Abstract
Purpose
Patients are sometimes admitted to intensive care units (ICU) after elective noncardiac surgery for advanced monitoring and treatments not available on a general postsurgical ward. However, patterns of ICU utilization are poorly understood. Our aims were to assess the incidence and determinants of ICU utilization after elective noncardiac surgical procedures.
Methods
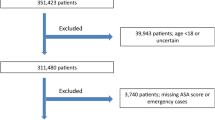
Population-based cohort study included adult patients who underwent 13 types of major elective noncardiac surgical procedures between 2006 and 2014 in Ontario, Canada. Primary outcome was early admission to ICU within 24 h after surgery. A prespecified analysis using multilevel logistic regression modeling separately examined patient- and hospital-level factors associated with early ICU admission within distinct groups of surgical procedures.
Results
Early ICU admission occurred in 9.6% of the included 541,524 patients. Patients admitted early to ICU showed higher median age (68 vs. 65 years), burden of prehospital comorbidities (Charlson comorbidity index score ≥ 2, 33.1 vs. 10.4%), 30-day mortality rates (2.4 vs. 0.3%), and longer median postoperative hospital stays (6 vs. 4 days) than patients admitted to a ward. There was wide variation in proportions of patients admitted early to ICU across different surgery types (0.9% for hysterectomy to 90.8% for open abdominal aortic aneurysm repair) with generally low 30-day mortality across procedures (0.1–2.8%). Within individual procedures, there was wide interhospital variation in the range of early ICU admission rates (hysterectomy 0.07–14.4%, lower gastrointestinal resection 1.3–95%, endovascular aortic aneurysm 1.3–95.2%). The individual hospital where surgery was performed accounted for a large proportion of the variation in early ICU admission rates, with the median odds ratio ranging from 2.3 for hysterectomy to 21.5 for endovascular aortic aneurysm.
Conclusions
There is a wide variation in early ICU admission across and within surgical procedures. The individual hospital accounts for a large proportion of this variation. Further research is required to identify the basis for this variation and to develop better methods for allocating ICU resources for postoperative management of surgical patients.

Similar content being viewed by others
References
Weiser TG, Haynes AB, Molina G, Lipsitz SR, Esquivel MM, Uribe-Leitz T, Fu R, Azad T, Chao TE, Berry WR, Gawande AA (2015) Estimate of the global volume of surgery in 2012: an assessment supporting improved health outcomes. Lancet 385:S11
Gillies MA, Harrison EM, Pearse RM, Garrioch S, Haddow C, Smyth L, Parks R, Walsh TS, Lone NI (2017) Intensive care utilization and outcomes after high-risk surgery in Scotland: a population-based cohort study. Br J Anaesth 118:123–131
Biccard BM, Madiba TE, South African Surgical Outcomes Study Investigators (2015) The South African Surgical Outcomes Study: a 7-day prospective observational cohort study. S Afr Med J 105:465
Pearse RM, Moreno RP, Bauer P, Pelosi P, Metnitz P, Spies C, Vallet B, Vincent J-L, Hoeft A, Rhodes A (2012) Mortality after surgery in Europe: a 7 day cohort study. Lancet 380:1059–1065
Canadian Institute for Health Information (CIHI). Care in Canadian ICUs. August 2016
Wunsch H, Gershengorn HB, Cooke CR, Guerra C, Angus DC, Rowe JW, Li G (2016) Use of intensive care services for medicare beneficiaries undergoing major surgical procedures. Anesthesiology 124:899–907
Kahan BC, Koulenti D, Arvaniti K, Beavis V, Campbell D, Chan M, Moreno R, Pearse RM, International Surgical Outcomes Study Group (2017) Critical care admission following elective surgery was not associated with survival benefit: prospective analysis of data from 27 countries. Intensive Care Med 43:971–979
Gillies MA, Pearse RM (2016) Intensive care after high-risk surgery: what’s in a name? Anesthesiology 124:761–762
Ghaffar S, Pearse RM, Gillies MA (2017) ICU admission after surgery: who benefits? Curr Opin Crit Care 23:424–429
Gillies MA, Power GS, Harrison DA, Fleming A, Cook B, Walsh TS, Pearse RM, Rowan KM (2015) Regional variation in critical care provision and outcome after high-risk surgery. Intensive Care Med 41:1809–1816
Wunsch H, Angus DC, Harrison DA, Collange O, Fowler R, Hoste EA, de Keizer NF, Kersten A, Linde-Zwirble WT, Sandiumenge A, Rowan KM (2008) Variation in critical care services across North America and Western Europe. Crit Care Med 36(2787–2793):e2781–e2789
Wunsch H, Angus DC, Harrison DA, Linde-Zwirble WT, Rowan KM (2011) Comparison of medical admissions to intensive care units in the United States and United Kingdom. Am J Respir Crit Care Med 183:1666–1673
International Surgical Outcomes Study Group (2016) Global patient outcomes after elective surgery: prospective cohort study in 27 low-, middle- and high-income countries. Br J Anaesth 117:601–609
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudanal studies: development and validation. J Chron Dis 40:373–383
Charlson ME, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245–1251
Hux JE, Ivis F, Flintoft V, Bica A (2002) Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care 25:512–516
Tu K, Campbell NRC, Chen Z, Cauch-Dudek KJ, McAlister FA (2007) Accuracy of administrative databases in identifying patients with hypertension. Open Med 1:E18–E26
Gershon AS, Wang C, Guan J, Vasilevska-Ristovska J, Cicutto L, To T (2009) Identifying individuals with physician diagnosed COPD in health administrative databases. Copd 6:388–394
Quan H, Khan N, Hemmelgarn BR, Tu K, Chen G, Campbell N, Hill MD, Ghali WA, McAlister FA (2009) Validation of a case definition to define hypertension using administrative data. Hypertension 54:1423–1428
Garland A, Yogendran M, Olafson K, Scales DC, McGowan KL, Fransoo R (2012) The accuracy of administrative data for identifying the presence and timing of admission to intensive care units in a Canadian province. Med Care 50:e1–e6
Scales DC, Guan J, Martin CM, Redelmeier DA (2006) Administrative data accurately identified intensive care unit admissions in Ontario. J Clin Epidemiol 59:802–807
Juurlink D, Preyra C, Croxford R, Chong A, Austin P (2006) Canadian Institute for health information discharge abstract database: a validation study. ICES investigative report, Toronto
Canadian Institute for Health Information (CIHI). CIHI data quality study of the 2009–2010. Discharge Abstract Database. Revised June 2012
Mukaka MM (2012) Statistics corner: a guide to appropriate use of correlation coefficient in medical research. Malawi Med J 24:69–71
Harrell FE Jr (2015) Regression modeling strategies. Springer, Cham
Austin PC, Merlo J (2017) Intermediate and advanced topics in multilevel logistic regression analysis. Stat Med 36:3257–3277
Austin PC, Steyerberg EW (2014) Graphical assessment of internal and external calibration of logistic regression models by using loess smoothers. Stat Med 33:517–535
Admon AJ, Wunsch H, Iwashyna TJ, Cooke CR (2017) Hospital contributions to variability in the use of ICUs among elderly Medicare recipients. Crit Care Med 45:75–84
Gershengorn HB, Iwashyna TJ, Cooke CR, Scales DC, Kahn JM, Wunsch H (2012) Variation in use of intensive care for adults with diabetic ketoacidosis. Crit Care Med 40:2009–2015
Chen R, Strait KM, Dharmarajan K, Li SX, Ranasinghe I, Martin J, Fazel R, Masoudi FA, Cooke CR, Nallamothu BK, Krumholz HM (2015) Hospital variation in admission to intensive care units for patients with acute myocardial infarction. Am Heart J 170:1161–1169
Gershengorn HB, Garland A, Gong MN (2015) Patterns of daily costs differ for medical and surgical intensive care unit patients. Ann Am Thorac Soc 12:1831–1836
Sjoding MW, Prescott HC, Wunsch H, Iwashyna TJ, Cooke CR (2015) Hospitals with the highest intensive care utilization provide lower quality pneumonia care to the elderly. Crit Care Med 43:1178–1186
Valley TS, Sjoding MW, Ryan AM, Iwashyna TJ, Cooke CR (2015) Association of intensive care unit admission with mortality among older patients with pneumonia. JAMA 314:1272–1279
Acknowledgements
This study was supported by a grant from the Academic Health Science Centre Alternative Funding Plan (AHSC AFP) Innovation Fund. DNW is supported in part by a New Investigator Award from the Canadian Institutes of Health Research. HW and DNW are supported in part by Merit Awards from the Department of Anesthesia at the University of Toronto. AL holds a Canada Research Chair in Health Policy and Citizen Engagement. PCA is supported by a Career Investigator Award from the Heart and Stroke Foundation.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jerath, A., Laupacis, A., Austin, P.C. et al. Intensive care utilization following major noncardiac surgical procedures in Ontario, Canada: a population-based study. Intensive Care Med 44, 1427–1435 (2018). https://doi.org/10.1007/s00134-018-5330-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-018-5330-6