Eur J Appl Physiol 117:2335–2354
Mohtadi NG, Chan DS, Dainty KN, Whelan DB (2011) Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev 9:CD005960
Myer GD, Ford KR, Barber Foss KD, Liu C, Nick TG, Hewett TE (2009) The relationship of hamstrings and quadriceps strength to anterior cruciate ligament injury in female athletes. Clin J Sport Med 19:3–8
Nakamura N, Horibe S, Sasaki S, Kitaguchi T, Tagami M, Mitsuoka T, Toritsuka Y, Hamada M, Shino K (2002) Evaluation of active knee flexion and hamstring strength after anterior cruciate ligament reconstruction using hamstring tendons. Arthroscopy 18:598–602
Nawasreh Z, Logerstedt D, Cummer K, Axe MJ, Risberg MA, Snyder-Mackler L (2017) Do patients failing return-to-activity criteria at 6 months after anterior cruciate ligament reconstruction continue demonstrating deficits at 2 years? Am J Sports Med 45:1037–1048
Palmieri-Smith RM, Thomas AC, Wojtys EM (2008) Maximizing quadriceps strength after ACL reconstruction. Clin Sports Med 27:405–424
Papandreou M, Billis E, Papathanasiou G, Spyropoulos P, Papaioannou N (2013) Cross-exercise on quadriceps deficit after ACL reconstruction. J Knee Surg 26:51–58
Papandreou MG, Billis EV, Antonogiannakis EM, Papaioannou NA (2009) Effect of cross exercise on quadriceps acceleration reaction time and subjective scores (Lysholm questionnaire) following anterior cruciate ligament reconstruction. J Orthop Surg Res 4:2 (799X-4-2)
Pearce AJ, Hendy A, Bowen WA, Kidgell DJ (2013) Corticospinal adaptations and strength maintenance in the immobilized arm following 3 weeks unilateral strength training. Scand J Med Sci Sports 23:740–748
Rabash J, Steele F, Brown W, Goldstein H (2009) A user’s guide to MLwiN, v. 2.10, 3rd edn. Center for Multilevel Modelling, University of Bristol, Bristol
Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR (2007) Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther 87:337–349
Ruddy KL, Carson RG (2013) Neural pathways mediating cross education of motor function. Front Hum Neurosci 7:397
Schmitt LC, Paterno MV, Hewett TE (2012) The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 42:750–759
Tan SH, Lau BP, Khin LW, Lingaraj K (2016) The importance of patient sex in the outcomes of anterior cruciate ligament reconstructions: a systematic review and meta-analysis. Am J Sports Med 44:242–254
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Thomee R, Kaplan Y, Kvist J, Myklebust G, Risberg MA, Theisen D, Tsepis E, Werner S, Wondrasch B, Witvrouw E (2011) Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 19:1798–1805
Toole AR, Ithurburn MP, Rauh MJ, Hewett TE, Paterno MV, Schmitt LC (2017) Young athletes cleared for sports participation after anterior cruciate ligament reconstruction: how many actually meet recommended return-to-sport criterion cutoffs? J Orthop Sports Phys Ther 47:825–833
Undheim MB, Cosgrave C, King E, Strike S, Marshall B, Falvey E, Franklyn-Miller A (2015) Isokinetic muscle strength and readiness to return to sport following anterior cruciate ligament reconstruction: is there an association? A systematic review and a protocol recommendation. Br J Sports Med 49:1305–1310
van Melick N, van Cingel RE, Brooijmans F, Neeter C, van Tienen T, Hullegie W, Nijhuis-van der Sanden MW (2016) Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med 50:1506–1515
Webster KE, Feller JA (2017) Younger patients and men achieve higher outcome scores than older patients and women after anterior cruciate ligament reconstruction. Clin Orthop Relat Res 475:2472–2480
Weinhandl JT, Earl-Boehm JE, Ebersole KT, Huddleston WE, Armstrong BS, O’Connor KM (2014) Reduced hamstring strength increases anterior cruciate ligament loading during anticipated sidestep cutting. Clin Biomech (Bristol Avon) 29:752–759
Welling W, Benjaminse A, Seil R, Lemmink K, Zaffagnini S, Gokeler A (2018) Low rates of patients meeting return to sport criteria 9 months after anterior cruciate ligament reconstruction: a prospective longitudinal study. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-4916-4
Zult T, Gokeler A, van Raay JJ, Brouwer RW, Zijdewind I, Hortobagyi T (2017) An anterior cruciate ligament injury does not affect the neuromuscular function of the non-injured leg except for dynamic balance and voluntary quadriceps activation. Knee Surg Sports Traumatol Arthrosc 25:172–183
Acknowledgements
The authors thank BSc. A. Doornbos, BSc. A. Elsinghorst, BSc. K. Koorenhof, and BSc. L. Winkelhorst for their assistance with the data collection, MSc. E. Nieman and MSc. I. Brookman for performing the pilot study, Dr. R. Stewart for his assistance with the statistical analysis, and Medisch Centrum Zuid-Flytta for providing the research facilities.
Funding
This work was supported by start-up fund 653013 from the University Medical Center Groningen, Groningen, The Netherlands.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report that no conflicts of interest have occurred that are associated with the current study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.

Rights and permissions
About this article
Cite this article
Zult, T., Gokeler, A., van Raay, J.J.A.M. et al. Cross-education does not improve early and late-phase rehabilitation outcomes after ACL reconstruction: a randomized controlled clinical trial. Knee Surg Sports Traumatol Arthrosc 27, 478–490 (2019). https://doi.org/10.1007/s00167-018-5116-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5116-y