Abstract
Purpose
Postoperative wound complication is a significant risk factor for subsequent deep periprosthetic joint infection after total knee arthroplasty (TKA). Central sensitization is an abnormal enhancement of pain mechanism involving the central nervous system. Although psychological disorder is widely considered as a risk factor, the relationship between central sensitization and wound complication is currently unclear. Therefore, the purpose of this study was to investigate whether central sensitization was associated with high wound complication rate after primary TKA.
Materials and methods
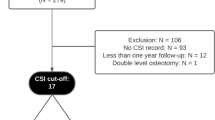
Between January and June 2016, 161 patients undergoing unilateral TKA were prospectively divided into two groups based on central sensitization inventory score of 40 points after excluding cases with known risk factors such as physical comorbidities, health-related behaviors, and psychological disorders. Group 1 consisted of 112 patients (112 knees) whose central sensitization inventory score was < 40 points and group 2 consisted of 49 patients (49 knees) whose central sensitization inventory score was ≥ 40 points. Wound complications were defined as wound dehiscence, suture granuloma, prolonged wound oozing after postoperative day 5, significant hematoma formation, or surgical site infection recorded during the initial 90-day postoperative period. Demographic data, visual analog scale (VAS), central sensitization inventory score, and wound complications were compared between the two groups.
Results
Wound complications developed in 3 (2.7%) knees in group 1 and 14 (28.6%) knees in group 2 (p < 0.001). Multivariate logistic regression analysis showed that the odds of postoperative wound complications were increased 15.7 times in patients with central sensitization inventory score ≥ 40 (95% CI 4.1–60.0, p < 0.001).
Conclusion
Central sensitization is a risk factor for the development of postoperative wound complication after primary TKA.
Level of evidence
II.


Similar content being viewed by others
References
Abdouh M, Storring JM, Riad M, Paquette Y, Albert PR, Drobetsky E, Kouassi E (2001) Transcriptional mechanisms for induction of 5-HT1A receptor mRNA and protein in activated B and T lymphocytes. J Biol Chem 276(6):4382–4388
Beilin B, Shavit Y, Trabekin E, Mordashev B, Mayburd E, Zeidel A, Bessler H (2003) The effects of postoperative pain management on immune response to surgery. Anesth Analg 97(3):822–827
Carroll K, Dowsey M, Choong P, Peel T (2014) Risk factors for superficial wound complications in hip and knee arthroplasty. Clin Microbiol Infect 20(2):130–135
Deleuran T, Vilstrup H, Overgaard S, Jepsen P (2015) Cirrhosis patients have increased risk of complications after hip or knee arthroplasty. Acta Orthop 86(1):108–113
Dennis DA (1997) Wound complications in total knee arthroplasty. Orthopedics 20(9):837–840
Eka A, Chen AF (2015) Patient-related medical risk factors for periprosthetic joint infection of the hip and knee. Ann Transl Med 3(16):233
Galat DD, McGovern SC, Larson DR, Harrington JR, Hanssen AD, Clarke HD (2009) Surgical treatment of early wound complications following primary total knee arthroplasty. J Bone Jt Surg Am 91(1):48–54
Garbedian S, Sternheim A, Backstein D (2011) Wound healing problems in total knee arthroplasty. Orthopedics 34(9):e516-518
Gosain A, DiPietro LA (2004) Aging and wound healing. World J Surg 28(3):321–326
Gosain A, Jones SB, Shankar R, Gamelli RL, DiPietro LA (2006) Norepinephrine modulates the inflammatory and proliferative phases of wound healing. J Trauma 60(4):736–744
Kim SH, Yoon KB, Yoon DM, Yoo JH, Ahn KR (2015) Influence of centrally mediated symptoms on postoperative pain in osteoarthritis patients undergoing total knee arthroplasty: a prospective observational evaluation. Pain Pract 15(6):E46–E53
Koh IJ, Kim TK, Chang CB, Cho HJ, In Y (2013) Trends in use of total knee arthroplasty in Korea from 2001 to 2010. Clin Orthop Relat Res 471(5):1441–1450
Kong L, Cao J, Zhang Y, Ding W, Shen Y (2017) Risk factors for periprosthetic joint infection following primary total hip or knee arthroplasty: a meta-analysis. Int Wound J 14(3):529–536
Latremoliere A, Woolf CJ (2009) Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain 10(9):895–926
Lee YC, Nassikas NJ, Clauw DJ (2011) The role of the central nervous system in the generation and maintenance of chronic pain in rheumatoid arthritis, osteoarthritis and fibromyalgia. Arthritis Res Ther 13(2):211
Lenz G, Goncalves D, Luo Z, Avruch J, Rodnight R, Neary JT (2001) Extracellular ATP stimulates an inhibitory pathway towards growth factor-induced cRaf-1 and MEKK activation in astrocyte cultures. J Neurochem 77(4):1001–1009
Lundblad H, Kreicbergs A, Jansson KA (2008) Prediction of persistent pain after total knee replacement for osteoarthritis. J Bone Jt Surg Br 90(2):166–171
Malinin A, Oshrine B, Serebruany V (2004) Treatment with selective serotonin reuptake inhibitors for enhancing wound healing. Med Hypotheses 63(1):103–109
Mann DA, Oakley F (2013) Serotonin paracrine signaling in tissue fibrosis. Biochimica et Biophysica Acta (BBA) Mol Basis Dis 1832(7):905–910
Martinez V, Fletcher D, Bouhassira D, Sessler DI, Chauvin M (2007) The evolution of primary hyperalgesia in orthopedic surgery: quantitative sensory testing and clinical evaluation before and after total knee arthroplasty. Anesth Analg 105(3):815–821
Mayer TG, Neblett R, Cohen H, Howard KJ, Choi YH, Williams MJ, Perez Y, Gatchel RJ (2012) The development and psychometric validation of the central sensitization inventory. Pain Pract 12(4):276–285
McGuire L, Heffner K, Glaser R, Needleman B, Malarkey W, Dickinson S, Lemeshow S, Cook C, Muscarella P, Melvin WS, Ellison EC, Kiecolt-Glaser JK (2006) Pain and wound healing in surgical patients. Ann Behav Med 31(2):165–172
Murphy SL, Lyden AK, Phillips K, Clauw DJ, Williams DA (2011) Association between pain, radiographic severity, and centrally-mediated symptoms in women with knee osteoarthritis. Arthritis Care Res (Hoboken) 63(11):1543–1549
Neblett R, Cohen H, Choi Y, Hartzell MM, Williams M, Mayer TG, Gatchel RJ (2013) The central sensitization inventory (CSI): establishing clinically significant values for identifying central sensitivity syndromes in an outpatient chronic pain sample. J Pain 14(5):438–445
Panni AS, Vasso M, Cerciello S, Salgarello M (2011) Wound complications in total knee arthroplasty. Which flap is to be used? With or without retention of prosthesis? Knee Surg Sports Traumatol Arthrosc 19(7):1060–1068
Pugely AJ, Martin CT, Gao Y, Schweizer ML, Callaghan JJ (2015) The incidence of and risk factors for 30-day surgical site infections following primary and revision total joint arthroplasty. J Arthroplasty 30(9 Suppl):47–50
Ridgeway S, Wilson J, Charlet A, Kafatos G, Pearson A, Coello R (2005) Infection of the surgical site after arthroplasty of the hip. J Bone Jt Surg Br 87(6):844–850
Shih LY, Cheng CY, Chang CH, Hsu KY, Hsu RW, Shih HN (2004) Total knee arthroplasty in patients with liver cirrhosis. J Bone Jt Surg Am 86-a(2):335–341
Soga F, Katoh N, Inoue T, Kishimoto S (2007) Serotonin activates human monocytes and prevents apoptosis. J Investig Dermatol 127(8):1947–1955
Swift ME, Burns AL, Gray KL, DiPietro LA (2001) Age-related alterations in the inflammatory response to dermal injury. J Investig Dermatol 117(5):1027–1035
Vince K, Chivas D, Droll KP (2007) Wound complications after total knee arthroplasty. J Arthroplasty 22(4 Suppl 1):39–44
Voscopoulos C, Lema M (2010) When does acute pain become chronic? Br J Anaesth 105(Suppl 1):i69–i85
Woolf CJ (2011) Central sensitization: implications for the diagnosis and treatment of pain. Pain 152(3 Suppl):S2–S15
Wu C, Qu X, Liu F, Li H, Mao Y, Zhu Z (2014) Risk factors for periprosthetic joint infection after total hip arthroplasty and total knee arthroplasty in Chinese patients. PLoS One 9(4):e95300
Zhu Y, Zhang F, Chen W, Liu S, Zhang Q, Zhang Y (2015) Risk factors for periprosthetic joint infection after total joint arthroplasty: a systematic review and meta-analysis. J Hosp Infect 89(2):82–89
Acknowledgements
There was no external funding source in this investigation.
Disclaimer
There are no financial remuneration of any authors and any members of their family.
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Kim, M.S., Koh, I.J., Lee, S.Y. et al. Central sensitization is a risk factor for wound complications after primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 26, 3419–3428 (2018). https://doi.org/10.1007/s00167-018-4914-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4914-6