Abstract
Purpose
The arthrotomy techniques of knee surgery may cause varying degrees of disruption to the tissue blood supply. The aim of this study was to investigate the effects of the medial parapatellar (MPPa), midvastus (MVa), subvastus (SVa) and lateral parapatellar (LPPa) approaches on regional tissue perfusion of the knee.
Methods
In this experimental study, a total of 28 female rabbits were applied with four different arthrotomy techniques as Group MPPa, Group MVa, Group SVa and Group LPPa. The blood supply of the tissue around the knee was examined by scintigraphic imaging including the perfusion reserve and T max, and biochemical alteration of the oxidative stress parameters including malondialdehyde (MDA), fluorescent oxidation products (FlOPs), and histopathological findings were evaluated on tissue samples after 3 weeks.
Results
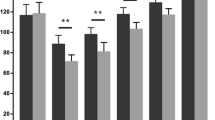
The perfusion reserve was increased in all four groups compared to the healthy, contralateral knees. In the Group LPPa, the vascularity was significantly increased compared to the Group MPPa (p = 0.006). In the examination of biochemical parameters, the increase in MDA levels was statistically significant in the Group MPPa compared with the Group LPPa (p = 0.004), and in the Group MVa compared with the Group LPPa (p = 0.006). The increase in the value of MDA levels was striking in the Group MPPa and Group MVa compared with the control group (p = 0.004, p = 0.004, respectively). The increase in another oxidative stress parameter, the tissue FlOPs levels, was statistically significant in the Group MPPa compared with the control group (p = 0.035).
Conclusion
The LPPa and SVa caused less oxidative stress and less disruption of the muscle blood supply, in biochemical and scintigraphic parameters, compared to the MPPa and MVa. Therefore, in clinical practice, the SVa is preferable to the MPPa and MVa in total knee arthroplasty and the LPPa should be preferred more frequently in selected cases with critical soft tissue viability.




Similar content being viewed by others
References
Amin AM, Nawito ZO, Atfy RA, El-Hadidi KT (2012) Tc99m sestamibi lower extremity muscle scan, is it a useful screening tool for assessment of preclinical atherosclerosis in rheumatoid arthritis patients? Rheumatol Int 32:2075–2081
Avcı CC, Gülabi D, Erdem M, Kurnaz R, Güneş T, Bostan B (2013) Minimal invasive midvastus versus standard parapatellar approach in total knee arthroplasty. Acta Orthop Traumatol Turc 47:1–7
Brick GW, Scott RD (1989) Blood supply to the patella. Significance in total knee arthroplasty. J Arthroplasty 4 Suppl:75–79
Bourke MG, Sclavos EK, Jull GA, Buttrum PJ, Russell TG, Dalton PA (2012) A comparison of patellar vascularity between the medial parapatellar and subvastus approaches in total knee arthroplasty. J Arthroplasty 27(6):1123–1127
Brochado Neto FC, Gonzalez J, Cinelli M Jr, Albers M (2000) Bypass to the genicular arteries for revascularisation of the lower limb. Eur J Vasc Endovasc Surg 20(6):545–549
Celen YZ, Zincirkeser S, Akdemir I, Yilmaz M (2000) Investigation of perfusion reserve using 99Tc(m)-MIBI in the lower limbs of diabetic patients. Nucl Med Commun 21:817–822
Cila E, Güzel V, Ozalay M, Tan J, Simşek SA, Kanatli U, Oztürk A (2002) Subvastus versus medial parapatellar approach in total knee arthroplasty. Arch Orthop Trauma Surg 122:65–68
Dines JS, Weber L, Razzano P, Prajapati R, Timmer M, Bowman S, Bonasser L, Dines DM, Grande DP (2007) The effect of growth differentiation factor-5-coated sutures on tendon repair in a rat model. J Shoulder Elbow Surg 16:S215–S221
Dutka J, Skowronek M, Sosin P, Skowronek P (2011) Subvastus and medial parapatellar approaches in TKA: comparison of functional results. Orthopedics 34(6):148
Engh GA, Holt BT, Parks NL (1997) A midvastus muscle-splitting approach for total knee arthroplasty. J Arthroplasty 12(3):322–331
Erdem M, Bostan B, Güneş T, Özkan F, Sen C, Özyurt H, Köseoğlu RD, Erdoğan H (2010) Protective effects of melatonin on ischemia-reperfusion injury of skeletal muscle. Eklem Hastalik Cerrahisi 21:166–171
Gunst S, Villa V, Magnussen R, Servien E, Lustig S, Neyret P (2016) Equivalent results of medial and lateral parapatellar approach for total knee arthroplasty in mild valgus deformities. Int Orthop 40:945–951
Heekin RD, Fokin AA (2014) Mini-midvastus versus mini-medial parapatellar approach for minimally invasive total knee arthroplasty: outcomes pendulum is at equilibrium. J Arthroplasty 29:339–342
Hemert WL, Senden R, Grimm B, Linde MJ, Lataster A, Heyligers IC (2011) Early functional outcome after subvastus or parapatellar approach in knee arthroplasty is comparable. Knee Surg Sports Traumatol Arthrosc 19:943–951
Hempfing A, Schoeniger R, Koch PP, Bischel O, Thomsen M (2007) Patellar blood flow during knee arthroplasty surgical exposure: intraoperative monitoring by laser doppler flowmetry. J Orthop Res 25(10):1389–1394
Hofmann AA, Plaster RL, Murdock LE (1991) Subvastus (Southern) approach for primary total knee arthroplasty. Clin Orthop Relat Res 269:70–77
Järvinen M (1975) Healing of a crush injury in rat striated muscle. 2. A histological study of the effect of early mobilization and immobilization on the repair processes. Acta Pathol Microbiol Scand A 83(3):269–282
Jung YB, Lee YS, Lee EY, Jung HJ, Nam CH (2009) Comparison of the modified subvastus and medial parapatellar approaches in total knee arthroplasty. Int Orthop 33(2):419–423
Kayler DE, Lyttle D (1998) Surgical interruption of patellar blood supply by total knee arthroplasty. Clin Orthop Relat Res 229:221–227
Koca K, Yurttas Y, Cayci T, Bilgic S, Kaldirim U, Durusu M, Cekli Y, OzkanH Hanci V, Purtuloglu T, Akgul EO, Oguz E, Yildiz C, Basbozkurt M (2011) The role of preconditioning and N-acetylcysteine on oxidative stress resulting from tourniquet-induced ischemia-reperfusion in arthroscopic knee surgery. J Trauma 70:717–723
Kohl S, Evangelopoulos DS, Hartel M, Kohlhof H, Roeder C, Eggli S (2011) Anterior knee pain after total knee arthroplasty: does it correlate with patellar blood flow? Knee Surg Sports Traumatol Arthrosc 19(9):1453–1459
Layher F, Zipfel M, Sander K, Matziolis G, Roth A (2016) Functional comparison of the outcome after midvastus and medial parapatellar surgical approach in total knee arthroplasty. Z Orthop Unfall 154(1):50–57
Lazaro LE, Wellman DS, Klinger CE, Dyke JP, Pardee NC, Sculco PK, Berkes MB, Helfet DL, Lorich DG (2013) Quantitative and qualitative assessment of bone perfusion and arterial contributions in a patellar fracture model using gadolinium-enhanced magnetic resonance imaging: a cadaveric study. J Bone Joint Surg Am 95(19):e1401–e1407
Lazaro LE, Cross MB, Lorich DG (2014) Vascular anatomy of the patella: implications for total knee arthroplasty surgical approaches. Knee 21(3):655–660
Lin SY, Chen CH, Fu YC, Huang PJ, Lu CC, Su JY, Chang JK, Huang HT (2013) Comparison of the clinical and radiological outcomes of three minimally invasive techniques for total knee replacement at two years. Bone Joint J. 95-B(7):906–910
Liu HW, Gu WD, Xu NW, Sun JY (2014) Surgical approaches in total knee arthroplasty: a meta-analysis comparing the midvastus and subvastus to the medial peripatellar approach. J Arthroplasty 29:2298–2304
Manevska N, Gjorceva DP, Ahmeti I, Todorovska L, Stojanoski S, Kocovska MZ (2016) Tissue-muscle perfusion scintigraphy of the lower limbs in a patient with Type 2 diabetes mellitus and peripheral arterial disease. Mol Imaging Radionucl Ther 25:42–46
Roysam GS, Oakley MJ (2001) Subvastus approach for total knee arthroplasty: a prospective, randomized, and observer-blinded trial. J Arthroplasty 16(4):454–457
Sanna M, Sanna C, Caputo F, Piu G, Salvi M (2013) Surgical approaches in total knee arthroplasty. Joints 1:34–44
Sarikaya I, Aygit AC, Candan L, Sarikaya A, Türkyilmaz M, Berkarda S (2000) Assessment of tissue viability after frostbite injury by technetium-99m-sestamibi scintigraphy in an experimental rabbit model. Eur J Nucl Med 27:41–50
Sedlak J, Lindsay RH (1968) Estimation of total, protein-bound, and nonprotein sulfhydryl groups in tissue with Ellman’s reagent. Anal Biochem 25:192–205
Shukla R, Mahajan P, Singh M, Jain RK, Kumar R (2017) Outcome of total knee replacement via two approaches in Indian scenario. J Knee Surg 30(2):174–178
Soslowsky LJ, Thomopoulos S, Tun S, Flanagan CL, Keefer CC, Mastaw J, Carpenter JE (2000) Neer Award 1999. Overuse activity injures the supraspinatus tendon in an animal model: a histologic and biomechanical study. J Shoulder Elbow Surg 9(2):79–84
Thienpont E (2013) Faster quadriceps recovery with the far medial subvastus approach in minimally invasive total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21(10):2370–2374
Toms AD, Mandalia V, Haigh R, Hopwood B (2009) The management of patients with painful total knee replacement. J Bone Joint Surg Br 91:143–150
Top H, Sarikaya A, Aygit AC, Benlier E, Kiyak M (2006) Review of monitoring free muscle flap transfers in reconstructive surgery: role of 99mTc sestamibi scintigraphy. Nucl Med Commun 27:91–98
Wallace CD, Amiel D (1991) Vascular assessment of the periarticular ligaments of the rabbit knee. J Orthop Res 9(6):787–791
Wasowicz W, Neve J, Peretz A (1993) Optimized steps in fluorometric determination of thiobarbituric acid-reactive substances in serum: importance of extraction ph and influence of sample preservation and storage. Clin Chem 39:2522–2526
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Confict of interest
The authors have no competing interests to declare.
Funding
This study was funded by Turkish Society of Orthopaedics and Traumatology (TSOT)- Turkish Ortopedik Araştırma Konseyi (TOAK).
Ethical approval
All procedures performed in study involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted.
Rights and permissions
About this article
Cite this article
Koçak, A., Özmeriç, A., Koca, G. et al. Lateral parapatellar and subvastus approaches are superior to the medial parapatellar approach in terms of soft tissue perfusion. Knee Surg Sports Traumatol Arthrosc 26, 1681–1690 (2018). https://doi.org/10.1007/s00167-017-4690-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4690-8